9.3 General Nervous System Assessment
Risk Factors and Social Determinants of Health Related to the Nervous System
As with other body systems, neurologic health disparities are created and perpetuated by structural and social determinants of health. These factors include, but are not limited to, interpersonal bias, institutional factors that lead to disparate access to care, and neighborhood-level factors, such as socioeconomic status, segregation, and access to healthy food. Effects of these determinants of health can be seen throughout neurology, including in stroke, epilepsy, headache, amyotrophic lateral sclerosis, multiple sclerosis, and dementia.[1] Research shows that Black and Hispanic individuals were 30%-40% less likely to see an outpatient neurologist for care of a neurological condition compared with White individuals, even after adjusting for demographic, insurance, and health status differences.[2]
The environments in which individuals live and work also affect brain health. Lower socioeconomic status can result in exposure to toxic and unhealthy environments that increase risk for neurological disease.[3]
General Assessment of the Nervous System
Health History
Before obtaining a health history, note the client’s cognition, appearance, speech, and motor function. If any deficits in speech, hearing, or cognition are noticed, it is helpful to interview a family member or significant other to obtain accurate baseline information. If a family member or significant other is not available, the nurse may need to use questions with “Yes” or “No” answers and rely on information in the electronic health record.
Interview questions often include the following questions[4]:
- Are you experiencing any current neurological concerns such as headache, decreased vision, dizziness, weakness, numbness, tingling, tremors, loss of balance, or decreased coordination?
- Have you experienced any difficulty swallowing or speaking?
- Have you experienced any recent falls or head injury?
- Have you ever experienced a neurological condition such as a stroke, transient ischemic attack, seizure, dementia, Parkinson’s disease, multiple sclerosis, or myasthenia gravis?
- Are you currently taking any medications, herbs, or supplements for a neurological condition? (The nurse should be aware if the client is taking sedatives, analgesics, or neuromuscular-blocking agents, as these may interfere with an accurate neurologic assessment.)
- Do you use alcohol, marijuana, or other street drugs?
The nurse is also aware that neurologic disorders may be acute or progressive, and some are characterized by variation in symptoms or symptom-free periods.
Physical Examination of the Neurological System
The brain and spinal cord cannot be examined directly, so physical examination of the nervous system is performed using a variety of observations, assessments, and clinical testing. Much of the examination is an indirect evaluation of the functioning of specific body part(s) controlled or innervated by the nervous system.
Neurological assessment includes the following components[5]:
- Level of consciousness and orientation
- Memory and mood
- Cranial nerves
- Sensory function
- Motor function
- Cerebellar function
- Reflexes
- Psychosocial
Level of Consciousness (LOC)
One of the first cues of decreased neurological function is a change in level of consciousness. Evaluate the client’s ability to respond appropriately to questions, as well as their orientation to person, self, time, and situation, and compare current findings to their baseline. In acute care of a neurological disorder, use the Glasgow Coma Scale. If acute deterioration is noted, notify the health care provider and/or seek emergency assistance according to agency policy.
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is a standardized tool used to objectively assess and continually monitor a client’s level of consciousness when damage has occurred, such as after a head injury or a cerebrovascular accident (stroke). See Figure 9.7[6] for an illustration of the Glasgow Coma Scale. Three primary areas assessed in the GCS include eye opening, verbal response, and motor response. Scores are added from these three categories to assign a client’s level of responsiveness. A score of 15 or higher is classified as the best response, a score less than 8 is classified as comatose, and a score of 3 is classified as unresponsive. (Note that 3 is the lowest possible score.) Additionally, a score that has decreased two or more points from the previous assessment is considered clinically significant and should be reported to the health care provider.
