11.9 Gastroesophageal Reflux Disease
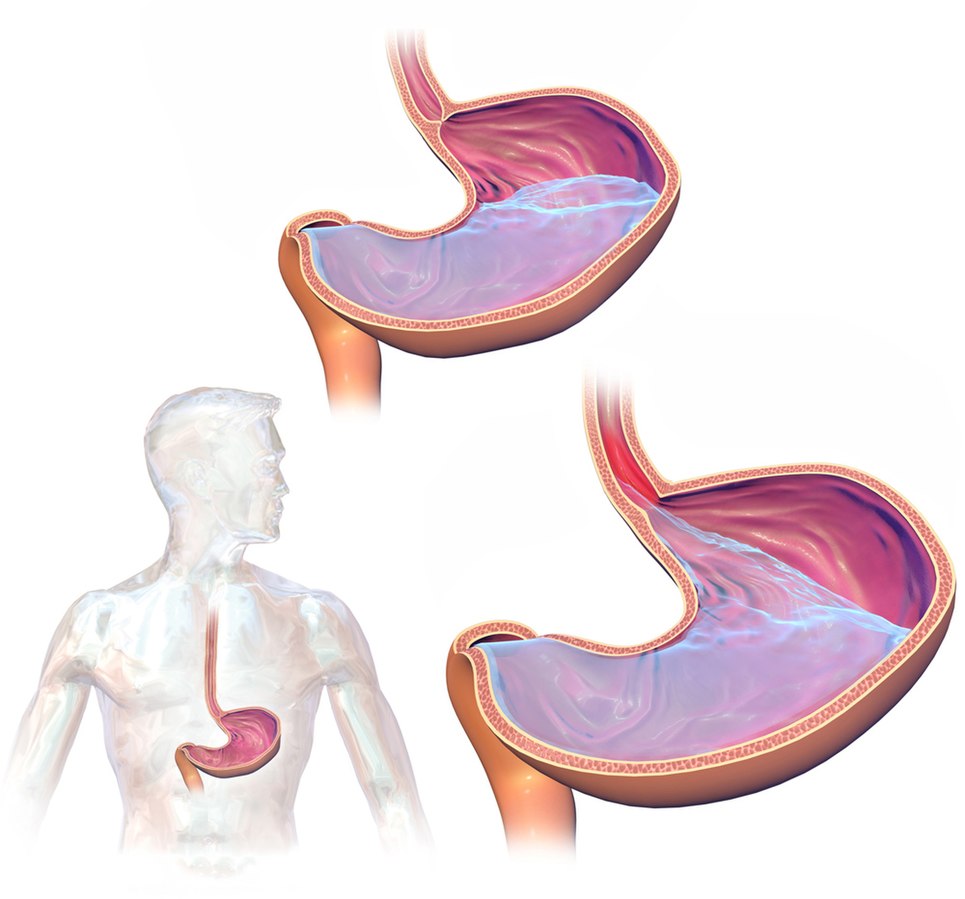
Gastroesophageal reflux disease (GERD) occurs when stomach contents flow backwards into the esophagus. GERD is a common, chronic disorder that develops in about 20% of adults in the United States.[1] Please see Figure 11.30[2] for an image of what occurs with GERD.
GERD can be classified into three different types, based on whether or not damage is occurring to the esophagus: nonerosive reflux disease (no damage to the esophagus), erosive esophagitis (formation of ulcers or erosions in the esophagus), and Barrett’s esophagus. Barrett’s esophagus is further described in the “Pathophysiology” subsection.[3]
Common risk factors for the development of GERD include the following[4]:
- Poor muscle tone in the lower esophageal sphincter
- Hiatal hernia
- Slow gastric contents emptying
- Obesity
- Hiatal hernia
- Age over 50 years old
- Tobacco usage
- Excessive alcohol use
- Pregnancy
- Low socioeconomic status
- Medications such as calcium channel blockers, anticholinergics, benzodiazepines, NSAIDs/aspirin, some antidepressants, albuterol, and nitroglycerin
Pathophysiology
There are several abnormalities that can cause GERD, such as impaired lower esophageal sphincter (LES) tone, the presence of a hiatal hernia, impaired esophageal mucosa, and altered esophageal peristalsis.[5]
The LES is a ring of smooth muscle located between the esophagus and stomach to prevent backward flow of stomach contents. In clients who do not have GERD, the LES is a high-pressure area that only opens when food is present, allowing food to flow to enter the lower pressure area of the stomach. However, in clients with GERD, the LES may inappropriately relax, allowing stomach contents to flow backwards into the esophagus.[6]
A hiatal hernia is a condition in which the upper part of the stomach abnormally bulges through the hiatus of the diaphragm. When there is laxity in this hiatus, gastric content can back up into the esophagus.[7] Read more about hiatal hernias in the “Hernia” section of this chapter.
