6.7 Pneumonia
Pathophysiology
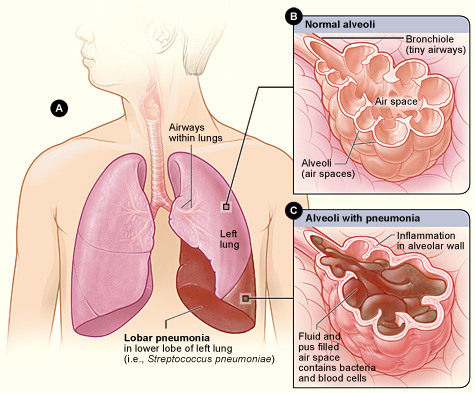
Pneumonia is a common respiratory infection that can affect people of all ages. It is characterized by inflammation and infection within the alveoli, causing them to fill with fluid or purulent material, resulting in a productive cough, fever, chills, and difficulty breathing. Pneumonia differs from chronic conditions like asthma and COPD in that it is an acute infection. Pneumonia can range in seriousness from mild to life-threatening. It is most serious for infants and young children, people older than age 65, and people with chronic health problems like COPD or weakened immune systems.[1],[2]
Pneumonia can be caused by a variety of microorganisms, including bacteria, viruses, and fungi. Common bacteria that cause pneumonia include Streptococcus pneumoniae and Mycoplasma pneumoniae. A variety of respiratory viruses such as rhinovirus, influenza, respiratory syncytial virus (RSV), and COVID-19 also cause pneumonia. Fungi can also cause pneumonia, especially in individuals with weakened immune systems.[3] See Figure 6.23[4] for an illustration of pneumonia.
Classifications of Pneumonia
Pneumonia is classified according to the type of microorganism that caused it and the location where the individual developed the infection. This classification affects the medical treatment plan and the antibiotics used to treat it. Classifications of pneumonia include the following[5]:
- Community-acquired pneumonia (CAP) refers to pneumonia that began in the community (not in a hospital).
- Hospital-acquired pneumonia (HAP) refers to pneumonia that began during or immediately following a stay in a health care setting. Health care settings include hospitals, long-term care facilities, and dialysis centers.
- Ventilator-associated pneumonia (VAP) refers to when someone gets pneumonia during or after being on a ventilator.
- Aspiration pneumonia refers to when someone inhales food, drink, vomit, saliva, or medication into the lungs instead of swallowing it. Risk factors for aspiration pneumonia include difficulty swallowing, a brain injury that causes an impaired gag reflex, oversedation by medications, or excessive alcohol or drug use.[6]
Assessment
Clinical manifestations of pneumonia vary in severity and can be influenced by factors such as the causative pathogen, as well as the individual’s age, overall health, and underlying medical conditions. See Table 6.7 for a summary of clinical manifestations of pneumonia across body systems. It is essential for nurses to recognize these symptoms early and notify the health care provider of suspected pneumonia.
Table 6.7. Clinical Manifestations of Pneumonia[7],[8]
| Body System | Clinical Manifestations |
|---|---|
| Respiratory | Cough (nonproductive or productive of purulent sputum), dyspnea, pleuritic chest pain (worse with deep breathing or coughing), labored breathing, tachypnea, fine crackles on auscultation, and decreased pulse oximetry readings |
| Cardiovascular | Tachycardia |
| Nervous | New onset confusion or altered mental status |
| Gastrointestinal | Decreased appetite |
| Musculoskeletal | Muscle aches and joint pain, especially for viral causes, fatigue, and weakness |
| Integumentary | Diaphoresis and cyanosis (bluish or grayish skin due to lack of oxygen) |
| General | Fever, shaking chills (most often with high temperature), malaise (general discomfort or uneasiness), and weight loss (often due to reduced appetite) |
Diagnostic Testing
Pneumonia is typically diagnosed through a combination of clinical assessment, medical history, and diagnostic tests. Common diagnostic tests used to diagnose pneumonia are as follows:
- Chest X-Ray: A chest X-ray identifies areas of the lung that are inflamed or filled with fluid, called “consolidation.” The X-ray provides a visual confirmation of the infection and its extent in the lungs.
- Complete Blood Count (CBC): An elevated white blood cell count is often an indicator of an infection.