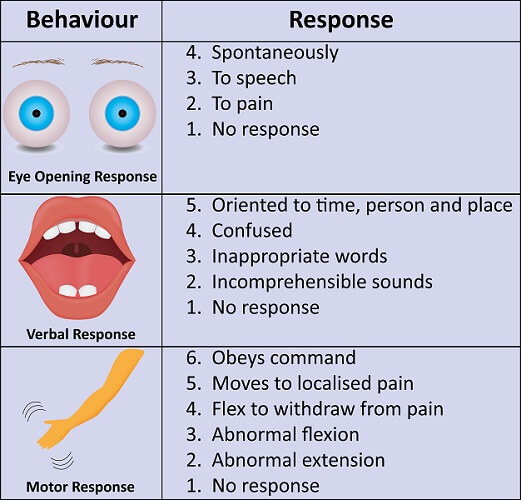
View the Glasgow Coma Scale and associated instructions: Glasgow Assessment Aid PDF.
Memory and Mood
Assess language and memory while asking the client for details regarding the current illness and any significant past events. During the exam observe for any agitation, anger, depression, or euphoria, as well as the appropriateness of these states.
Cranial Nerves
When assessing cranial nerves, compare opposite sides of face and neck, noting if there are differences. Each side should be symmetrical. The assessment of multiple cranial nerves can be combined, such as eye movement (controlled by cranial nerves III, IV, VI).
Review how to perform a cranial nerve assessment in the “Assessing Cranial Nerves” section of the “Neurological Assessment” chapter of Open RN Nursing Skills, 2e.
Sensory Function
When testing sensory function, several areas are tested. Recall that each sensory modality is carried by a specific ascending pathway in the spinal cord before it reaches the sensory cortex of the brain.
As a rule, when performing sensory testing, do so with the client’s eyes closed. Avoid providing cues. For example, ask the client, “How does this feel?” rather than “Does this feel sharp?” Sensory testing of the anterior and posterior torso and all four extremities is typically sufficient in a routine neurological examination. However, if there is an abnormality within the routine neurological exam, further investigation is warranted.
Light touch is usually tested by using a cotton wisp or soft pinprick. Each of the four extremities is tested by asking the client to tell the examiner if they feel the stimulus. Testing pain reception is performed by alternatively touching the skin with a dull item and then a sharp end of a pin. The client is then asked to respond “Sharp” or “Dull.” Each limb should be evaluated separately.
Motor Function
The motor system exam includes assessment of muscle strength, tonicity, coordination, and symmetry. Ask the client to push and pull against the resistance of your arm, rating their strength on a scale of 1-5, with 5 being the strongest. These actions assess flexion and extension of the client’s muscle and should be performed at the client’s shoulder, elbows, wrists, hips, knees, and ankles.
To test muscle tone, passively move the client’s limbs through their range of motion. As the client’s muscles are moved, the nurse should be able to identify a slight resistance to the movements. Abnormal tone is referred to as hypotonia (flaccidity) or hypertonia (spasticity).
During the motor exam, observe and document any involuntary movements such as tics, tremors, or myoclonus (spasm of muscles) and evaluate for coordination and symmetry of movement.
Cerebellar Function
Cerebellar function is tested by assessing gait, balance, and coordination. Ataxia refers to lack of muscle control in the arms and legs that causes poor balance and coordination, which can result in trouble walking.
Observe a client’s posture while standing, as well as their gait when walking. These are good screening tests for balance and muscle strength because being able to hold up one’s weight in a standing position and walking require muscle strength, as well as the coordination of the nervous system. It is also an excellent way to determine the client’s fall risk and level of fall precautions required.
To examine fine motor movement and coordination, perform the finger-to-nose test, heel-to-shin test, and alternative hand movement test. In the finger-to-nose test, ask the client to alternately touch their nose and then your finger. During the heel-to shin test, ask the client to stroke the heel of one foot up and down the shin of their opposite leg. During the alternating hand movement test, ask the client to rapidly pronate and supinate both hands simultaneously. Being able to perform these tests accurately and smoothly indicates a normal test.
View a supplementary YouTube video[7] on assessing cerebellar function: Cerebellar Function Tests.
