11.8 Diverticulitis
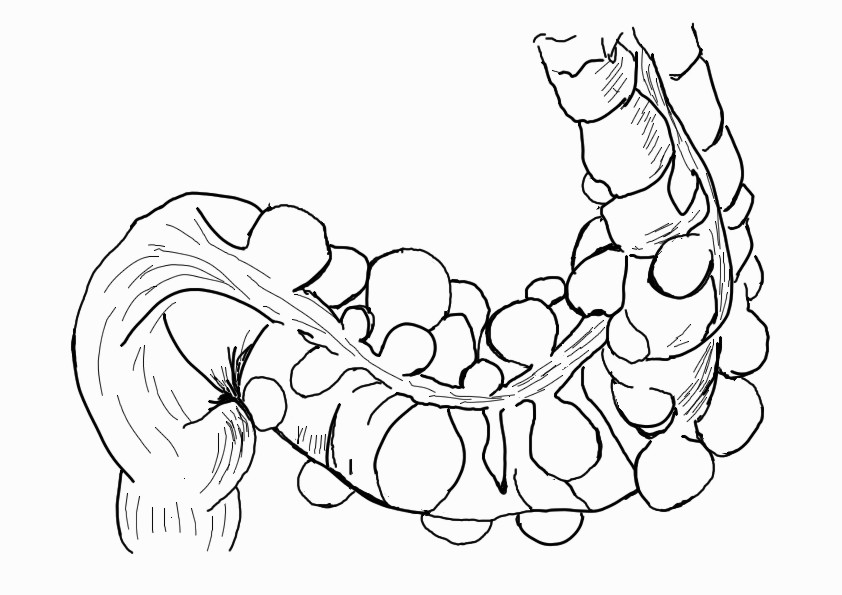
A diverticulum is an out-pouching of the wall of the colon. The presence of many diverticula is known as diverticulosis. Clients with diverticulosis are generally asymptomatic, but a small percentage develop diverticulitis, inflammation of a diverticulum.[1],[2] See Figure 11.28[3] for an image of a colon with diverticulosis.
Diverticulitis can be complicated or uncomplicated. Uncomplicated diverticulitis means there is inflammation with no complications present. Complicated diverticulitis refers to diverticulitis associated with an abscess, perforation, fistula (an abnormal connection between two organs), or a bowel blockage.[4],[5]
Risk factors for diverticulosis and diverticulitis are the same, with the main risk factors being dietary intake. Clients with low-fiber intake or high intake of red meat and fatty foods are at increased risk for developing diverticulosis and diverticulitis. Other risk factors include obesity, tobacco usage, certain medications (NSAIDs, steroids, opioids and statins), and age, with 60% of clients aged 60 or older having diverticulosis.[6],[7]
Pathophysiology
Diverticula form where the walls of the colon are weak. This weakness occurs due to increased pressures in the colon or a result of connective tissue disorders. Constipation and the straining that occurs during bowel movements can play a role in diverticula forming due to the increased pressure within the colon.[8],[9],[10]
Obstruction from hardened stool or food eroding the wall of the diverticula causes inflammation and necrosis of the diverticulum, which lead to the perforation. Perforation can cause diverticulitis, which can also lead to formation of an abscess, fistula, or bowel obstruction. Major perforations can cause peritonitis.[11],[12],[13]
Assessment
Physical Exam
Clients with diverticulosis are often asymptomatic. However, blood may be present in the stool because diverticula bleed easily.
Clients with diverticulitis commonly present with abdominal pain, typically in the left lower quadrant. Clients may also experience altered bowel habits such as diarrhea or constipation. Fever, nausea, and vomiting may also be present.
When completing a physical exam, if an abscess is present, the provider may be able to palpate a mass. Bowel sounds are commonly hypoactive.
Common Laboratory and Diagnostic Tests
Lab Tests
Labs tests ordered to diagnose diverticulitis are a complete blood count and inflammatory markers[14],[15]:
- Complete blood count (CBC) will often show elevated white blood cells.
