7.5 Antiemetics
This section will review the pathophysiology of nausea and vomiting and then apply the nursing process to administering antiemetic medications.
Review of the Pathophysiology of Nausea and Vomiting
Nausea and vomiting are common conditions. Nausea is the unpleasant sensation of having the urge to vomit, and vomiting (emesis) is the forceful oral expulsion of gastric contents.[1] There are many potential causes of nausea and vomiting, such as the following:
- Morning sickness during pregnancy
- Gastroenteritis and other infections
- Migraines
- Motion sickness
- Food poisoning
- Side effects of medicines, including those for cancer chemotherapy
- GERD and ulcers
- Intestinal obstruction
- Poisoning or exposure to a toxic substance
- Diseases of other organs (cardiac, renal, or liver)
Nausea and vomiting are common and are usually not serious. However, the health care provider should be contacted immediately if the following conditions occur:
- Vomiting for longer than 24 hours
- Blood in the vomit (also called hematemesis)
- Severe abdominal pain
- Severe headache and stiff neck
- Signs of dehydration, such as dry mouth, infrequent urination, or dark urine
Treatment of nausea and vomiting should be tailored to the cause. There are several medications that work on different neuroreceptors that when used can treat nausea and vomiting. For severe cases of vomiting, intravenous fluids may also be needed to treat the accompanying dehydration.[2],[3]
The Vomiting Center and Associated Neurotransmitters
The vomiting center can be activated directly by irritants or indirectly following input from four principal areas: gastrointestinal tract, cerebral cortex and thalamus, vestibular region, and chemoreceptor trigger zone (CRTZ). See Figure 7.18 for an illustration of the pathophysiology of nausea and vomiting.[4]
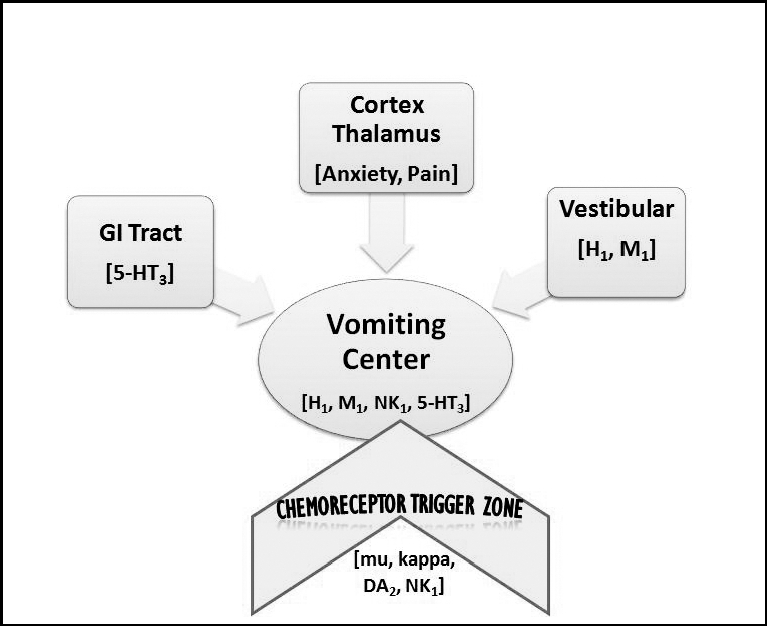
An important part of the emesis circuit is the chemoreceptor trigger zone (CTZ), located in the area postrema in the brain. The CTZ is not restricted by the blood–brain barrier, which allows it to respond directly to toxins in the bloodstream such as anesthesia and opioids. The CTZ also receives stimuli from several other locations in the body, including the vestibular center; visceral organs such as the GI tract, kidneys, and liver; the thalamus; and the cerebral cortex.
The vestibular center and cerebral cortex can stimulate the vomiting center directly or indirectly through the CTZ. The vestibular system is located within the inner ear and gives a sense of balance and spatial orientation for the purpose of coordinating movement with balance. The feeling of nausea associated with motion sickness often arises from stimuli from the vestibular center. The gastrointestinal tract sends stimuli to the CTZ via cranial nerves IX and X related to obstruction, distension, inflammation, and infection. The cerebral cortex and other parts of the brain can also stimulate a sense of nausea related to odors, tastes, and images and send these stimuli to the CTZ. The CTZ forwards these signals to the vomiting center in the brain. Pain can also directly stimulate the vomiting center.
