3.3 General Hematological System Assessment
When evaluating a client for possible disorders of the hematology system, the nurse pays close attention to risk factors, cultural factors, and socioeconomic factors, in addition to the client’s health history, physical examination findings, and diagnostic test results.
Risk Factors & Social Determinants of Health Related to Hematological System Risk Factors
Assessing for hematological risk factors allows health care professionals to identify individuals who may be at a higher risk of developing blood-related disorders. Identification of risk factors will allow for early intervention and preventative measures to be enacted, potentially impacting the severity or progression of the hematological alteration. It is important that nurses and health professionals carefully consider the following risk factors:
- Family History/Genetic Predisposition: Family history of certain blood disorders can increase an individual’s risk of developing the same condition. For example, hemophilia, a bleeding disorder, has a genetic predisposition.
- Age: Many hematological disorders are more commonly seen in older individuals. For example, anemia and chronic leukemia commonly occur in older adults.
- Environmental Exposures: Exposure to certain environmental toxins, radiation, or chemicals can increase an individual’s risk for developing a hematological condition. For example, exposure to benzene is an environmental risk for hematological conditions.
- Nutrition: Inadequate intake or absorption of essential nutrients, such as iron, vitamin B12, and folic acid, can lead to certain blood disorders. For example, iron-deficiency anemia can be caused by a lack of iron in the diet. Chronic health issues like inflammatory bowel disease can interfere with the absorption of nutrients.
- Medications: Medications can affect blood cell production and function. For example, chemotherapy and immunosuppressive medications can affect blood cell production and function.
- Underlying Health Conditions: Chronic health conditions can affect blood cell production and function, such as chronic kidney disease and liver disease.[1],[2]
Cultural Factors
Cultural practices, beliefs, and lifestyle choices can influence an individual’s health, including their risk for developing hematological conditions.
- Diet and Nutrition: Cultural dietary patterns can affect an individual’s intake of essential nutrients like iron, vitamin B12, and folic acid that are needed for healthy blood cell production. For example, vegetarian or vegan diets are often low in iron and can increase the risk for developing anemia.
- Herbal Medicines: Some cultural practices involve the use of traditional medicines and herbal remedies. While some herbal remedies may have beneficial effects, others might interfere with blood clotting or blood cell function and the risk of hematological disorders. For example, ginseng and green tea can interfere with blood clotting and should be discontinued before surgery.[3]
- Inherited Blood Disorders: Certain blood disorders, such as sickle cell disease or thalassemia, are more prevalent in specific ethnic groups due to inherited genetic factors. Cultural background can play a significant role in determining the prevalence of these conditions within certain populations.
- Traditional Practices and Rituals: Certain cultural practices may involve activities that carry a risk of bleeding or clotting disorders. For example, rituals in some cultural practices involve scarification or practices that may lead to injury and bleeding.
- Health Care Beliefs and Access: Cultural beliefs about health and illness can influence health care-seeking behaviors and adherence to medical advice. Lack of access to health care services or differences in health care practices between cultures may affect the detection and management of hematological disorders.
- Religious Practices: Some religious practices, such as fasting or dietary restrictions, may impact an individual’s nutritional intake and, in turn, affect their hematological health.
- Genetic Variations: Certain ethnic groups may carry specific genetic variations that affect blood cell function or clotting factors, leading to an increased risk of certain hematological disorders.[4],[5]
Socioeconomic Factors
Socioeconomic factors can play a significant role in impacting the hematological system. These factors may influence an individual’s access to health care, nutritional status, exposure to environmental hazards, and overall well-being.
- Access to Health Care: An individual’s access to quality health care services, including regular check-ups and early detection, can affect their health and hematological function. Limited access to medical care may result in delayed diagnosis and treatment of blood-related conditions, potentially leading to more severe health outcomes.
- Nutritional Status: Socioeconomic factors can influence an individual’s dietary habits and nutritional intake. Low socioeconomic status may be associated with limited access to nutritious foods, which could increase the risk of nutritional deficiencies and related hematological disorders, such as anemia.
- Exposure to Environmental Hazards: Socioeconomic factors can determine an individual’s living conditions and exposure to environmental pollutants. People in lower socioeconomic groups may be more likely to live in areas with higher pollution levels, which can negatively impact the hematological system.
- Occupational Hazards: Certain occupations may involve exposure to chemicals or toxins that can affect blood cell production or lead to hematological disorders.
