9.12 Other Nervous System Disorders
Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a neurological disorder that affects motor neurons and the control of voluntary muscle movement and breathing. As motor neurons degenerate and die, they stop sending messages to the muscles, causing them to weaken, twitch, and shrink. Eventually, the brain loses its ability to control voluntary movements, such as walking, talking, chewing, and breathing. However, cognitive abilities are not affected. Medications are available that may prolong survival, reduce the rate of decline, or help manage symptoms, but there is no known treatment to cure ALS.[1]
Autonomic Dysreflexia
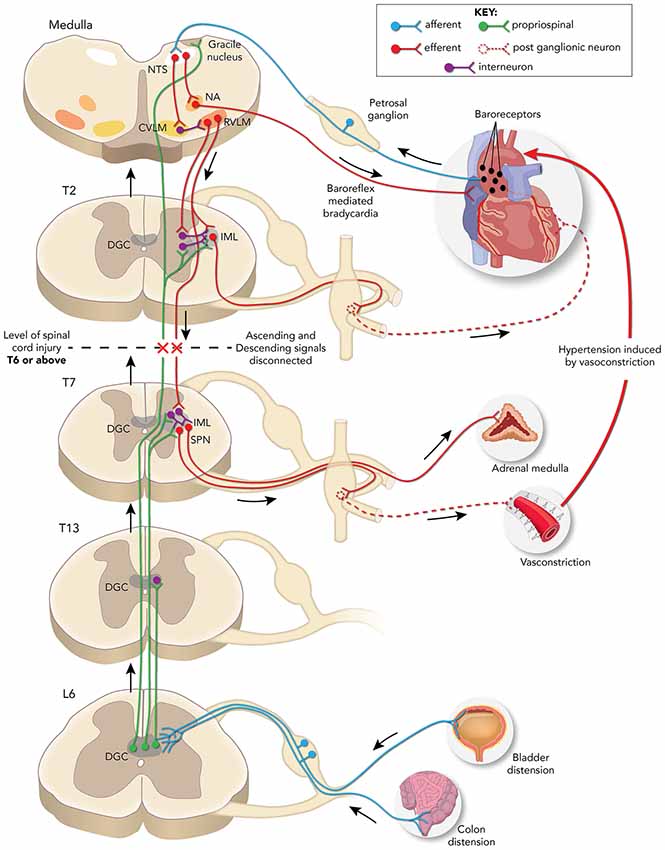
Autonomic dysreflexia is a medical emergency that occurs in clients who have sustained a spinal cord injury above T6. It is manifested by an exaggerated autonomic reflex response that is most often triggered by bowel or bladder distension such as constipation, impaction or urinary retention, or tight or restrictive clothing.
See Figure 9.31[2] for an illustration of neuronal pathways disrupted/rerouted by complete spinal cord injury above the sixth thoracic (T6) spinal level associated with the development of autonomic dysreflexia evoked by pelvic visceral distension.
Signs and symptoms of autonomic dysreflexia include the following:
- Severe headache
- Increased in blood pressure (hypertension)
- Bradycardia
- Flushing
- Profuse sweating
Management of autonomic dysreflexia focuses on removing the trigger, such as loosening restrictive clothing, emptying bowel or bladder, and elevating the head of the bed (while keeping correct body alignment).
Ongoing management includes frequent assessing of GI/GU systems, utilizing a kinetic bed to promote blood flow, providing range-of-motion exercise, applying sequential compression devices, protecting skin integrity, and promoting bowel and bladder training. Encourage the client to keep their bladder empty and their urine dilute and acidic to prevent urinary tract infection, a common cause of life-threatening sepsis.
View a supplementary YouTube[3] video on autonomic dysreflexia: Autonomic Dysreflexia.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is a common neurological and musculoskeletal disorder that occurs when the median nerve, which runs from the forearm into the palm of the hand, becomes pressed or squeezed at the wrist. The median nerve passes through the carpal tunnel, a narrow, rigid passageway of ligament and bones at the base of the hand. The median nerve provides feeling to the thumb, index, middle finger, and part of the ring finger. Compression of this nerve causes the symptoms of numbness, tingling, weakness, and pain in these fingers.[4]
See Figure 9.32[5] for an illustration of carpal tunnel syndrome.
