8.12 Benign Prostate Hypertrophy
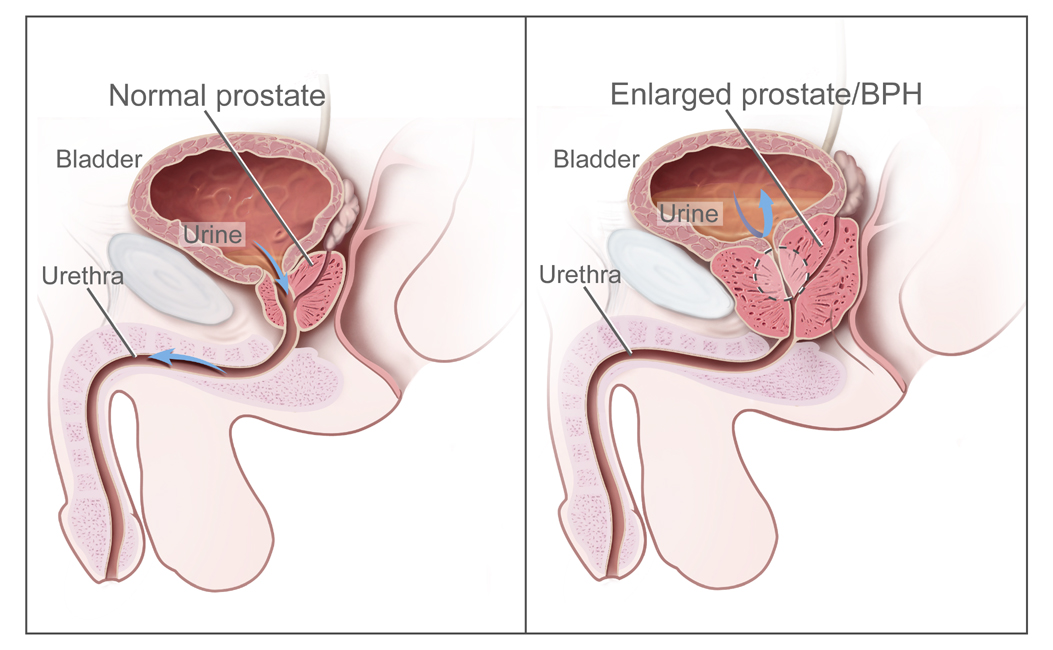
Benign prostatic hyperplasia (BPH) refers to enlargement of the prostate that is not cancerous. See Figure 8.16[1] for an illustration of BPH.
Pathophysiology
BPH is a common condition in males aged 50 and older. During BPH, the enlarged prostate presses against the urethra, causing it to narrow. Eventually, the bladder becomes weak from trying to pass urine through the narrowed urethra. It loses its ability to completely empty, leaving some urine in the bladder called urinary retention.[2]
Assessment
The inability to completely empty the bladder causes many of the symptoms associated with BPH, such as a frequent and intense urge to urinate, urinating frequently at night, difficulty starting a urine stream or a weak stream, and a sensation that the bladder has not emptied completely. If urinary retention is not adequately addressed, it can cause complications such as urinary tract infections, bladder damage, and kidney damage.[3]
The American Urological Association Symptom Index/International Prostate Symptom Score can be used to measure the severity of BPH symptoms.
View the American Urological Association Symptom Index/International Prostate Symptom Score on the MDCalc website.
Diagnostic Testing
A health care provider may order several types of diagnostic tests to diagnose BPH, such as prostate specific antigen blood test, urodynamic flow testing, voiding cystourethrogram, or a cystoscopy:
- Prostate specific antigen (PSA): The PSA test measures the level of prostate-specific antigen in the blood, a protein produced by normal, as well as malignant, cells of the prostate gland. BPH can cause elevated PSA levels.[4]
- Digital rectal exam: A digital rectal exam is commonly performed to identify abnormalities such as bumps or hardened spots on the prostate.
- Urodynamic flow testing: A procedure that looks at how well the bladder, sphincters, and urethra are storing and releasing urine. Most urodynamic tests focus on the bladder’s ability to hold urine and empty steadily and completely. Urodynamic tests can also show whether the bladder is having involuntary contractions that cause urine leakage.[5]
- Voiding cystourethrogram: X-ray technology called fluoroscopy visualizes the urinary tract and bladder to examine the size, shape, and direction of urine flow. A thin, flexible tube called a catheter is inserted into the urethra and passed into the bladder by a urologist. Contrast dye flows through the catheter into the bladder. X-rays are taken from various angles while the bladder is full of contrast dye, and then the catheter is removed, and X-rays are taken as the client empties their bladder.
- Cystoscopy: During a cystoscopy, the urologist can see signs of blockage, such as an enlarged prostate gland. Read more information about cystoscopy under “Diagnostic Testing” in the “General Urinary System Assessment” section.