- Inflammatory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are often elevated during diverticulitis.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Diagnostic Testing
Imaging modalities used to diagnose diverticulosis and diverticulitis are CT scan, abdominal ultrasound, and colonoscopy[16],[17]:
- A CT scan of the abdomen with contrast is considered the gold standard for diagnosing diverticulitis.
- An abdominal ultrasound can also be used to diagnose diverticulitis with almost as much sensitivity as a CT scan and is more cost-effective.
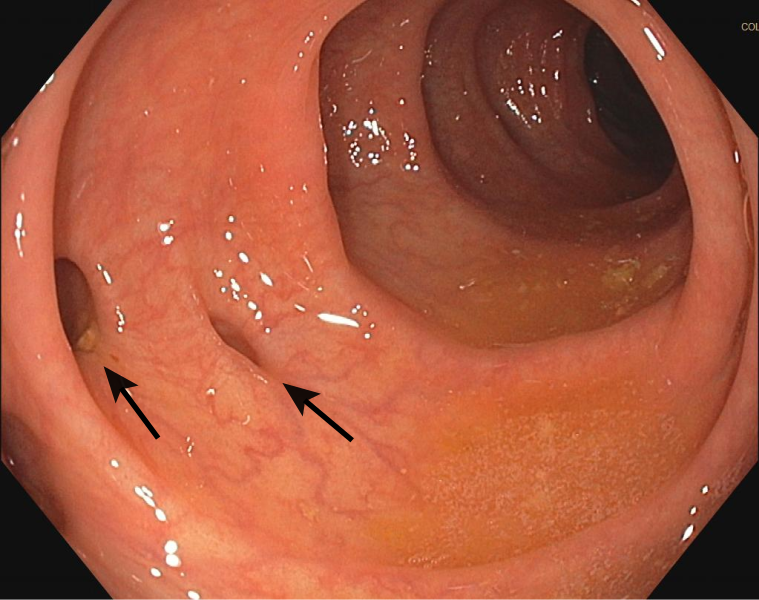
- Although a colonoscopy is routinely used to diagnose diverticulosis, it should not be performed during suspected diverticulitis because it can cause perforation of the colon. Clients with diverticulitis are typically encouraged to undergo a colonoscopy six to eight weeks after their diverticulitis symptoms have improved. See Figure 11.29[18] for an image showing two diverticula that were discovered via colonoscopy.
Nursing Diagnoses
Nursing priorities for clients with diverticulitis include managing pain, ensuring adequate nutritional intake, and optimizing stool consistency.
Nursing diagnoses for clients with diverticulitis are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Possible nursing diagnoses for those with diverticulitis are as follows[19],[20]:
- Acute Pain
- Imbalanced Nutrition: Less than Body Requirements
- Constipation
- Diarrhea
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes for some of the above nursing diagnoses include the following[21]:
- The client will rate their pain at 3 or less on a scale of 0 to 10 within two hours.
- The client will maintain their weight within a healthy range that is appropriate for their height until the next follow-up appointment.
- The client will pass bowel movements without straining within three days.
- The client will pass formed stools in a nonurgent manner until the next follow-up appointment.
Interventions
Medical Interventions
Depending on the severity of the case of diverticulitis, the client may require inpatient care. Client characteristics that may require hospitalization include extreme vomiting, those who cannot take liquids by mouth, older adults, those who are immunocompromised, or those with signs of complications.
Regardless of the setting, treatment for diverticulitis consists of bowel rest, increased fluids, and antibiotics. Initially, hospitalized clients will have nothing by mouth (NPO) diet orders, whereas those undergoing outpatient treatment may be on a clear liquid diet. Fluids should be increased by mouth. In the inpatient setting intravenous fluids may be administered. Oral antibiotics are prescribed for those in the outpatient setting, and intravenous antibiotics are administered for hospitalized clients. Pain management may also be necessary depending on the comfort level of the client.[22],[23]
Surgery may be required for clients who develop an abscess, fistula, perforation, bowel obstruction, or other complication. Clients who experience recurring bouts of diverticulitis may require surgery to remove diseased portion(s) of the colon.[24],[25]
Nursing Interventions
When providing nursing care to clients with diverticulitis, nursing interventions can be divided into the following: nursing assessments, nursing actions, and client teaching[26],[27]:
Nursing Assessments
- Assess the client’s vitals and pain level on a 0-10 scale, as changes in vitals and/or the quality of their pain can indicate a complication is occurring.