The vomiting center (VC) is located in the medulla in the brain. In response to these stimuli, the vomiting center initiates vomiting by inhibiting peristalsis and producing retro-peristaltic contractions beginning in the small bowel and ascending into the stomach. It also produces simultaneous contractions in the abdominal muscles and diaphragm that generate high pressures to propel the stomach contents upwards. Additionally, autonomic stimulation of the heart, airways, salivary glands, and skin cause other symptoms associated with vomiting such as salivation, pallor, sweating, and tachycardia. Several neurotransmitters are involved in the nausea and vomiting process, and antiemetic medications are targeted to specific neuroreceptors.[5]
Table 7.5a compares the neurotransmitters involved in the nausea and vomiting process, classes of antiemetic medication targeting these neurotransmitters, prototype antiemetic medications, and associated mechanisms of action.[6] Each medication class is also discussed in more detail later in this section.
Table 7.5a Neurotransmitters and Associated Medications Used to Treat Nausea and Vomiting
| Neurotransmitter | Medication Class | Antiemetic Drug | Mechanism of Action |
|---|---|---|---|
| Acetylcholine (M1) | Anticholinergics | scopolamine | Blocks ACh receptors in vestibular system |
| Histamine (H1) | Antihistamines | meclizine | Blocks H1 receptors and thus blocks ACh in vestibular system |
| Dopamine (DA2) | Dopamine antagonists | prochlorperazine | Blocks dopamine in CTZ and may block ACh |
| Dopamine and ACh (DA2 and M1) | Prokinetics | metoclopramide | Blocks dopamine in CTZ and stimulates ACh in GI tract |
| Serotonin (5HT) | Serotonin antagonists | ondansetron | Blocks serotonin in GI tract, CTZ, and VC |
| Substance P (NK1) | Neurokinin antagonists | aprepitant | Inhibits substance P neurokinin receptors |
| Cannabinoid (CB1) | Tetrahydrocannabinols (THC) | dronabinol or medical marijuana | Activated CB1 receptor leading to inhibitory effects on cerebral cortex |
Applying the Nursing Process to Administering Antiemetics
Assessment
When administering antiemetics, identify factors contributing to the symptoms of nausea and vomiting so that treatment can correctly target the cause. Document the frequency and amount of emesis and effects on the client’s appetite and fluid intake. Assess for symptoms of dehydration, such as decreased blood pressure associated with tachycardia, decreased skin turgor, and decreased urine output or dark concentrated urine. If lab tests are ordered, monitor hemoglobin, hematocrit, and serum sodium levels for additional signs of dehydration.
Implementation
Advocate for the most effective route of administration if the client is vomiting. Consider timing of administration of antiemetics in advance of meals when appetite is affected. Follow drug label administration information and monitor the client closely for potential side effects associated with that category of medication. For example, when administering anticholinergics and antihistamines, monitor for anticholinergic side effects, especially in elderly clients.
Evaluation
Monitor for improvement of nausea and vomiting and notify the provider if expected improvement does not occur so that other treatment can be initiated. Continue to monitor for dehydration. Teach the client these nonpharmacological interventions for nausea:
- Drink enough fluids to avoid dehydration. If you are having trouble keeping liquids down, drink sips of clear liquids every few minutes.
- Eat bland foods; stay away from spicy, fatty, or salty foods.
- Eat smaller meals more often.
- Avoid strong smells because they can sometimes trigger nausea and vomiting.
- If you are pregnant and have morning sickness, eat crackers before you get out of bed in the morning.[7]
Antiemetic Medication Classes
Anticholinergics
Scopolamine is an example of an anticholinergic medication that is often used to treat motion sickness or nausea and vomiting associated with surgical recovery from anesthesia and/or opiate analgesia.
Mechanism of Action: Anticholinergics block ACh receptors in the vestibular center and within the brain to prevent nausea-inducing stimuli to the chemoreceptor trigger zone (CTZ) and the vomiting center (VC). They also dry GI secretions and reduce smooth muscle spasms.
Indications: Anticholinergics, like scopolamine, are commonly used to prevent motion sickness and treat nausea and vomiting
Nursing Considerations: The scopolamine transdermal patch (see Figure 7.19)[8] is designed for continuous release of scopolamine following application to an area of intact skin on the head, behind the ear. The system is formulated to deliver approximately 1 mg of scopolamine to the systemic circulation over three days. It is contraindicated in clients with glaucoma. It has been reported to exacerbate psychosis, induce seizures, and cause drowsiness, confusion, and sedation. Due to its anticholinergic properties, scopolamine can decrease gastrointestinal motility and cause urinary retention. Scopolamine should be discontinued in clients who develop difficulty in urination. Scopolamine transdermal patches contain an aluminized membrane; skin burns have been reported at the application site in clients wearing an aluminized transdermal system during an MRI scan. Remove scopolamine transdermal patches before undergoing an MRI.

Application instructions:
- Only wear one transdermal system at any time.