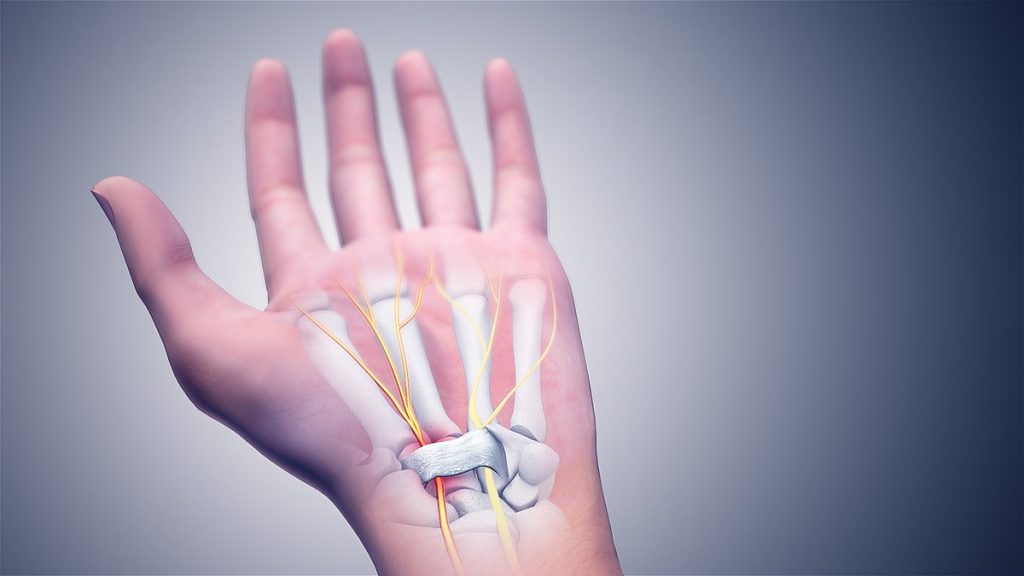
Carpal tunnel syndrome may be diagnosed with a nerve conduction study that measures how quickly impulses are transmitted along a nerve. An electromyography test may also be used, where a fine needle is inserted into a muscle, and electrical activity is viewed on a screen to determine the severity of damage to the median nerve. Treatment includes wearing a splint at night while sleeping to keep the wrist straight and medications to reduce inflammation in the carpal tunnel. If these treatments are not effective, carpal tunnel release surgery is performed to release pressure on the nerve.[6]
Guillain Barre Syndrome
Guillain-Barré syndrome (GBS) is a rare autoimmune disease that causes muscle weakness and sometimes paralysis. Early symptoms of GBS include weakness and tingling in both legs that progress to the arms and upper body. The weakness can increase to paralysis. Symptoms can progress over hours, days, or weeks. Most people start to recover two to three weeks after symptoms first start. Recovery may take as little as a few weeks or as long as a few years. Many people recover fully, but some have permanent nerve damage, and GBS can result in death if the respiratory muscles are affected.[7]
Infection with Campylobacter jejuni, a common cause of diarrhea, is also a common cause of GBS. Influenza and other viruses like cytomegalovirus and Epstein-Barr virus can also cause GBS.[8]
Treatment of GBS includes plasma exchange (a procedure that removes and replaces the liquid part of the blood) and high-dose immunoglobulin therapy.[9]
View a supplementary YouTube video[10] on Guillain-Barre syndrome: Understanding Guillain-Barré Syndrome.
Mental Health Disorders
Many mental health disorders, such as anxiety, bipolar disorder, obsessive compulsive disorder (OCD), and schizophrenia can be caused by imbalanced levels of neurotransmitters. Mental health disorders are treated with a combination of medications, psychotherapy, and support groups.
Read additional information about mental health disorders in Open RN Nursing: Mental Health and Community Concepts.
Migraines
A migraine is a type of headache characterized by recurrent attacks of moderate to severe throbbing and pulsating pain on one side of the head. Untreated attacks last from 4 to 72 hours. Additional symptoms such as nausea, vomiting, or sensitivity to light and sound may occur with a migraine. There are two main types of migraines called a classic migraine (with an aura) and a common migraine (without an aura). An aura is a group of neurologic symptoms considered a warning sign for the onset of a migraine and include the following[11],[12]:
- Temporary blind spots or colored spots
- Blurred vision
- Eye pain
- Seeing stars, zigzag lines, or flashing lights
- Tunnel vision (only able to see objects close to the center of the field of view)
After a migraine, individuals often feel exhausted or confused for up to 24 hours.[13]
Pathophysiology
A migraine is caused by abnormal brain activity that can have several triggers. The causes of a migraine remain unclear, but medical experts believe it involves nerve pathways and chemical changes that affect blood flow in the brain and surrounding tissues.
