5.6 Arteriosclerosis & Atherosclerosis
Overview
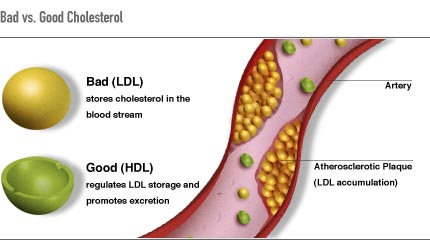
Arteriosclerosis and atherosclerosis are interrelated cardiovascular conditions that can significantly impact cardiac health. Arteriosclerosis refers to the thickening and stiffening of arterial walls.[1] It is commonly associated with normal aging. The subsequent loss of elasticity of blood vessels makes them less responsive to changes in blood flow and can reduce blood flow to organs and tissues within the body. Atherosclerosis is a condition where cholesterol, low-density lipoprotein (LDL) deposits, and wastes build up within the lining of the arteries.[2] This buildup of substances within the vessel walls, often referred to as plaque, creates inflammation and can cause blockage of the artery. Clients who experience arteriosclerosis often will also experience atherosclerosis as plaque accumulates within blood vessels. Conditions such as diabetes often correlate with arteriosclerosis and atherosclerosis as the result of sustained inflammation within the vessels from elevated blood glucose levels. See Figure 5.27[3] for an image of an atherosclerotic plaque resulting from LDL accumulation.
Assessment
Signs and symptoms of arteriosclerosis and atherosclerosis often develop as a result of decreased oxygenation to tissues and organs within the body. The manifestations will vary depending on where the arterial hardening or blockage is located within the body. See Table 5.6 for potential clinical manifestations of arteriosclerosis and atherosclerosis.
Table 5.6. Clinical Manifestations of Arteriosclerosis and Atherosclerosis[4],[5]
| Body System | Physical Assessment Findings |
|---|---|
| Cardiovascular System | – Hypertension (high blood pressure)
– If atherosclerosis develops in a coronary artery, chest pain (angina) associated with coronary artery disease (CAD) |
| Peripheral Vascular | – Cool extremities
– Pallor in extremities – Weak peripheral pulses – Capillary refill time greater than three seconds – Signs of peripheral artery disease (PAD), such as intermittent claudication (leg pain with walking) |
| Neurological | – Transient ischemic attacks (TIAs) or stroke symptoms if cerebral arteries are affected (e.g., weakness, speech difficulties, visual disturbances, confusion)
– Neuropathy in extremities |
| Renal | – Decreased urine output if renal arteries are affected, causing chronic kidney disease (CKD) |
| Integumentary | – Cool or pale skin
– Delayed wound healing |
| Ophthalmic | – Vision loss if retinal arteries are affected |
Diagnostic Testing
Diagnostic testing for atherosclerosis involves various methods to assess the condition of arteries and determine the extent of plaque buildup and narrowing of the arterial walls. Laboratory tests, such as lipid profile and C-reactive protein are related to the buildup of cholesterol or inflammation within the arteries respectively. Additional diagnostic testing that may be performed include carotid ultrasound to examine blood flow within the carotid arteries. Coronary angiography and coronary CT angiography (CTA) may be ordered to visualize strictures and buildup of plaques within the coronary arteries.[6]
Nursing Problems and Diagnoses
Nursing problems and diagnoses for clients with atherosclerosis focus on identifying abnormalities and preventing complications associated with these conditions.
Common nursing diagnoses for clients with atherosclerosis include the following[7]:
- Risk for Impaired Tissue Integrity related to altered circulation
- Readiness for Enhanced Health Self-Management
Outcome Identification
Outcome identification involves setting short- and long-term goals and creating expected outcome statements tailored to the client’s specific needs. These outcomes should be measurable and responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to atherosclerosis are as follows:
- The client will exhibit adequate tissue perfusion, as evidenced by vital signs within normal range, warm extremities, and capillary refill less than two to three seconds.
- The client will verbalize three lifestyle modifications to reduce the risk of plaque buildup.
- The client will verbalize when to notify the health care provider of new symptoms related to worsening atherosclerosis.
Interventions
Medical Interventions
Medical interventions for arteriosclerosis and atherosclerosis aim to improve blood flow through the affected arteries and reduce the risk of complications related to insufficient arterial blood flow to other organs. Interventions include lifestyle modifications, medication therapy, and surgical procedures.