Nursing Diagnoses
Nursing problems and diagnoses for clients with BPH focus on managing urinary retention and preventing urinary tract infection. Common diagnoses include the following:
- Impaired Urinary Elimination
- Urinary Retention
- Risk for Infection
- Disturbed Sleep Pattern
- Readiness for Enhanced Knowledge
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Examples of expected outcomes for clients with BPH are as follows:
- The client will verbalize three methods to manage urinary retention by the end of the teaching session.
- By the end of the teaching session, the client will verbalize symptoms of urinary tract infection to promptly report to the health care provider.
- The client will remain free from urinary tract injury caused by urinary retention.
Interventions
Medical Interventions
BPH may be treated with lifestyle changes, medications, or transurethral procedures.
Lifestyle Modifications
Health care providers may recommend lifestyle changes for men whose BPH symptoms are mild to help manage the symptoms. Lifestyle modifications include the following[6]:
- Reducing intake of liquids, particularly before going out in public or before sleeping
- Avoiding or reducing intake of caffeinated beverages and alcohol
- Avoiding medications such as decongestants, antihistamines, antidepressants, and diuretics that can worsen symptoms
- Training the bladder to hold more urine for longer periods
- Trying to urinate a second time after voiding to fully empty the bladder, referred to as double voiding
- Pelvic floor muscle exercises
- Preventing or treating constipation
Medication Therapy
Medications may be prescribed to stop the growth of the prostate, shrink it, or reduce symptoms associated with BPH[7]:
- Alpha-blockers: Alpha-blockers relax the smooth muscles of the prostate and bladder neck to improve urine flow and reduce bladder blockage. Examples include tamsulosin, doxazosin, prazosin, and terazosin.
- 5-alpha reductase inhibitors: These medications block the production of DHT, which accumulates in the prostate and may cause prostate growth. Examples include dutasteride and finasteride.
- Combination therapy: Research indicates combining two classes of medications can more effectively improve symptoms, urinary flow, and quality of life. Examples of combination medications include finasteride and doxazosin or dutasteride and tamsulosin. Alpha-blockers and antimuscarinics may also be prescribed for overactive bladder symptoms, where the bladder muscles contract uncontrollably causing urinary frequency, urinary urgency, and urinary incontinence. Antimuscarinics are a class of medications that relax the bladder muscles.
- Phosphodiesterase inhibitors: Although commonly prescribed for erectile dysfunction, this medication is also used to relax smooth muscles in the lower urinary tract to improve urine flow. An example of this medication is tadalafil.
Minimally Invasive Procedures
Minimally invasive procedures may be performed by urologists to relieve BPH symptoms when medications are ineffective. These procedures use the transurethral method, which involves inserting a catheter or cystoscope through the urethra to destroy enlarged prostate tissue or widen the urethra. This can help relieve blockage and urinary retention caused by benign prostatic hyperplasia. Minimally invasive procedures include the following[8]:
- Transurethral needle ablation: Uses heat generated by radiofrequency energy to destroy selected portions of prostate tissue.
- Transurethral microwave thermotherapy: Uses heat generated by microwave to destroy selected prostate tissue.
- High-intensity focused ultrasound: Uses heat generated by ultrasound waves to destroy enlarged prostate tissue.
- Transurethral electrovaporization: Electric current vaporizes selected prostate tissue and seals blood vessels, which reduces the risk of bleeding.
- Water-induced thermotherapy: Uses heated water to destroy selected prostate tissue.
- Prostatic stent insertion: A small device called a prostatic stent is passed through the urethra to the area narrowed by the enlarged prostate. Once in place, the stent expands like a spring, and it pushes back the prostate tissue, widening the urethra.
If a patient is not a surgical candidate, intermittent catheterization or a chronic Foley may be utilized.
Surgery
Surgery may be performed when symptoms are severe, other treatments haven’t helped, or a complication has developed such as bladder damage. Surgeries remove part or all of the prostate or make cuts in the prostate to take pressure off the urethra. Although removing enlarged prostate tissue relieves many BPH symptoms, it does not cure BPH. Surgeries to remove enlarged prostate tissue include the following[9]:
- Transurethral resection of the prostate (TURP): TURP is considered the gold standard for treating blockage of the urethra due to BPH and is the most common type of surgery performed. A resectoscope is passed through the urethra to reach the prostate and cuts pieces of enlarged prostate tissue with a wire loop. Special fluid carries the tissue pieces into the bladder, where it is flushed out at the end of the procedure.
- Transurethral incision of the prostate (TUIP): A cystoscope and an instrument that uses an electric current or a laser beam are inserted through the urethra to reach the prostate where it makes a few small cuts in the prostate and in the bladder neck to widen the urethra.
- Laser surgery: A cystoscope is used to pass a laser fiber through the urethra into the prostate where it destroys the enlarged tissue. The risk of bleeding is lower than in TURP and TUIP because the laser seals blood vessels as it cuts through the prostate tissue.
- Open prostatectomy: An incision is made through the skin to reach the prostate where part or all of it is removed through the incision. This surgery is used when the prostate is greatly enlarged, complications occur, or the bladder is damaged and needs repair. Open prostatectomy requires general anesthesia, a longer hospital stay than other surgical procedures for benign prostatic hyperplasia, and a longer rehabilitation period.