- Stress and Mental Health: Prolonged stress can affect the immune system and blood cell production, potentially influencing hematological health.
- Health Care Adherence: Socioeconomic factors may affect an individual’s ability to adhere to prescribed medical treatments and follow-up appointments, impacting disease management and control of hematological disorders.
- Health Literacy: Socioeconomic status can influence health literacy. Health literacy refers to an individual’s ability to access, understand, and use health-related information. Lower health literacy may lead to a lack of awareness about hematological disorders and their prevention, hindering early intervention.
- Social Support: Support systems and social networks play a role in managing chronic conditions, including hematological disorders. Socioeconomic factors may influence the availability of social support, impacting disease management and outcomes.[6],[7]
General Assessment
A comprehensive evaluation of a client’s body systems is essential because hematological conditions can affect many body systems due to decreased oxygen delivery, increased risk for bleeding or clotting, or increased risk of infection.
Health History
Specific areas to note in a client history that may reveal an underlying hematological disorder include the following assessment findings[8],[9]:
- RBC impairment and impact on oxygenation:
- Fatigue: Fatigue is a common symptom of many hematological disorders, particularly anemia. Explore the client’s level of fatigue, its impact on daily activities, and any associated symptoms.
- Shortness of Breath, Heart Palpitations, or Chest Pain: Obtain information about the onset, duration, and triggers of shortness of breath, heart palpitations, or chest pain. Ask if the client experiences these symptoms at rest, during physical activity, or at specific times of the day.
- WBC impairment and risk for infection:
- Infection and Fever: Determine if the client has experienced any recent infections, such as respiratory or urinary tract infections, and ask about any associated fever or chills.
- Lymph Node Swelling: Lymph node swelling can occur with systemic infection. Inquire about the location, duration, and progression of any lymph node swelling. Ask if the client has noticed any changes in the size or tenderness of the lymph nodes.
- Platelet impairment and risk for bleeding:
- Excessive Bruising or Bleeding: Ask about any recent injuries or trauma and inquire about the frequency, severity, and duration of excessive bruising or bleeding. Take note of any history of recurrent nosebleeds, prolonged bleeding after minor cuts, bleeding gums, or blood in the urine or stool.
- Excessive or Prolonged Bleeding After Dental Work or During Menstruation: Specifically ask about any prolonged bleeding episodes after dental procedures or during menstrual periods.
Physical Assessment
Conducting a thorough examination of each body system provides the nurse with cues regarding potential hematological disorders. Early identification of abnormal findings and notification of the health care provider can lead to prompt intervention and management and improve client outcomes. Table 3.3a summarizes assessments for each body system.
Table 3.3a. General Hematological Assessments by Body System[10],[11]
| Body System | Focused Assessments |
|---|---|
| Skin |
|
| Head & Neck |
|
| Respiratory |
|
| Cardiovascular |
|
| Renal & Urinary |
|
| Musculoskeletal |
|
| Abdominal |
|
| Central Nervous |
|
| Psychosocial |
|
Based on the client’s health history and physical examination findings, the health care provider should be notified of signs of potential hematological disorders to determine the need for follow-up, such as blood tests, bone marrow examination, or imaging studies.
Check Your Knowledge – Clinical Scenario Part A
Sarah Jimenz presents to her primary care provider with a chief complaint of fatigue, bruising, and swollen lymph nodes in her neck for the past two months. She also reports ongoing shortness of breath with minor exertion and presence of heart palpitations.
Sarah denies any past medical issues, surgeries, or hospitalizations. She also is not currently taking any medications or herbal supplements. Her family history reveals no notable concerns. Sarah currently works as an elementary school teacher and is married with two children. She reports that she eats a balanced diet but has not been eating as much lately due to work-related stress and family responsibilities. She denies consuming tobacco products or alcohol.
A physical examination reveals the following findings:
Skin: Skin appears pale. No signs of jaundice or cyanosis. Petechiae and ecchymoses are observed on her lower extremities.
Head & Neck: Mucous membranes and nail beds appear pale. The tongue shows signs of slight fissures. Palpation of lymph nodes reveals bilateral enlargement of the cervical lymph nodes, which are slightly tender.
Respiratory: Respiratory rate is within the normal range at rest. However, she reports feeling fatigued easily and experiences shortness of breath with minimal exertion.