- Do not cut the transdermal system.
- Apply the transdermal system to the skin in the postauricular area (hairless area behind one ear).
- After the transdermal system is applied on the dry skin behind the ear, wash hands thoroughly with soap and water and dry hands.
- If the transdermal system becomes displaced, discard the transdermal system, and apply a new transdermal system on the hairless area behind the other ear.
- For surgeries other than cesarean section, apply one scopolamine transdermal system the evening before scheduled surgery. Remove the transdermal system 24 hours following surgery.
Side Effects/Adverse Effects: Anticholinergics have potential side effects such as dry mouth, constipation, blurred vision, confusion, and memory impairment, especially in elderly clients.
Health Teaching & Health Promotion: Scopolamine transdermal patches may impair the mental and/or physical abilities required for the performance of hazardous tasks such as driving a motor vehicle, operating machinery, or participating in underwater sports. Concomitant use of other drugs (e.g., alcohol, sedatives, hypnotics, opiates, and anxiolytics) that cause central nervous system (CNS) adverse reactions, or that have anticholinergic properties, may increase this impairment. Inform clients not to operate motor vehicles or other dangerous machinery or participate in underwater sports until they are reasonably certain that scopolamine does not affect them adversely. Scopolamine can cause temporary dilation of the pupils, resulting in blurred vision if it comes in contact with the eyes. Advise clients to wash their hands thoroughly with soap and water and dry their hands immediately after handling the transdermal system. Upon removal, fold the used transdermal system in half with the sticky side together, and discard in household trash in a manner that prevents accidental contact or ingestion by children, pets, or others.[9]
Antihistamines
Meclizine is an example of an antihistamine that is often used to treat motion sickness.
Mechanism of Action: Antihistamines block H1 receptors in the vestibular center and may also block acetylcholine (ACh).
Indications: Antihistamines such as meclizine block the action of histamine in the body. When H1 receptors are blocked in the vestibular center, this prevents motion sickness and nausea.
Nursing Considerations: Antihistamines are contraindicated in clients with glaucoma or an enlarged prostate gland. Dosage should be started one hour before travel begins.
Side Effects/Adverse Effects: Antihistamines have potential side effects such as drowsiness, dry mouth, blurred vision, and constipation. Some antihistamines can also interact with other medications or medical conditions.
Health Teaching & Health Promotion: Advise clients of the following:
- Do not exceed recommended dosage.
- Be advised that drowsiness may occur.
- Avoid alcohol, sedatives, and tranquilizers, which may increase drowsiness.
- Avoid alcoholic drinks.
- Be careful when driving a motor vehicle or operating machinery.[10]
Dopamine Antagonists
Prochlorperazine is an example of a dopamine antagonist used to treat nausea and vomiting. It can also be used as an antipsychotic medication.
Mechanism of Action: Prochlorperazine blocks dopamine in the chemoreceptor trigger zone (CTZ). It also calms the central nervous system and may also block acetylcholine.
Indications: Dopamine antagonists block the action of dopamine in the brain and can help treat nausea and vomiting.
Nursing Considerations: Prochlorperazine can be administered orally, intramuscularly, rectally or intravenously. It is contraindicated in children under age 2 or under 20 pounds. Severe side effects have occurred when used to treat psychosis.
Side Effects/Adverse Effects: Potential side effects are drowsiness, restlessness, dry mouth, constipation, and movement disorders, especially with long-term use.