- Sputum Culture: A sputum sample (mucus coughed up from the lungs) may be collected for laboratory testing to identify the causative microorganism. This is especially important for selecting appropriate antibiotic treatment.
In serious cases of pneumonia, especially for hospitalized clients, additional diagnostic testing may be performed[9],[10]:
- Arterial Blood Gas (ABG): ABG testing assesses the amount of dissolved oxygen and carbon dioxide levels in the blood and determines the severity of hypoxemia and hypercapnia.
- Bronchoscopy: In cases where the diagnosis is uncertain or when there is a need to examine the airways directly, a bronchoscopy may be performed. This involves passing a thin, flexible tube with a camera through the airways to visualize the lungs and collect samples.
- CT Scan: A computed tomography (CT) scan may be performed to provide more detailed images of the lungs.
- Blood Cultures: Blood cultures may be performed to determine if bacterial pneumonia has spread to the blood.
- Pleural Fluid Culture: A pleural fluid culture may be taken using a procedure called thoracentesis, which is a procedure where a health care provider uses a needle to take a sample of fluid from the pleural space between the lungs and chest wall.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing priorities for clients with pneumonia are focused on improving respiratory function, alleviating symptoms, and supporting recovery while preventing complications.
Nursing diagnoses for clients with pneumonia are formulated based on the client’s assessment data, medical history, and specific needs. Common nursing diagnoses include the following[11]:
- Ineffective Airway Clearance
- Impaired Gas Exchange
- Ineffective Thermoregulation
- Decreased Activity Intolerance
- Risk for Deficient Fluid Volume
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to pneumonia are as follows:
- The client will maintain oxygen saturation within the target range, typically above 92%.
- The client’s signs of infection, such as fever above 101 degrees Fahrenheit and elevated white blood cell count, will improve with treatment.
- The client’s reported level of dyspnea at rest and with activity will decrease with treatment.
Interventions
Medical Interventions
Medical interventions for pneumonia aim to treat the underlying infection, alleviate symptoms, and support the client’s recovery.
Medication Therapy
A variety of medications may be prescribed for clients with pneumonia[12],[13]:
- Antibiotic Therapy: Antibiotics are prescribed if the suspected or confirmed causative agent is bacteria. The choice of antibiotic by the health care provider is based on the classification of pneumonia (i.e., CAP, HAP, VAP, or aspiration pneumonia). The antibiotic may be adjusted based on sputum or blood culture and sensitivity results. Duration of treatment is determined by the type of pneumonia and the client’s clinical response.
- Antiviral Medications: If pneumonia is caused by a viral infection, antiviral medications may be prescribed. These medications aim to reduce viral replication and severity of symptoms.
- Antifungal Medications: If pneumonia is caused by a fungal infection, antifungal medications are utilized to target and eliminate fungal pathogens, disrupting their ability to grow and reproduce.
- Bronchodilators: Bronchodilators, such as albuterol, may be administered to alleviate bronchoconstriction and improve airflow, especially in clients with concurrent obstructive lung diseases like asthma or COPD.
- Corticosteroids: Corticosteroids may be prescribed in specific cases to reduce inflammation in the airways and improve breathing.
- Antipyretics: Antipyretic medications (e.g., acetaminophen or ibuprofen) may be prescribed to reduce fever and discomfort.
- Pneumococcal and Influenza Vaccinations: To prevent future episodes of pneumonia, clients are encouraged to receive influenza, COVID, and pneumococcal vaccines.
- Oxygen Therapy: Supplemental oxygen is prescribed to maintain adequate oxygen saturation levels. Oxygen delivery methods vary based on the client’s needs and severity of respiratory distress.
- Fluid Intake: Clients are encouraged to increase fluid intake to maintain hydration and thin secretions, if not contraindicated. For hospitalized clients, IV fluids may be prescribed, especially if the client has a high fever, reduced oral intake, or difficulty swallowing.
Read additional information about oxygen equipment and safety measures in the “Oxygenation Therapy” chapter of Open RN Nursing Skills, 2e.