Cardiovascular: Pulses are regular and of normal strength. No distended neck veins or edema are noted. Blood pressure reading shows a lower value than usual.
Renal & Urinary: No hematuria or abnormal urine coloration is observed. However, Sarah mentions experiencing frequent urinary tract infections over the past few months.
Musculoskeletal: Firm pressure on the skin over the ribs and sternum elicits tenderness. Sarah reports some discomfort in these areas.
Abdominal: Palpation reveals an enlarged spleen on the left side under the ribs. The liver is not palpable. There are no signs of blood in the stool.
Central Nervous System: Sarah appears alert and oriented. There are no signs of neurological deficits or head trauma.
Psychosocial: Sarah expresses feeling overwhelmed and stressed due to work and family responsibilities. She has a good support system in her family and friends but admits not seeking help when needed.
1. Based upon Sarah’s case presentation, what physical assessment findings and clinical manifestations are consistent with the presence of a possible hematological alteration?
Pallor, petechiae, bruising, swollen lymph nodes, shortness of breath, enlarged spleen, fatigue, and tenderness in sternum are findings indicating a possible hematological alteration.
Life Span Considerations
Pediatric Considerations[12]
- A small volume of blood loss can be significant for small children. For example, 100 mL of blood loss by an infant weighing 5 kg is 10% of their total blood volume.
- RBC and WBC levels increase from birth throughout childhood, achieving adult levels in adolescence.
- Newborns’ platelet and clotting factors are low, so prophylactic vitamin K is administered at birth.
Older Adult Considerations
- Older adults have decreased blood volume with lower levels of plasma proteins.
- As bone marrow ages, there is less red bone marrow, and fewer blood cells are produced.
- Hemoglobin and hematocrit levels may be decreased.
- Atrophy of the kidneys, liver, and spleen affect the hematological system. Atrophic kidneys make less erythropoietin that stimulates the production of RBCs. An atrophied liver produces less clotting factors, and decreased functioning affects the recycling/breakdown of RBCs. An atrophic spleen stores fewer platelets and is less efficient in recycling the “heme” (i.e., the iron component) needed to produce RBCs.
- Increased incidence of arthritis, vision impairment, chronic disease, and living alone put older adults at risk for poor nutrition, resulting in the lack of nutrients needed for building RBCs.
- Thin skin, fragile blood vessel walls, and increased use of anticoagulants result in increased bruising.
- Initiating IV access can be challenging due to fragile vessels. Nurses consider the size of the IV cannula when initiating IV access and may select a smaller gauge cannula like 22 gauge.
- Chronic medical conditions (such as heart failure and kidney disease) increase the risk of fluid overload following blood transfusions, dialysis, and IV fluid administration.
Diagnostic Testing
Diagnostic testing is ordered by health care providers to identify and diagnose hematological conditions. When identifying hematological conditions, one of the most definitive signs of an issue is reflected in the change of laboratory test results. Common laboratory tests that are performed to assist in hematological alteration identification include the following[13]:
- Complete Blood Count (CBC): A CBC provides a comprehensive assessment of various blood components, including RBCs, WBCs, platelets, hematocrit (HCT), and hemoglobin (Hgb). Additional parameters help evaluate the overall health of the hematological system and can indicate anemia, infection, or other blood disorders:
- Mean Corpuscular Volume (MCV): Shows the size of the red blood cells, which can help to diagnose different types of anemia. An increased MCV means that red blood cells are large or macrocytic. This could be seen in vitamin B12 anemia. An decreased MCV means that red blood cells are small or microcytic. This could be seen with iron-deficiency anemia.
- Mean Corpuscular Hemoglobin Concentration (MCHC): Helps to determine the coloring of the red blood cells. A decrease in MCHC means that the red blood cells are hypochromic or paler than normal. This can be seen in iron-deficiency anemia.
- CBC With Differential: Measures the different types of white blood cells (i.e., neutrophils, neutrophils, lymphocytes, monocytes, eosinophils, and basophils).
- Peripheral Blood Smear: A peripheral blood smear is a microscopic examination of a thin layer of blood cells, allowing a provider to determine the shape, size, and appearance of different types of blood cells.
- Prothrombin Time/International Normalized Ratio (PT/INR): PT/INR tests evaluate the blood’s ability to clot through the extrinsic pathway. PT measures how long it takes for blood to clot after specific factors are added. INR is a standardized value used to monitor clients taking warfarin.