Health Teaching & Health Promotion: Clients should be instructed to take medications as prescribed. They should avoid alcohol and other CNS depressants. Clients may experience increased photosensitivity, and extreme temperatures should be avoided. Clients should be advised that urine may turn pinkish to reddish-brown.[11]
Prokinetics
Metoclopramide is an example of a prokinetic medication (see Figure 7.20).[12]
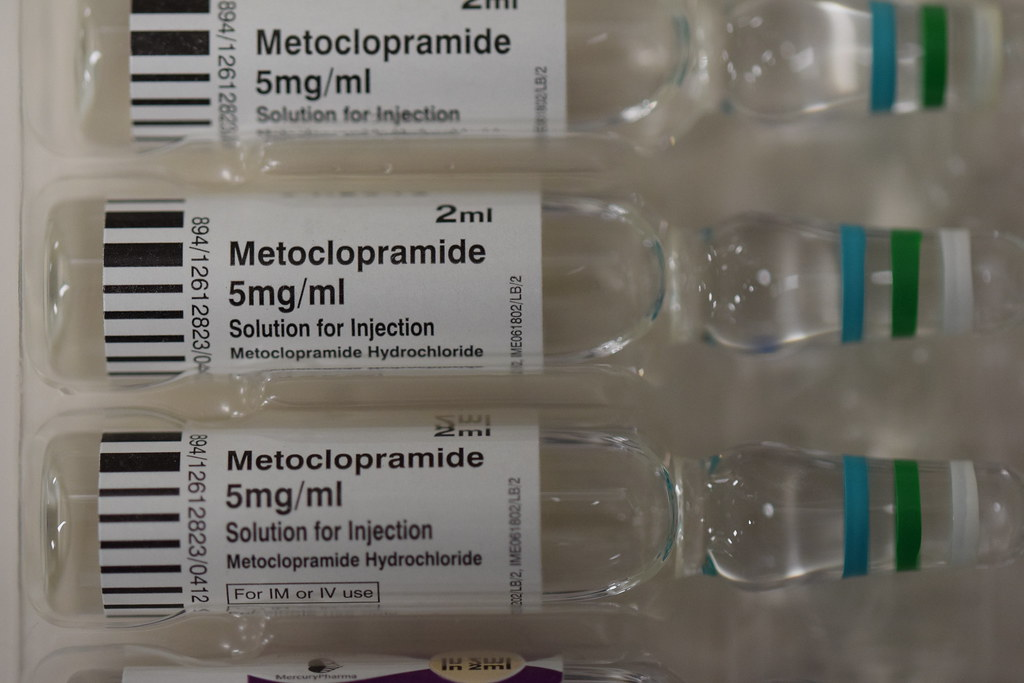
Mechanism of Action: Metoclopramide blocks dopamine and may also sensitize tissues to acetylcholine. It is used to promote peristalsis to empty the gastrointestinal tract and thus reduce nausea.
Indications: Metoclopramide is a dopamine antagonist that can be used to treat gastrointestinal disorders by improving motility.
Nursing Considerations: Metoclopramide can be administered orally, intramuscularly, and intravenously. The onset of pharmacological action of metoclopramide is 1 to 3 minutes following an intravenous dose, 10 to 15 minutes following intramuscular administration, and 30 to 60 minutes following an oral dose. Pharmacological effects persist for 1 to 2 hours.
Metoclopramide should not be used whenever stimulation of gastrointestinal motility might be dangerous (e.g., in the presence of gastrointestinal hemorrhage, mechanical obstruction, or perforation). Metoclopramide is contraindicated in clients with pheochromocytoma because the drug may cause a hypertensive crisis. Metoclopramide should not be used in epileptics or clients receiving other drugs that are likely to cause extrapyramidal reactions because the frequency and severity of seizures or extrapyramidal reactions may be increased. Rare reports of neuromalignant syndrome have occurred.
Side Effects/Adverse Effects: Metoclopramide has potential side effects, such as drowsiness, restlessness, movement disorders, and an increased risk of depression and suicidal thoughts, especially with long-term use.
Health Teaching & Health Promotion: Teach clients to immediately inform the health care provider if they experience new feelings of depression or abnormal muscle movements they cannot control such as the following:
- Lip smacking, chewing, or puckering of the mouth
- Frowning or scowling
- Sticking out the tongue
- Blinking and moving the eyes
- Shaking of the arms and legs[13]
Serotonin Antagonists
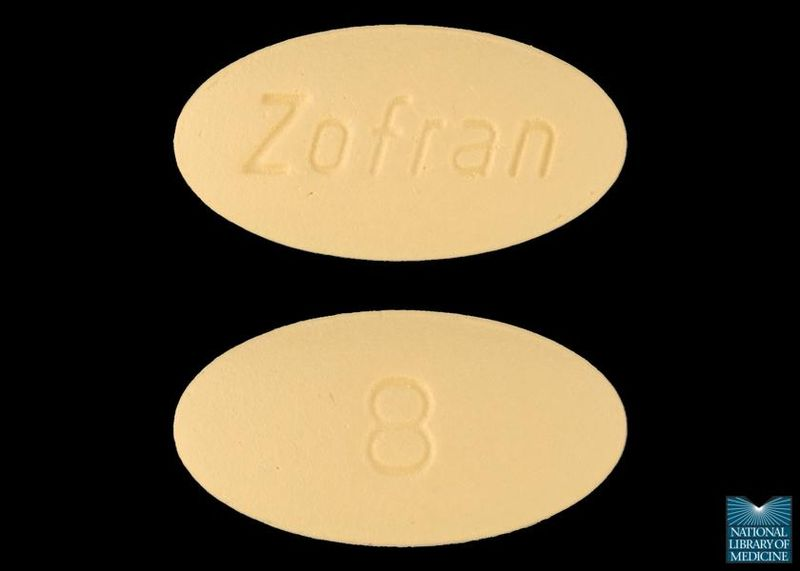
Ondansetron is an example of a serotonin (5HT) antagonist often used to treat severe nausea and vomiting associated with chemotherapy, postoperative nausea and vomiting, and hyperemesis during pregnancy. (See Figure 7.21[14] for an image of ondansetron blocking the 5-HT3 receptor.)