Lifestyle Modifications
Recommended lifestyle medications include the following:
- Dietary Changes: Adopting a heart-healthy diet that is low in saturated fats, cholesterol, and sodium can help reduce plaque buildup and lower blood pressure.
- Regular Physical Activity: Engaging in regular physical activity can improve cardiovascular health, reduce cholesterol levels, and enhance overall circulation.
- Smoking Cessation: Quitting smoking is crucial, as smoking is a major risk factor for atherosclerosis and arterial disease.
- Weight Management: Achieving and maintaining a healthy weight can help improve blood pressure and reduce the workload on the heart.
- Blood Sugar Management: Tight control of blood sugars in clients with diabetes diminishes the progression of arteriosclerosis and atherosclerosis.
Medication Therapy
Several classes of medications may be prescribed to manage atherosclerosis and arteriosclerosis:
- Antilipemics: Lower LDL cholesterol levels and reduce the risk of plaque buildup.
- Antihypertensives: Control high blood pressure and reduce strain on the arteries; vasodilators relax blood vessels and improve blood flow.
- Blood coagulation modifiers (Antiplatelets and anticoagulants): Prevent blood clots from forming in narrowed arteries.
For additional information about the classes of medications used to treat arteriosclerosis and atherosclerosis, visit the “Cardiovascular & Renal System” chapter in Open RN Nursing Pharmacology, 2e.
Surgical Interventions
Several procedures or surgeries may be performed, depending on the location of the plaque buildups. An endarterectomy is the surgical removal of plaque from arteries. Procedures related to atherosclerosis in the coronary arteries are discussed in “Medical Interventions” in the “Coronary Artery Disease” section. In acute situations where atherosclerotic plaque becomes a thrombotic clot or embolus obstructing blood flow, thrombolytic medications may be administered.[8],[9]
Nursing Interventions
Nursing interventions for arteriosclerosis and atherosclerosis include safely administering medications and providing health teaching about lifestyle modifications, risk factor reduction, and medication therapy.
Medication Management
Nurses administer prescribed medications and teach about potential side effects and when to notify the provider.
Health Teaching
Nurses provide health teaching about lifestyle modifications to promote heart health, including dietary changes, smoking cessation, and regular physical activity. A heart-healthy diet is encouraged that is low in saturated fats, cholesterol, and sodium. If the client smokes and is ready to stop smoking, resources are provided for quitting. Realistic physical activity is recommended based on the client’s abilities. Risk factor modification, including controlling blood pressure, cholesterol levels, and blood sugar (if applicable), is emphasized during health teaching.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
- Kaski, J. C. (2022). Pathogenesis of atherosclerosis. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Crea, F., Kolodgie, F., Finn, A. & Virmani, R. (2022). Mechanisms of acute coronary syndromes related to atherosclerosis. UpToDate. Retrieved August 20, 2023, from https://www.uptodate.com/ ↵
- “máu nhiễm mỡ - cholesterol” by LÊ VĂN THẢO is licensed under CC BY-SA 2.0 ↵
- Kaski, J. C. (2022). Pathogenesis of atherosclerosis. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Crea, F., Kolodgie, F., Finn, A. & Virmani, R. (2022). Mechanisms of acute coronary syndromes related to atherosclerosis. UpToDate. Retrieved August 20, 2023, from https://www.uptodate.com/ ↵
- Crea, F., Kolodgie, F., Finn, A. & Virmani, R. (2022). Mechanisms of acute coronary syndromes related to atherosclerosis. UpToDate. Retrieved August 20, 2023, from https://www.uptodate.com/ ↵
- Flynn Makic, M.B., and Martinez-Kratz, M.R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care. 13th edition. ↵
- Kaski, J. C. (2022). Pathogenesis of atherosclerosis. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Crea, F., Kolodgie, F., Finn, A. & Virmani, R. (2022). Mechanisms of acute coronary syndromes related to atherosclerosis. UpToDate. Retrieved August 20, 2023, from https://www.uptodate.com/ ↵
Thickening and stiffening of arterial walls.
A condition where cholesterol, low-density lipoprotein (LDL) deposits, and wastes build up within the lining of the arteries.
The surgical removal of plaque from arteries.
A blood clot, air bubble, or fatty deposit which has been carried in the bloodstream to lodge in a vessel