- Partial Thromboplastin Time (PTT): PTT assesses the blood’s ability to clot through the intrinsic pathway. PTT measures how long it takes for blood to clot after certain activators are added. It is used to evaluate coagulation disorders and monitor clients on heparin.
- Liver Function Tests (LFTs): Impaired liver function can affect the synthesis of clotting factors. Therefore, LFTs may be ordered if clotting abnormalities are seen.
- Iron Studies: Iron studies include tests like serum iron, total iron-binding capacity (TIBC), and ferritin levels. These tests are used to diagnose iron-deficiency anemia and other disorders related to iron metabolism.
- Serum Iron: Measures how much iron is in the blood.
- Total Iron-Binding Capacity (TIBC): Measures the blood’s ability to attach to iron and carry it throughout your body. More specifically, a TIBC test shows the amount of transferrin in the blood. Transferrin is a protein the liver makes that regulates the absorption of iron into the blood.
- Transferrin Saturation: Transferrin saturations of less than 20% indicate iron-deficiency anemia, while transferrin saturations of more than 50% suggest iron overload such as polycythemia.
- Serum Ferritin: Measures the amount of ferritin, a blood protein that contains iron. Low serum ferritin levels indicate iron-deficiency anemia, whereas high levels indicate a condition that causes the body to store too much iron, such as polycythemia.
Reference ranges of these diagnostic tests are provided in Appendix A.
Bone Marrow Aspiration & Biopsy
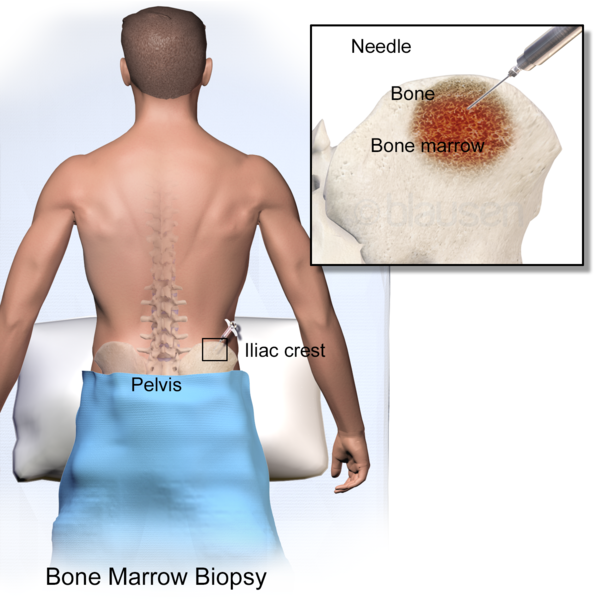
Bone marrow aspiration and biopsies are performed to obtain samples of bone marrow for diagnostic purposes. Results of bone marrow aspiration and biopsy guide health care professionals in providing tailored and effective care to clients.[14] The results of these procedures provide information about cell composition, overall health, and function of an individual’s bone marrow.
Bone marrow aspiration involves the extraction of a small sample of liquid bone marrow from the center of a bone. Common sites for bone marrow aspiration include the pelvic bone and sternum. The procedure is typically performed under local anesthesia. To perform the aspiration, the provider inserts a needle into the bone marrow space and then draws out a liquid sample. The aspiration allows the provider to evaluate the cellular components of the bone marrow, including the composition of red blood cells, white blood cells, and platelets. Bone marrow aspiration is helpful for determining the presence of severe blood disorders, such as leukemia, and is also used to monitor disease progression or treatment effectiveness.[15]
Bone marrow biopsy involves obtaining a small core of bone and marrow tissue from the bone marrow space. The procedure is often performed in conjunction with bone marrow aspiration. In contrast to the bone marrow aspiration procedure, the provider uses a larger needle to remove a cylindrical section of both the bone and marrow. Bone marrow biopsy provides a comprehensive evaluation of the bone marrow, allowing for a closer assessment of the bone marrow’s cellular density, structure, and the presence of any abnormal or diseased cells. It helps diagnose a wider range of conditions, including nonhematological disorders like metastatic cancers and immune diseases, that may infiltrate the bone marrow.[16]
See Figure 3.5[17] for an illustration of a bone marrow biopsy. See Figure 3.6[18] for an image of a bone marrow biopsy needle.