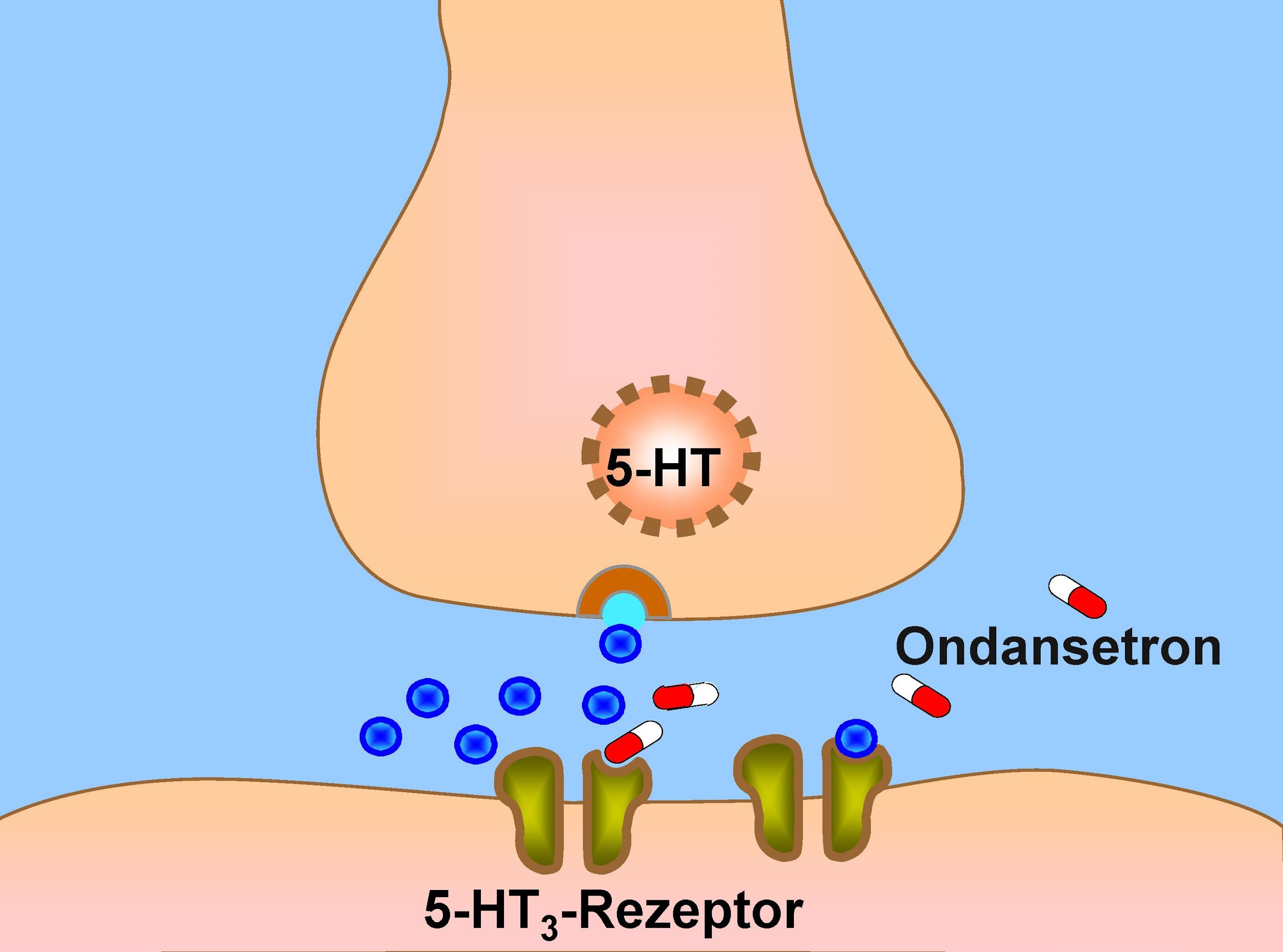
Mechanism of Action: Ondansetron blocks serotonin receptors in the GI tract, the chemoreceptor trigger zone (CTZ), and the vomiting center (VC). See Figures 7.22[15] and 7.23[16] for images of the injectable and oral formulations of ondansetron.
Indications: Serotonin antagonists, also known as serotonin blockers, are a class of drugs that block the action of serotonin, a neurotransmitter in the brain.