Respiratory Therapies
Chest physiotherapy techniques, such as postural drainage and percussion, may be used to assist in clearing mucus and secretions from the airways. Vibratory positive expiratory pressure (PEP) therapy (i.e., flutter valves) may be prescribed for clients who need assistance in clearing mucus from their airways. Clients are encouraged to cough and deep breathe, and incentive spirometry devices may be prescribed to treat/prevent atelectasis. Review information about vibratory positive expiratory pressure therapy, coughing and deep breathing, and incentive spirometers in the “General Nursing Interventions Related to Respiratory Alterations” subsection earlier in this chapter.
Ventilation Support
In severe cases of pneumonia, noninvasive positive pressure ventilation, commonly referred to as CPAP or BiPAP, or intubation and mechanical ventilation may be necessary to provide respiratory support.[14],[15] See Figure 6.24[16] for an image of a simulated client with a BiPAP mask in place.

Read more about CPAP, BiPAP, and mechanical ventilation in the “Oxygen Equipment” section of the “Oxygen Therapy” chapter of Open RN Nursing Skills, 2e.
Pleural Procedures
In cases of pleural effusion (accumulation of fluid in the pleural cavity), procedures such as thoracentesis or chest tube insertion may be required.[17],[18]
Nursing Interventions
Nursing interventions for pneumonia focus on promoting recovery, preventing complications, and preventing future illness.
Medication Management
Nurses safely administer prescribed antibiotics, antivirals, or antifungals that target the specific pathogen causing pneumonia. Antipyretic medications (e.g., acetaminophen or ibuprofen) are administered as needed to reduce fever and discomfort. Bronchodilators may be administered to alleviate bronchoconstriction and improve airflow, especially in clients with preexisting lung conditions. Nurses teach clients about the purpose of prescribed medications and the importance of taking the full course of antibiotics as directed.
Maintain Hydration
Nurses monitor fluid intake and output and for signs of fluid volume deficit. Clients are encouraged to maintain adequate hydration, especially if they have a fever, productive cough, or increased respiratory rate that can contribute to fluid loss. Clients are encouraged to drink at least two liters of water daily to loosen secretions, unless they are on a fluid restriction.
Assist With Respiratory Therapy
Nurses assist clients with techniques such as postural drainage, coughing and deep breathing, incentive spirometry, and/or vibratory pressure therapy, as prescribed. Effective coughing techniques are demonstrated and encouraged. Review enhanced breathing and coughing techniques in the “General Nursing Interventions Related to Respiratory Alterations” subsection earlier in this chapter.
Infection Control
Nurses implement appropriate infection control measures, including hand hygiene, personal protective equipment, and transmission-based precautions based on the infectious organism to prevent the spread of infection.
Immunizations
Nurses encourage clients to remain up-to-date on recommended vaccinations, including the pneumococcal vaccine for adults at risk and all those over age 65.
Review current information about “Recommended Vaccines By Age” from the Centers for Disease Control and Prevention (CDC).
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Pneumonia
RN Recap: Pneumonia
View a brief YouTube video overview of pneumonia[19]:
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Centers for Disease Control and Prevention. (2022). Pneumonia. https://www.cdc.gov/pneumonia/index.html ↵
- “Lobar_pneumonia_illustrated.jpg” by Heart, Lung and Blood Institute is licensed in the Public Domain. ↵
- Centers for Disease Control and Prevention. (2022). Pneumonia. https://www.cdc.gov/pneumonia/index.html ↵
- Mayo Clinic. (2020). Pneumonia. https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204 ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- “Simulated patient wearing a BiPAP mask” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 6 - Pneumonia [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/PDbrPS3X50I?si=BGo8htPvDJIqfW82 ↵
Characterized by inflammation and infection within the alveoli, causing them to fill with fluid or purulent material, resulting in a productive cough, fever, chills, and difficulty breathing.
Refers to pneumonia that began in the community (not in a hospital).
Refers to pneumonia that began during or immediately following a stay in a health care setting.
Refers to when someone gets pneumonia during or after being on a ventilator.
Refers to when someone inhales food, drink, vomit, saliva, or medication into the lungs instead of swallowing it.
A procedure where a healthcare provider uses a needle to take a sample of fluid from the pleural space between the lungs and chest wall.
Techniques such as postural drainage and percussion, which may be used to assist in clearing mucus and secretions from the airways.
Therapy which uses handheld devices such as flutter valves or Acapella devices for clients who need assistance in clearing mucus from their airways.