Reflexes
Reflexes are assessed by testing the reflex contraction of the skeletal muscle when the associated tendon is stretched. Tendons have built in receptors that are sensitive to stretch. The biceps, triceps, brachioradialis, patellar, Achilles tendon reflexes, and Babinski reflex are typically tested by advanced practice nurses and health care providers. The nurse should be aware of the purpose of reflex testing and correlate abnormal findings with the client’s condition.
Psychosocial
Nurses assess the client’s psychosocial response to illness or injury and plan customized interventions to promote effective coping.
Life Span Considerations
Pediatric Considerations
Nurses consider the following differences when caring for pediatric clients. [8]
- The anterior fontanel of an infant remains open until 12-18 months of age. The posterior fontanelle of an infant closes between 2-3 months of age.
- Newborns and infants have underdeveloped temperature regulation that can result in hypothermia if their heads are left exposed.
- Children have increased fall risk due to incomplete motor development.
- Children are more susceptible to head injuries due to their larger head size in relationship to their body size.
- The cranial bones of pediatric clients are thin and leave brain tissue less protected, resulting in hemorrhages, head trauma, and diffuse brain injury as the result of accidents or injuries.
Older Adult Considerations
Nurses consider the following differences when caring for older adults. [9]
- The brains of older adults experience normal physiological changes associated with aging, such as atrophy, decreased vascularization, and memory impairment.
- The percentage of people with Alzheimer’s disease (AD) increases dramatically with age, with 33% of people aged 85 or older having AD.
- The number of neurotransmitters, particularly dopamine and serotonin, decline with aging. In addition, neuronal, dendrite, and myelin changes negatively impact nerve impulse transmission.
- Ischemia that occurs later in life may result in white matter lesions, strokes, and increased risk for dementia. Prolonged decreased blood flow to the brain can result in permanent damage.
Common Laboratory and Diagnostic Testing
Blood tests associated with neurological assessment may include the following:
- Complete blood count (CBC) and serum levels of albumin and vitamins/minerals (particularly B vitamins) because anemia, malnutrition, and vitamin deficiencies can contribute to neurological disorders.
- Basic metabolic panel (BMP) with serum calcium, phosphorous, and magnesium levels to assess for abnormal electrolytes and glucose that can cause neurologic impairment.
- Arterial blood gas (ABG) because respiratory distress can alter neurological status, so pH, oxygen, and carbon dioxide levels are evaluated.
- Drug screen because alcohol and drugs may contribute to neurological impairment.
- Blood, urine, or other cultures because underlying infection can lead to abnormalities in the neurologic system, such as meningitis and encephalitis.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
There are several common diagnostic tests that may be ordered for the diagnosis and monitoring of neurologic system disorders. See Table 9.3 for descriptions of common diagnostic tests and associated nursing considerations.
Table 9.3. Common Diagnostic Tests for Nervous System Disorders
| Diagnostic Test | Description and Indication | Nursing Considerations |
|---|---|---|
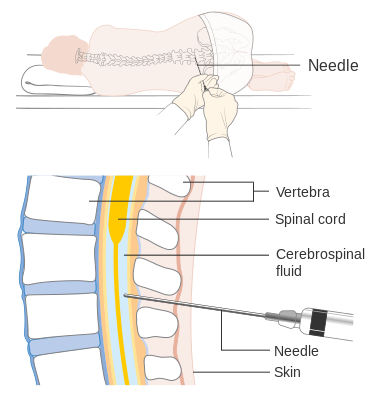
| Lumbar puncture (See Figure 9.8[10]) | Cerebrospinal fluid (CSF) is aspirated from the subarachnoid space by a health care provider by inserting a needle between L3-4 or L4-5. Used to examine CSF for infection or presence of blood and measure and reduce CSF pressure. Fluid should be clear and colorless. Pink or blood-tinged CSF may be a sign of subarachnoid hemorrhage, and cloudiness may be due to increased WBCs. | Before: Ensure written consent is obtained. Describe sensations that may occur during the procedure, such as a temporary, sharp pain or tingling that radiates down the leg as the sterile needle is passed between the lumbar vertebrae. Ask the client to void before the procedure and then assist the client into a side-lying position with their back toward the provider. Legs should be flexed as much as possible to make it easier for the provider to access the correct area.