Esophageal mucosa normally functions as a protective defensive barrier against acid gastric contents, but with repeated exposure to stomach contents (which are highly acidic), the mucosa can become damaged. Clients with chronic GERD can develop Barrett’s esophagus. Chronic exposure to acidic stomach contents causes squamous epithelial cells that line the esophagus to transition into columnar epithelium, also known as Barrett’s epithelium. Barrett’s epithelium is more resistant to acid exposure but can become cancerous. Therefore, Barrett’s esophagus is considered a precancerous condition that is closely monitored.[8],[9]
Normally, the acidic gastric contents that enter the esophagus are cleared by frequent esophageal peristalsis and neutralized by salivary bicarbonate. Clients with GERD may have impaired esophageal peristalsis, leading to decreased clearance of gastric contents, resulting in reflux symptoms and mucosal damage.[10]
Assessment
Physical Exam
The most common symptoms of GERD are heartburn and regurgitation of gastric contents. Heartburn is defined as a retrosternal burning sensation or discomfort that may radiate into the neck and typically occurs after the ingestion of meals or when in a reclined position. Regurgitation refers to backwards flow of acidic gastric contents into the esophagus or mouth. Clients may also have difficult or painful swallowing, nausea, epigastric area pain, and increased belching. Some clients have atypical symptoms of GERD such as chest pain, persistent coughing, new-onset asthma, laryngitis, dental cavities, or a hoarse voice.[11]
Common Laboratory and Diagnostic Tests
GERD is typically diagnosed based on clinical signs and symptoms or by trialing a proton pump inhibitor (PPI) medication to determine if symptoms improve with treatment. In clients with significant symptoms, such as difficult or painful swallowing, reduced red blood counts, hematemesis, or unintended weight loss, an esophagogastroduodenoscopy (EGD) may be performed to rule out complications of GERD such as erosions, Barrett’s esophagus, narrowing of the esophagus (caused by scar tissue formation), and esophageal cancer.[12] To review information on an EGD, please visit the “Common Laboratory and/or Diagnostic Tests” subsection of the “General Assessment of the Gastrointestinal System.”
In clients with GERD whose symptoms do not respond to medications, health care providers may order ambulatory esophageal reflux monitoring. This test entails inserting a catheter into the client’s nose with the distal tip near the LES. The catheter is used to monitor acid levels at the LES and help link the occurrence of symptoms with the presence of high acid levels.[13]
Nursing Diagnoses
Nursing priorities for those suffering from GERD include symptom management, lifestyle changes, dietary education, and preventing complications.
Nursing diagnoses for clients with GERD are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Common nursing diagnoses for clients diagnosed with GERD are as follows[14],[15],[16]:
- Acute Pain
- Deficient Knowledge
- Imbalanced Nutrition: Less than Body Requirements
- Impaired Tissue Integrity
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes include the following:
- The client will rate their pain at 3 or less on a scale of 0 to 10 within 24 hours.
- The client will verbalize three lifestyle modifications that will help reduce the prevalence of GERD symptoms after the teaching session.
- The client will achieve a weight within a healthy range appropriate for their height within six months.
- The client will verbalize the importance of medication adherence to prevent complications by the end of the teaching session.
Interventions
Medical Interventions
Medical treatment for GERD can be categorized as lifestyle changes, medication therapy, and surgical management.[17]
Lifestyle Changes
Lifestyle changes are typically the first step for treating GERD. The client is taught to stop consuming food three hours before bed and to elevate the head of the bed if possible. Clients are also taught to modify their diet to reduce GERD symptoms. Although there is some disagreement on the necessities of eliminating certain foods, clients are typically taught to avoid chocolate, caffeine, coffee, heavily spiced foods, foods with high citrus content, and carbonated beverages. If the client is obese, weight loss is encouraged.[18]
Medications
If lifestyle changes do not effectively manage GERD symptoms, medications are prescribed. Commonly prescribed classes of medications are proton pump inhibitors (PPIs), histamine 2 receptor antagonists (H2RAs), and prokinetics. PPIs are considered the gold standard of medical treatment for GERD due to their effectiveness in treating both nonerosive and erosive GERD. Some PPIs and H2RAs are available as over-the-counter medications, and some require a prescription. Prokinetic medications help promote esophageal peristalsis. Although some clients may benefit from prokinetic medications like metoclopramide, their use is controversial due to the side effects that can occur with long-term use.[19]
For more information about medications used to treat GERD, visit the “Antiulcer Medications” and “Antiemetics” sections in the “Gastrointestinal System” chapter in Open RN Nursing Pharmacology, 2e.
Surgical Management
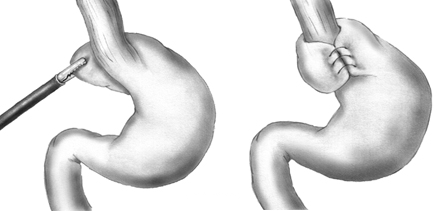
If GERD does not respond to typical medication therapy or unacceptable side effects occur, surgery may be an option, especially if a large hiatal hernia is present. The most common surgical procedure for GERD is a laparoscopic Nissen fundoplication. In this procedure, the upper portion of the stomach is wrapped around the lower portion of the esophagus to prevent the reflux of gastric contents into the esophagus. See Figure 11.31[20] for an illustration of the laparoscopic Nissen fundoplication procedure. Common postoperative complications are abdominal bloating, difficulty swallowing, and increased burping, although most clients experience an improvement in GERD symptoms.[21],[22]
View a supplementary YouTube video[23] on surgery used to treat GERD: Anti-reflux surgery, fundoplication-Mayo Clinic.