Nursing Considerations: Ondansetron is available as an orally disintegrating tablet and as an injectable for those clients too nauseated to tolerate oral medication. It is contraindicated with apomorphine. Serotonin syndrome can occur if administered concurrently with other serotonin antagonists or selective serotonin reuptake inhibitors. Ondansetron can cause headaches, drowsiness, constipation, fever, and diarrhea. A rare but serious adverse effect of ondansetron is QT prolongation that can cause an abnormal cardiac rhythm.
Side Effects/Adverse Effects: It is important to note that serotonin antagonists have potential side effects such as dizziness, headache, constipation, and nausea. Some serotonin antagonists can also interact with other medications or medical conditions.
Health Teaching & Health Promotion: Teach clients to immediately inform their health care provider if they experience a change in heart rate, light-headedness, or feel faint or have any signs and symptoms of hypersensitivity reactions such as fever, chills, rash, or breathing problems.[17]
Neurokinin Receptor Antagonists
Aprepitant is an example of a neurokinin antagonist used to prevent nausea and vomiting associated with chemotherapy and surgery.
Mechanism of Action: Aprepitant inhibits substance-P neurokinin receptors in the brain stem.
Indications: Neurokinin receptor antagonists are a class of drugs that block the action of substance P, a neuropeptide that plays a role in pain, inflammation, and other physiological processes.
Nursing Considerations: Aprepitant is usually administered concurrently with dexamethasone (a corticosteroid) and ondansetron. It can be administered orally or intravenously. It has clinically significant CYP3A4 drug interactions with medications, such as pimozide, diltiazem, and rifampin, and can decrease INR levels when taken concurrently with warfarin. It can also reduce the effectiveness of oral contraceptives.
Side Effects/Adverse Effects: Neurokinin receptor antagonists have potential side effects such as fatigue, dizziness, constipation, and decreased appetite.
Health Teaching & Health Promotion: Teach clients taking warfarin that they will need to monitor their INR levels more closely, which may require adjustment of the warfarin dosage, while taking aprepitant. Teach clients using an oral contraceptive to use backup birth control.[18]
Tetrahydrocannabinols (THC)
Dronabinol or medical marijuana is an example of a THC medication used to treat nausea in clients with cancer or AIDS (see Figures 7.24[19] and 7.25[20]).
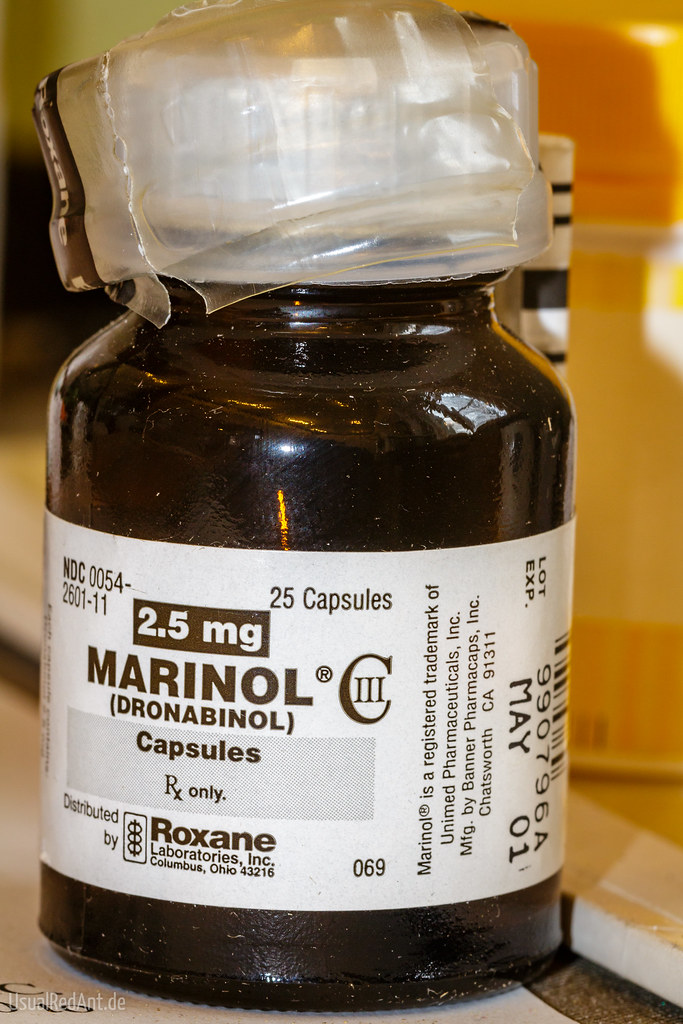

Mechanism of Action: THC has inhibitory effects in the cerebral cortex causing an alteration in mood and the body’s perception of its surroundings, which may relieve nausea and vomiting, as well as stimulate the appetite.