During: Assist the client to maintain the position and avoid sudden movement, which can cause injury. After: Assist the client to lie supine on bedrest for a few hours after the test. Encourage fluids. Monitor neurologic signs and vitals. Monitor for post puncture spinal headache, meningeal irritation (nuchal rigidity), hematoma, and pain. Administer analgesics as needed. |
| CT (computed tomography) scan | Computer assisted X-ray that provides cross-sectional views of body parts. Used to detect problems such as hemorrhage, tumor, cyst, infarction, edema, brain atrophy, and other abnormalities. Contrast can be used to enhance visualization of brain structures, although scanning is typically first performed without contrast. | Before: Assess for allergies or contraindications to contrast, such as allergies to shellfish, iodine, or dye. Evaluate kidney function tests and notify the provider of any concerns prior to the administration of contrast. Assess for and address anxiety related to procedure. Instruct the client to remain still during the procedure.
Note: *If IV contrast is planned for clients taking metformin, there is risk for lactic acidosis if they have severe renal dysfunction (i.e., estimated glomerular filtration rate [eGFR] <30 mL/min) and contrast is contraindicated. Notify the provider before proceeding. After: Promote fluid intake to assist in elimination of contrast. |
| X-rays (skull and spine) | Simple X-ray images of the skull and spine are done to detect fractures, calcifications, bone erosion, and abnormal vascularity. | Before: Explain that the procedure is noninvasive. |
| Cerebral angiography | Considered the gold standard for diagnosis of intracranial vascular disease. This test is a series of X-rays using contrast medium to visualize intracranial and extracranial blood vessels and identify impaired perfusion to the brain tissue. It is performed to detect vascular lesions such as hematoma, AV malformations, and aneurysms and tumors of the brain. A catheter is typically inserted into the femoral artery and advanced into the base of the carotid or vertebral area to inject the contrast. | Before: Assess the client for stroke risk because thrombi may dislodge during the procedure. Provider orders typically include an NPO order after midnight prior to the procedure. Inform the client they may feel a hot flush when the contrast medium is injected and to lie still during the procedure.
During: Monitor for signs and symptoms of an allergic/anaphylactic reaction from the contrast dye. After: Monitor insertion site and pulses distal to the insertion site. Perform neuro checks and vital signs according to agency policy, typically every 15-30 minutes x two hours and then every hour x 24 hrs. Ensure bed rest for the first six hours. If a closure device is used at the insertion site, bed rest is only required for one hour. Monitor for bleeding and report any neurological status changes. |
| Magnetic resonance imaging (MRI) (See Figure 9.9[11]) | Provides imaging of the brain and spinal cord by using magnetic energy to detect strokes, multiple sclerosis, tumors, trauma, seizures, and brain herniation. Produces greater detail than CT with improved detail of intracranial structures, but the procedure takes longer to complete and may not be appropriate if a client is experiencing a life- threatening emergency.
Contrast agents, such as gadolinium, can be used with MRI to enhance visualization. |
Before: Screen the client for presence of any metal parts internally and externally, such as pacemakers, metal plates, jewelry, etc. Instruct the client they need to lie very still for up to one hour. Assess for claustrophobia prior to the procedure because sedation may be necessary.