Postoperative Concerns
After surgery is performed, the prostate, urethra, and surrounding tissues may be irritated and swollen, causing urinary retention. To prevent urinary retention, the urologist typically inserts an indwelling (Foley) catheter after the procedure so urine can drain freely out of the bladder. Sometimes, the indwelling catheter causes recurring, painful, difficult-to-control bladder spasms the day after surgery. Medications, such as oxybutynin, may be prescribed to relax bladder muscles and prevent bladder spasms.[10]
Potential postoperative complications include the following[11]:
- Problems urinating: Painful urination, difficulty urinating, urinary frequency, urgency, or retention may occur after surgery but will gradually lessen. After a couple of months, urination will be easier and less frequent.
- Urinary incontinence: As the bladder returns to normal after surgery, clients may have temporary problems controlling their urination, resulting in incontinence. The longer their urinary problems existed before surgery, the longer it takes for the bladder to regain its full function after surgery.
- Bleeding: After surgery, the prostate or tissues around it may bleed, and blood or blood clots may appear in urine. Some bleeding is normal and should clear up within several days. However, the surgeon should be notified if the urine contains large clots, it is so red it is difficult to see through, or the client is experiencing pain.
- Deep vein thrombosis: Blood clots from BPH surgery can pass into the bloodstream and lodge in other parts of the body, most often the legs. The surgeon should be promptly notified of calf pain or unilateral leg warmth and swelling.
- Infection: Anesthesia used during surgery may cause urinary retention and increase the risk of a urinary tract infection (UTI). An indwelling catheter also increases the risk of a UTI. The health care provider should be promptly notified of UTI symptoms for the prescription of antibiotics.
- Scar tissue: Scar tissue may form in the urethra and cause it to narrow for up to one year after surgery, which may require additional surgery.
- Sexual dysfunction: Some men may experience temporary problems with sexual function after BPH surgery. The length of time for restored sexual function depends on the type of surgery performed and how long symptoms were present before surgery.
Nursing Interventions
Health Teaching
Nurses reinforce lifestyle modifications to help manage BPH symptoms. Nurses teach clients about signs and symptoms of urinary tract infections and urinary retention. If medications are prescribed, nurses ensure the client understands the purpose of the medications and potential side effects. For example, clients taking alpha-blockers are instructed that dizziness may occur and to change positions slowly because of potential orthostatic blood pressure changes. Clients should also be instructed regarding therapeutic onset of medication therapy and that symptom improvement may take time to achieve.
Postoperative Care
In addition to monitoring for potential postoperative complications that were previously described under the “Surgery” subsection, nurses also perform urinary catheter care and monitor urine output.
If the client had a TURP procedure, continuous bladder irrigation is typically prescribed to decrease blood clots in the bladder and maintain the flow and patency of urine after surgery. The nurse titrates the flow of saline into the bladder to keep the urine light pink to clear. Maintaining accurate urinary output records is an important part of CBI intervention. The nurse should ensure that the total urine output is calculated to account for the volume of saline instilled. A large-size drainage bag should be utilized to collect the urine and irrigation fluids due to the high volume being instilled and drained.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Benign Prostate Hypertrophy
RN Recap: Benign Prostate Hypertrophy
View a brief YouTube video[12] overview on Benign Prostate Hypertrophy:
- “Benign_Prostatic_Hyperplasia_nci-vol-7137-300.jpg” by unknown author for National Cancer Institute is licensed in the Public Domain. ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2022, Aug. 17]. Enlarged prostate (BPH); [cited 2023, Oct. 10]. https://medlineplus.gov/enlargedprostatebph.html ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2022, Aug. 17]. Enlarged prostate (BPH); [cited 2023, Oct. 10]. https://medlineplus.gov/enlargedprostatebph.html ↵
- National Cancer Institute. (2022, March 11). Prostate-specific antigen (PSA) test. https://www.cancer.gov/types/prostate/psa-fact-sheet ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021, September). Urodynamic testing. National Institutes of Health. https://www.niddk.nih.gov/health-information/diagnostic-tests/urodynamic-testing ↵
- National Institute of Diabetes and Digestive and Kidney Disease. (2014, September). Prostate enlargement (benign prostatic hyperplasia). National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#complications ↵
- National Institute of Diabetes and Digestive and Kidney Disease. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#complications ↵
- National Institute of Diabetes and Digestive and Kidney Disease. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#complications ↵
- National Institute of Diabetes and Digestive and Kidney Disease. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#complications ↵
- National Institute of Diabetes and Digestive and Kidney Disease. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#complications ↵
- National Institute of Diabetes and Digestive and Kidney Disease. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#complications ↵
- Open RN Project. (2024, April 24).Health Alterations - Chapter 8 Renal and Urinary Disease - Benign Prostatic Hypertrophy.[Video]. YouTube. CC BY-NC 4.0 https://youtu.be/_DV0O6AVL0g ↵
Enlargement of the prostate that is not cancerous.
Inability of the bladder to completely empty leaving some urine in the bladder.