Indications: THC has antiemetic properties and can be used to treat nausea and vomiting associated with chemotherapy or other medical conditions.
Nursing Considerations: THC will cause a dose-related responses such as elation, heightened awareness, and laughing. THC should be used cautiously in elderly clients because they may be more sensitive to the neurological, psychoactive, and postural hypotensive effects of the drug. In general, dose selection for an elderly client should be cautious, usually starting at the low end of the dosing range.
Side Effects/Adverse Effects: THC has potential side effects, including impaired memory and concentration, impaired motor coordination, anxiety, and paranoia. Additionally, THC can be habit-forming and may have psychoactive effects that can impair daily activities.
Health Teaching & Health Promotion: Teach clients to not drive, operate machinery, or engage in any hazardous activity when using THC. Keep out of reach of children and pets.[21]
Herbal and Vitamin Supplements
Ginger has been used in traditional Indian and Chinese medicine as an antiemetic. Although its mechanism of action is not completely understood, ginger is thought to antagonize the 5HT and cholinergic receptors and may have direct activity on the gastrointestinal tract. Although ginger can cause reflux and heartburn and may potentially cause bleeding because of its anticoagulant effects, dosages of up to 2 grams per day in divided doses of 250 mg are considered safe even in pregnant women. Pyridoxine (vitamin B6) has also been recommended for treating nausea and vomiting in pregnancy. Typical dosages of pyridoxine 10 to 25 mg every eight hours cause minimal adverse effects.[22]
Now let’s take a closer look at the medication grid comparing medications used to treat nausea. See Table 7.5b.[23]
Medication grids are intended to assist students to learn key points about each medication. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. Basic information related to each class of medication is outlined below. Detailed information on a specific medication can be found for free at DailyMed. On the home page, enter the drug name in the search bar to read more about the medication. Prototype/generic medications listed in the grids below are also linked to a DailyMed page.
Table 7.5b Antiemetics Medication Grids
| Class/Subclass | Prototype/Generic | Nursing Considerations | Therapeutic Effects | Side/Adverse Effects |
|---|---|---|---|---|
| Anticholinergic | scopolamine | Apply patch to hairless skin behind ear for 3 days or apply the night before surgery and remove 24 hours later
Do not cut patch After application, thoroughly wash and dry hands Remove before an MRI Contraindicated in clients with glaucoma |
Prevent or reduce nausea and vomiting associated with motion sickness or surgery | Monitor for anticholinergic effects such as decreased GI motility and urinary retention
Discontinue if it exacerbates psychosis or causes seizures or cognitive impairment |
| Antihistamine | meclizine | Contraindicated in clients with glaucoma or an enlarged prostate gland
Dosage should be started one hour before travel begins |
Prevent or reduce nausea and vomiting associated with motion sickness | May cause drowsiness |
| Dopamine Antagonist | prochlorperazine | Can be administered PO, IM, PR, or IV | To control nausea and vomiting associated with surgery | Drowsiness, dizziness, amenorrhea, blurred vision, skin reactions, and hypotension may occur |
| Prokinetic | metoclopramide | Can be administered PO, IM, and IV
Onset of action is 1 to 3 minutes following an IV dose, 10 to 15 minutes following IM administration, and 30 to 60 minutes following an oral dose Pharmacological effects persist for 1 to 2 hours |
To prevent or treat nausea and vomiting associated with surgery or chemotherapy | Restlessness, drowsiness, fatigue, depression, and suicide ideation
Should be immediately discontinued if symptoms of tardive dyskinesia (abnormal muscle movements) or neuromalignant syndrome occur (hyperthermia, muscle rigidity, altered consciousness, irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac arrhythmias) |
| Serotonin Antagonist | ondansetron | Can be administered as oral disintegrating tablet, PO, or IV | Prevention or treatment of severe nausea and vomiting associated with surgery, chemotherapy, or hyperemesis in pregnancy | Hypersensitivity reactions, including fever, chills, rash, or breathing problems
Headache, drowsiness, constipation, fever, and diarrhea May cause QT prolongation Can cause serotonin syndrome if given concurrently with other serotonin antagonists or SSRIs |
| Neurokinin Receptor Antagonist | aprepitant | Can be administered PO or IV | Prevention of nausea and vomiting associated with chemotherapy and surgery | Hypersensitivity reaction, such as hives, rash, and itching; skin peeling or sores; or difficulty in breathing or swallowing
If taking warfarin, increase monitoring of INR levels If taking oral contraceptives, use a backup method of birth control |
| THC | dronabinol or medical marijuana | Administered PO
Most clients respond to 5 mg three or four times daily Dosage may be escalated during a chemotherapy cycle or at subsequent cycles, based on initial results |
For treatment of nausea and vomiting associated with cancer chemotherapy when other treatment fails | Use cautiously in elderly clients because they may be more sensitive to the neurological, psychoactive, and postural hypotensive effects of the drug. In general, dose selection for an elderly client should be cautious, usually starting at the low end of the dosing range |
Critical Thinking Activity 7.5
A nurse is caring for a client who underwent surgery earlier today and is experiencing nausea and vomiting. The original post-op orders included prochlorperazine, but the client continues to experience vomiting despite receiving this medication. The nurse calls the provider and receives a new order for ondansetron orally dissolving tablets 8 mg three times daily as needed.