For client safety, no client care equipment such as oxygen tanks that contain metal can enter the MRI room. |
| Positron emission tomography (PET) | Measures metabolic activity of the brain to determine cell death or damage. A radioactive isotope is injected that shows up as a bright spot on the image if abnormal activity is occurring. Indicated for clients with stroke, Alzheimer’s disease, seizure disorders, Parkinson’s disease, infection, and tumors. | Before: Provider orders typically indicate the client should be NPO with no caffeine, alcohol, tobacco, sedatives, or tranquilizers prior to exam because these substances can interfere with the results. Ask the client to void before the procedure. |
| Myelogram | X-rays of the spinal cord and vertebral column are taken after contrast is injected into the subarachnoid space. Used to detect spinal lesions and/or CSF leaks. | Before: Explain the test is performed on a tilting table that is moved during the test. Ask the client to empty their bladder prior to the test. Administer sedative if ordered.
After: Client should lie flat for a few hours. Perform neuro checks and vital signs according to agency policy. Monitor for headache and nausea/vomiting. |
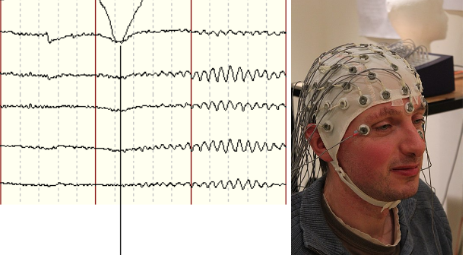
| Electroencephalography (EEG) (See Figure 9.10[12]) | Electrodes are placed on the scalp to record electrical activity of the cerebral hemispheres. Each graphic recording represents electrical impulses within the brain. The frequency, amplitude, and characteristics of the brain waves are recorded to evaluate seizure disorders, cerebral disease, brain injury, and brain death. | Before: Instruct the client the test is noninvasive and does not cause electric shock. Anti-seizure medications are held prior to the procedure. Sleep deprivation prior to the procedure may be encouraged to attempt to invoke an event during testing. Fasting and caffeine should be avoided before the procedure because hypoglycemia and caffeine can alter the test results. Ensure that hair is clean and without conditioners, hair creams, lotions, sprays, or styling gels. Verify with the provider if any medications such as tranquilizers or anti-seizure medications should be held prior to the exam.
After: Resume any medications that were held. Remove the electrode paste from the scalp/hair. |
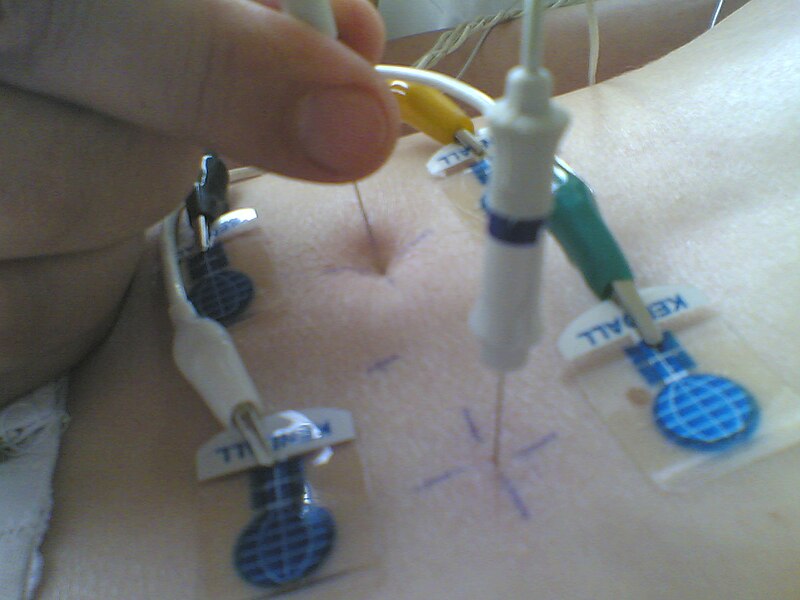
| Electromyography (EMG)(See Figure 9.11[13]) | Records the muscle and nerve integration and electrical activity. Needle electrodes are inserted into the specific muscle units being tested. Normal, relaxed muscles show no electrical activity, and contracted muscles show electrical activity. The test is indicated for testing for muscle and nerve diseases. | Before: Explain the procedure and inform the client that there will be some pain associated with the insertion of the needle electrodes. |