Nursing Care During Bone Marrow Aspiration/Biopsy
Nursing care for a client undergoing a bone marrow aspiration and biopsy involves not only assisting during the procedure but also providing comprehensive post-procedure care and emotional support. Nurses provide care to clients before, during, and after bone marrow aspiration and biopsy and also provide health teaching.
Pre-Procedure:
- Ensure informed consent has been obtained and the client understands the procedure, its purpose, and potential risks. Notify the surgeon of any concerns related to adequate informed consent.
- Address the client’s anxiety by providing clear and honest explanations and offering emotional support.
- Prepare the client for a sterile procedure and explain the need for the precautions to prevent infection.
- Position the client in a prone or side-lying position, whichever is more comfortable and suitable for the procedure.[19],[20],[21]
During the Procedure:
- Administer a local topical anesthetic to numb the area where the needle will be inserted, reducing discomfort during the procedure.
- Inform the client that they may experience a burning or stinging sensation, pressure, and a crunching sound as the needle enters the bone marrow space.
- Assist the health care provider with the procedure, ensuring the client remains as comfortable and still as possible.
- Offer reassurance and encouragement throughout the process, addressing any concerns the client may have.[22],[23],[24]
Post-Procedure Care:
- Monitor the client closely for any signs of bleeding, infection, or adverse reactions to the procedure.
- Administer a mild analgesic, as prescribed, to manage any discomfort or pain. The analgesic should be aspirin-free to prevent bleeding.
- Apply an ice pack to the site to help reduce swelling and discomfort.
- Inspect the aspiration site every two hours for any signs of bleeding, swelling, or infection.
- Ensure cessation of bleeding at the site by applying pressure as needed until it resumes.[25],[26],[27]
Health Teaching:
- Educate the client about potential side effects, such as mild pain or discomfort at the aspiration site and inform them of when to seek further medical attention if needed.
- Review any post-procedure care instructions and ensure the client understands how to care for the site and when to follow up with the health care provider.
- Offer emotional support and address any concerns or questions the client may have regarding the postoperative care at home.
- Provide instructions to the client on activity restrictions, advising against contact sports or any activity that may cause trauma to the area for 24-48 hours.[28],[29],[30]
Check Your Knowledge – Clinical Scenario Continued Part B
Recall Sarah Jimenz, discussed earlier in this section. Sarah presented to her primary care provider with a chief complaint of fatigue, bruising, and swollen lymph nodes in her neck for the past two months. She also reported ongoing shortness of breath with minor exertion and presence of heart palpitations.
Based on Sarah Jimenz’s presentation and the physical assessment findings previously discussed, the health care provider determines additional laboratory and diagnostic testing should be ordered.
1. What laboratory and diagnostic tests would be helpful in diagnosing Sarah? Why?
Complete Blood Count (CBC): Provides information about the number and types of blood cells in the client’s bloodstream. It includes measurements of red blood cells (RBCs), white blood cells (WBCs), and platelets.
Peripheral Blood Smear: Assesses the size, type, and shape of the blood cells.
Coagulation Studies:
- Prothrombin Time (PT)/International Normalized Ratio (INR): Allows for examination of extrinsic factors (Factor VII) in the clotting cascade.
- Partial Thromboplastin Time (PTT): Evaluates intrinsic pathway of clotting factors (Factors VIII, IX, XI, and XII).
Bone Marrow Aspiration & Biopsy: Provide insight into the production and maturation of blood cells.
Iron Studies: Evaluate iron status within the blood.
Liver Function Tests: Examine any abnormalities in liver function that may impact the synthesis of clotting factors.