- How will the nurse assess for symptoms of dehydration?
- When administering the medication, the client states, “This tastes terrible! Why can’t I have a normal pill to swallow?” What is the nurse’s best response?
- What other measures should the nurse teach the client to reduce feelings of nausea and avoid dehydration?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” section at the end of the book.
- Bashashati, M., & McCallum, R. (2014). Neurochemical mechanisms and pharmacologic strategies in managing nausea and vomiting related to cyclic vomiting syndrome and other gastrointestinal disorders. European Journal of Pharmacology, 772, 79. https://doi.org/10.1016/j.ejphar.2013.09.075 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2019 October 23]. Nausea and vomiting; [updated 2019 February 7; reviewed 2016 March 17; cited 2019 October 27]. https://medlineplus.gov/nauseaandvomiting.html ↵
- Bashashati, M., & McCallum, R. (2014). Neurochemical mechanisms and pharmacologic strategies in managing nausea and vomiting related to cyclic vomiting syndrome and other gastrointestinal disorders. European Journal of Pharmacology, 772, 79. https://doi.org/10.1016/j.ejphar.2013.09.075 ↵
- Becker, D. E. (2010). Nausea, vomiting, and hiccups: A review of mechanisms and treatment. Anesthesia Progress, 57(4), 150–157. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3006663/ ↵
- Becker, D. E. (2010). Nausea, vomiting, and hiccups: A review of mechanisms and treatment. Anesthesia Progress, 57(4), 150–157. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3006663/ ↵
- Bashashati, M., & McCallum, R. (2014). Neurochemical mechanisms and pharmacologic strategies in managing nausea and vomiting related to cyclic vomiting syndrome and other gastrointestinal disorders. European Journal of Pharmacology, 772, 79. https://doi.org/10.1016/j.ejphar.2013.09.075 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2019 October 23]. Nausea and vomiting; [updated 2019 February 7; reviewed 2016 March 17; cited 2019 October 27]. https://medlineplus.gov/nauseaandvomiting.html ↵
- “Scopoderm 278:365” by Andreas Nilsson is licensed under CC BY-NC-ND 2.0 ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- “Metoclopramide” by John Campbell is licensed under CC0 ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- “Eichelbaum2.jpg” by Michel Eichelbaum is licensed under CC BY-SA 3.0 DE ↵
- “000817lg Zofran 8 MG Oral Tablet.jpg” by NLM is licensed under CC0 ↵
- “Ondansetron (1)” by M is licensed under CC BY-NC 2.0 ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- “Marinol - Dronabinol” by Steffen Geyer is licensed under CC BY-NC 2.0 ↵
- “Medical Marijuana” by Circe Denyer is licensed under CC0 ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
- Flake, Z., Linn, B., & Hornecker, J. (2015). Practical selection of antiemetics in the ambulatory setting. American Family Physician, 91(5), 293-296. https://pubmed.ncbi.nlm.nih.gov/25822385/ ↵
- This work is a derivative of DailyMed by U.S. National Library of Medicine in the Public Domain. ↵
Infection of the intestines.
Blood in the vomit.
Area in the brain that responds directly to toxins in the bloodstream and also receives stimuli from several other locations in the body that stimulates the vomiting center.
A structure in the medulla oblongata in the brainstem that controls vomiting. Its location in the brain also allows it to play a vital role in the control of autonomic functions by the central nervous system.
An area located within the inner ear that gives a sense of balance and spatial orientation for the purpose of coordinating movement with balance.
An area in the brain that initiates vomiting by inhibiting peristalsis and producing retro peristaltic contractions beginning in the small bowel and ascending into the stomach. It also produces simultaneous contractions in the abdominal muscles and diaphragm that generate high pressures to propel the stomach contents upwards.
Symptoms associated with serotonin syndrome may include the following combination of signs and symptoms: mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, with or without gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
Tetrahydrocannabinoids found in marijuana.