| Electroneurography (nerve conduction studies) | Measures the conduction velocity of peripheral nerves. A brief electrical stimulus is initiated at the distal portion of the sensory nerve being tested. A recording of the depolarization wave is taken at a point proximal to the stimulus. The time between the initial stimulus and the beginning of the depolarization wave is measured (i.e., nerve conduction velocity). Damaged nerves will have slower conduction velocities. | Before: Instruct the client on the procedure. |
| Carotid artery duplex scan | Combines ultrasound and Doppler technology to evaluate the degree of stenosis (narrowing) of the carotid and vertebral arteries. Using transducer gel, a probe is placed over the common carotid artery and moved slowly along its length. Frequency of reflected ultrasound signal corresponds with the velocity of blood flow. Increased blood flow velocity may indicate stenosis or partial or total occlusion of the vessels. | Before: Explain the test is noninvasive. |
- Rosendale, N. (2022). Social determinants of health in neurology. Neurologic clinics. 40(1), 231-247. https://doi.org/10.1016/j.ncl.2021.08.012 ↵
- Rost, N. S., Salinas, J., Jordan, J. T., Banwell, B., Correa, D. J., Said, R. R., Selwa, L. M., Song, S., & Evans, D. A. (2023). The brain health imperative in the 21st century - A call to action. Neurology. 101(13), 570-579. https://doi.org/10.1212/WNL.0000000000207739 ↵
- Rost, N. S., Salinas, J., Jordan, J. T., Banwell, B., Correa, D. J., Said, R. R., Selwa, L. M., Song, S., & Evans, D. A. (2023). The brain health imperative in the 21st century - A call to action. Neurology. 101(13), 570-579. https://doi.org/10.1212/WNL.0000000000207739 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/ ↵
- “glasgow-coma-scale-gcs-600w-309293585.jpg” by joshya on Shutterstock. All rights reserved. Image used with purchased permission. ↵
- Patient Examination Videos - Educor. (2022, April 14). Cerebellar function tests [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=VmsXL40Yado ↵
- Queensland Emergency Pediatric Care. (2022). How children are different: Anatomic and physiological differences. https://www.childrens.health.qld.gov.au/__data/assets/pdf_file/0031/179725/how-children-are-different-anatomical-and-physiological-differences.pdf ↵
- Peters, R. (2006). Ageing and the brain. Journal of Postgraduate Medicine, 82(964), 84-8. https://doi.org/10.1136/pgmj.2005.036665 ↵
- “Diagram_showing_how_you_have_a_lumbar_puncture_CRUK_157.svg” by Cancer Research UK is licensed under CC BY-SA 4.0 ↵
- “HITACHI,_Magnetic_Resonance_Imaging_System,_ECHELON_OVAL,.jpg” by Mj-bird is licensed under CC BY-SA 3.0 ↵
- "Normalt_EEG_vaken_vuxen.PNG" by Nitramus is licensed under CC BY-SA 3.0 and ”Three_quarter_view_of_EEG_subject.jpg” by Chris Hope, with permissions from Tim Sheerman-Chase, is licensed under CC BY 2.0 ↵
- "Normalt_EEG_vaken_vuxen.PNG" by Nitramus and “Needle_EMG_of_paravertebral_muscles(2J009).jpg” by Kychot are licensed under CC BY-SA 3.0 ↵
A standardized tool used to objectively assess and continually monitor a client’s level of consciousness when damage has occurred, such as after a head injury or a cerebrovascular accident (stroke).
Flaccidity.
Spasticity.
Spasm of muscles.
Tested by assessing gait, balance, and coordination.
Poor balance and coordination.