- American Society of Hematology. (n.d.). Blood disorders. https://www.hematology.org/education/patients/blood-disorders ↵
- National Heart, Lung, and Blood Institute. (2023, August 7). Bleeding disorders: Causes and risk factors. National Institutes of Health. https://www.nhlbi.nih.gov/health/bleeding-disorders/causes ↵
- Wang, C. Z., Moss, J., & Yuan, C. S. (2015). Commonly used dietary supplements on coagulation function during surgery. Medicines, 2(3), 157–185. https://doi.org/10.3390/medicines2030157 ↵
- American Society of Hematology. (n.d.). Blood disorders. https://www.hematology.org/education/patients/blood-disorders ↵
- National Heart, Lung, and Blood Institute. (2023, August 7). Bleeding disorders: Causes and risk factors. National Institutes of Health. https://www.nhlbi.nih.gov/health/bleeding-disorders/causes ↵
- American Society of Hematology. (n.d.). Blood disorders. https://www.hematology.org/education/patients/blood-disorders ↵
- National Heart, Lung, and Blood Institute. (2023, August 7). Bleeding disorders: Causes and risk factors. National Institutes of Health. https://www.nhlbi.nih.gov/health/bleeding-disorders/causes ↵
- American Society of Hematology. (n.d.). Blood disorders. https://www.hematology.org/education/patients/blood-disorders ↵
- National Heart, Lung, and Blood Institute. (2023, August 7). Bleeding disorders: Causes and risk factors. National Institutes of Health. https://www.nhlbi.nih.gov/health/bleeding-disorders/causes ↵
- American Society of Hematology. (n.d.). Blood disorders. https://www.hematology.org/education/patients/blood-disorders ↵
- Office on Women’s Health. (2021, February 22). Bleeding disorders. U.S. Department of Health & Human Services. https://www.womenshealth.gov/a-z-topics/bleeding-disorders ↵
- Queensland Pediatric Emergency Care. (2022). How children are different - Anatomical and physiological differences. https://www.childrens.health.qld.gov.au/__data/assets/pdf_file/0031/179725/how-children-are-different-anatomical-and-physiological-differences.pdf ↵
- MedlinePlus. (2016, May 5). Blood count tests. National Library of Medicine. https://medlineplus.gov/bloodcounttests.html ↵
- Leukaemia Foundation. (n.d.). The bone marrow and blood formation. https://www.leukaemia.org.au/blood-cancer/understanding-your-blood/bone-marrow-and-blood-formation/ ↵
- Medline Plus. (n.d.). Bone marrow aspiration. National Library of Medicine. https://medlineplus.gov/ency/article/003658.htm ↵
- Medline Plus. (n.d.). Bone marrow biopsy. National Library of Medicine. https://medlineplus.gov/ency/article/003934.htm ↵
- “Blausen_0097_BoneMarrowBiopsy.png” by Blausen Medical Communications, Inc. is licensed under CC BY 3.0 ↵
- “Multi_Purpose_Bone_Marrow_Biopsy_Needle.jpg” by Thirteen Of Clubs from Minneapolis is licensed under CC BY-SA 2.0 ↵
- Leukaemia Foundation. (n.d.). The bone marrow and blood formation. https://www.leukaemia.org.au/blood-cancer/understanding-your-blood/bone-marrow-and-blood-formation/ ↵
- Medline Plus. (n.d.). Bone marrow biopsy. National Library of Medicine. https://medlineplus.gov/ency/article/003934.htm ↵
- Medline Plus. (n.d.). Bone marrow aspiration. National Library of Medicine. https://medlineplus.gov/ency/article/003658.htm ↵
- Leukaemia Foundation. (n.d.). The bone marrow and blood formation. https://www.leukaemia.org.au/blood-cancer/understanding-your-blood/bone-marrow-and-blood-formation/ ↵
- Medline Plus. (n.d.). Bone marrow biopsy. National Library of Medicine. https://medlineplus.gov/ency/article/003934.htm ↵
- Medline Plus. (n.d.). Bone marrow aspiration. National Library of Medicine. https://medlineplus.gov/ency/article/003658.htm ↵
- Leukaemia Foundation. (n.d.). The bone marrow and blood formation. https://www.leukaemia.org.au/blood-cancer/understanding-your-blood/bone-marrow-and-blood-formation/ ↵
- Medline Plus. (n.d.). Bone marrow biopsy. National Library of Medicine. https://medlineplus.gov/ency/article/003934.htm ↵
- Medline Plus. (n.d.). Bone marrow aspiration. National Library of Medicine. https://medlineplus.gov/ency/article/003658.htm ↵
- Leukaemia Foundation. (n.d.). The bone marrow and blood formation. https://www.leukaemia.org.au/blood-cancer/understanding-your-blood/bone-marrow-and-blood-formation/ ↵
- Medline Plus. (n.d.). Bone marrow biopsy. National Library of Medicine. https://medlineplus.gov/ency/article/003934.htm ↵
- Medline Plus. (n.d.). Bone marrow aspiration. National Library of Medicine. https://medlineplus.gov/ency/article/003658.htm ↵
Blood in urine.
The extraction of a small sample of liquid bone marrow from the center of a bone.
A procedure that involves obtaining a small core of bone and marrow tissue from the bone marrow space.