Nursing Interventions
When providing nursing care to clients with GERD, the following nursing interventions can be categorized as nursing assessments, nursing actions, and client teaching[24],[25]:
Nursing Assessments
- Assess the client’s nutritional status because it can be impacted by GERD symptoms and avoidance of triggering foods.
- Perform a comprehensive assessment of chest pain symptoms because the pain caused by GERD can be similar to symptoms of a myocardial infarction, especially in female clients.
- Assess for signs and symptoms of aspiration caused by GERD (i.e., wheezing, new onset asthma, chronic cough, and hoarseness).
- Assess complete blood count results for signs of anemia as a result of erosive GERD. Cardiac labs may be ordered by the health care provider to rule out a myocardial infarction when atypical chest pain is present.
Nursing Actions
- Obesity can increase GERD symptoms, so weight loss is encouraged. A typical goal is to lose one pound per week until a desired weight is achieved. The client can also be referred to a dietician to help develop a healthy eating plan. Gastric bypass surgery is an option for severely obese clients with GERD.
- Small, frequent meals are encouraged instead of large meals because they are easier to digest and may reduce GERD symptoms.
- Administer prescribed GERD medications.
- Elevate the head of bed of clients in inpatient care to prevent GERD symptoms and decrease the risk of aspiration.
Client Teaching
The following topics are typically included when providing health teaching about GERD:
- Understand the GERD disease process and medications prescribed to manage the condition.
- Sit upright during and after meals.
- Avoid eating three hours before bedtime and elevate the head of the bed using boards or other devices.
- Follow dietary restrictions to help manage symptoms.
- Monitor the stool and vomit for the presence of blood because this can indicate erosive GERD.
- Encourage smoking cessation and avoidance of alcohol because these symptoms can cause increased production of acid, as well as relaxation of the LES, leading to increased GERD symptoms.
- Avoid bending over, coughing, and straining with bowel movements, as these actions can raise intra-abdominal pressure and increase reflux.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
View a supplementary YouTube video[26] on GERD: Treatments for Heartburn | Gastroesophageal Reflux Disease (GERD) | Gastrointestinal Society.
View a supplementary video[27] on GERD and hiatal hernias: Heartburn and hiatal hernia.
![]() RN Recap: GERD
RN Recap: GERD
View a brief YouTube video overview of GERD[28]:
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- “GastroEsophageal_Reflux_Disease_(GERD).jpg” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Khieu, M., & Mukherjee, S. (2024). Barrett Esophagus. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430979/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Curran, A. (2023). GERD nursing diagnosis and nursing care plan. https://nursestudy.net/gerd-nursing-diagnosis/ ↵
- Vera, M. (2023). 8 gastroesophageal reflux disease (GERD) nursing care plans. https://nurseslabs.com/gastroesophageal-reflux-disease-gerd-nursing-care-plans/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- “Nissen_fundoplication.png” by Xopusmagnumx at English Wikipedia is in the Public Domain. ↵
- Antunes, C., Aleem, A., & Curtis, S. A. (2023). Gastroesophageal Reflux Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441938/ ↵
- Cleveland Clinic. (n.d.). Nissen fundoplication. https://my.clevelandclinic.org/health/treatments/4200-nissen-fundoplication ↵
- Mayo Clinic. (2010, April 22). Anti-reflux surgery, fundoplication-Mayo Clinic [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=X840-6PyO4c ↵
- Curran, A. (2023). GERD nursing diagnosis and nursing care plan. https://nursestudy.net/gerd-nursing-diagnosis/ ↵
- Vera, M. (2023). 8 gastroesophageal reflux disease (GERD) nursing care plans. https://nurseslabs.com/gastroesophageal-reflux-disease-gerd-nursing-care-plans/ ↵
- Gastrointestinal Society. (2017, October 24). Treatments for heartburn | Gastroesophageal reflux disease (GERD) | Gastrointestinal Society [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=wzdb4x0rAE4 ↵
- Mayo Clinic. (n.d.). Heartburn and hiatal hernia [Video]. Unknown platform. All rights reserved. https://www.mayoclinic.org/diseases-conditions/heartburn/multimedia/heartburn-gerd/vid-20084644 ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 11 - GERD [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/DEq57OCB0L4?si=6g2xwVjRO-s_zXsP ↵
When stomach contents flow backwards into the esophagus.
Clients with chronic GERD whose esophagus is exposed to acidic stomach content and causes changes in the squamous epithelial cells that line the esophagus and transition into columnar epithelium.
Retrosternal burning sensation or discomfort that may radiate into the neck and typically occurs after the ingestion of meals or when in a reclined position.
Backwards flow of acidic gastric contents into the esophagus or mouth.