- Assess the client’s intake and output, including stool characteristics.
- Monitor lab results, such as white blood cell count.
Nursing Actions
- Administer prescribed antibiotics, IV fluids, and pain medications.
- If surgery is required, complete a preoperative checklist. Review preoperative checklists and preparing a client for surgery in the “Perioperative Care” chapter.
- Collaborate with a dietician to help optimize nutrition.
Client Teaching
- After the acute phase of diverticulitis has passed, teach the client to consume a diet that is rich in fiber to prevent constipation that can cause more diverticula. However, during the acute phase of diverticulitis, fiber-rich foods should be avoided because they increase GI motility in a time when bowel rest is desired.
- Reinforce increased fluid intake (2.5-3 liters per day) to prevent hard stools and straining.
- Encourage weight loss, if indicated, because of the association between obesity and diverticulitis.
- Teach the client to avoid anything that can increase intra-abdominal pressure (such as straining with bowel movements and heavy lifting) because this can lead to the formation of more diverticula. During the acute phase, this pressure can also increase pain.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
View a supplementary YouTube video[28] on diverticulitis: Diverticulitis, causes, signs and symptoms, diagnosis and treatment.
![]() RN Recap: Diverticulitis
RN Recap: Diverticulitis
View a brief YouTube video overview of diverticulitis[29]:
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- “Sigmoid_diverticulum_(diagram).jpg” by Anpol42 is licensed under CC BY-SA 4.0 ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- Cleveland Clinic. (n.d.). Diverticulosis. https://my.clevelandclinic.org/health/diseases/24883-diverticulosis ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- Cleveland Clinic. (n.d.). Diverticulosis. https://my.clevelandclinic.org/health/diseases/24883-diverticulosis ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Nallapeta, N. S., Farooq, U., & Patel, K. (2023). Diverticulosis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430771/ ↵
- “Diverticulosis_(two_diverticula)_01.svg” by Jmarchn is licensed under CC BY-SA 3.0 ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Wagner, M. (2023). Diverticulitis: Nursing diagnoses, care plans, assessment & interventions. https://www.nursetogether.com/diverticulitis-nursing-diagnosis-care-plan/ ↵
- Wagner, M. (2023). Diverticulitis: Nursing diagnoses, care plans, assessment & interventions. https://www.nursetogether.com/diverticulitis-nursing-diagnosis-care-plan/ ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Wagner, M. (2023). Diverticulitis: Nursing diagnoses, care plans, assessment & interventions. https://www.nursetogether.com/diverticulitis-nursing-diagnosis-care-plan/ ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Wagner, M. (2023). Diverticulitis: Nursing diagnoses, care plans, assessment & interventions. https://www.nursetogether.com/diverticulitis-nursing-diagnosis-care-plan/ ↵
- Linzay, C. D., & Pandit, S. (2023). Acute Diverticulitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459316/ ↵
- Wagner, M. (2023). Diverticulitis: Nursing diagnoses, care plans, assessment & interventions. https://www.nursetogether.com/diverticulitis-nursing-diagnosis-care-plan/ ↵
- Medical Centric. (2021, March 9). Diverticulitis, causes, signs and symptoms, diagnosis and treatment [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=k_9Gbn0TBz0 ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 11 - Diverticulitis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/F8lTgfp_de0?si=Qkr-KpnLEpA6rnyZ ↵
A small, bulging pouch that can form in the lining of the colon.
The condition of having diverticula in the colon.
Inflammation or infection of one or more diverticula in the digestive tract.
An abnormal connection between two organs.