Triggers of migraine headaches include the following[14]:
- Caffeine withdrawal
- Changes in hormone levels during a menstrual cycle or due to birth control pills
- Changes in sleep patterns, such as not getting enough sleep
- Drinking alcohol
- Exercise or other physical stress
- Loud noises or bright lights
- Missed meals
- Odors or perfumes
- Smoking or exposure to smoke
- Stress and anxiety
- Foods, such as chocolate, dairy foods (especially certain cheeses), onions, and peanuts and other nuts and seeds
- Foods with monosodium glutamate (MSG) or tyramine, such as red wine; aged cheese; smoked fish; chicken livers; figs; certain beans; meats containing nitrates (bacon, hot dogs, salami, cured meats); and processed, fermented, pickled, or marinated foods
Migraine headaches tend to first appear between the ages of 10 and 45 and occur more often in women than men. There may be a genetic component with family history being a risk factor. There are no specific diagnostic tests for migraines.[15]
Treatment
There is no cure for migraines. The goal of treatment is to prevent symptoms by avoiding triggers and immediately managing symptoms when they occur. Treatment includes lifestyle changes, quick relief measures, medication therapy, biofeedback, and relaxation training.[16],[17]
Lifestyle changes include the following[18]:
- Healthier sleep habits, such as getting enough sleep and going to bed at the same time each night
- Healthier eating habits, including not skipping meals and avoiding food triggers
- Managing stress
- Losing weight if overweight
Quick relief measures that can be implemented at the onset of a migraine include napping or resting with eyes closed in a quiet, darkened room; placing a cool cloth or ice pack on the forehead; and drinking lots of fluid, especially if the migraine is accompanied by vomiting. Small amounts of caffeine may help during early stages of a migraine.[19]
Medication therapy is divided into acute and preventative treatment. Acute medications are taken as soon as symptoms occur to relieve pain and restore function. Preventive treatment involves taking medications daily to prevent migraines or reduce their severity. Acute treatment for migraines may include the following medications[20]:
- Nonprescription analgesics or over-the-counter drugs such as ibuprofen, aspirin, or acetaminophen can ease mild to moderate pain. Combination analgesics involve a mix of medications such as acetaminophen and caffeine.
- Ergot derivative drugs bind to serotonin receptors on nerve cells and decrease the transmission of pain messages along nerve fibers. They are most effective during the early stages of migraine.
- Triptan medications are used for moderate to severe migraine pain. They increase serotonin levels in the brain, causing blood vessels to constrict and lowering the pain threshold.
Preventative treatment includes the following[21]:
- Anticonvulsants increase levels of certain neurotransmitters that dampen pain impulses.
- Beta-blockers and calcium channel blockers help stabilize blood vessel walls and prevent them from narrowing or widening, which affects blood flow to the brain and can cause a migraine.
- Antidepressants increase the production of serotonin and also may affect levels of other chemicals, such as norepinephrine and dopamine.
- Calcitonin gene-related peptide (CGRP) agents.
- Botulinum toxin type A (Botox) injections to reduce migraine attacks if they occur more than 15 days a month.
- Vitamins and minerals like riboflavin or magnesium.
Biofeedback and relaxation training can also be used to help individuals cope with and control the development of pain and the body’s response to stress.
Spinal Cord Injury
A spinal cord injury (SCI) refers to damage to the bundle of nerves and nerve fibers that sends and receives signals from the brain. The spinal cord extends from the lower part of the brain down through the lower back. SCI can be caused by direct injury to the spinal cord or from damage to the vertebrae that surround the spinal cord. This damage can cause temporary or permanent changes in feeling, movement, strength, and body functions below the site of injury.[22]
Motor vehicle accidents and serious falls are the most common causes of SCI. Other causes include gunshot wounds, sports injuries, surgical injury, industrial accidents, and diseases and conditions that can damage the spinal cord. Risk factors include age (either between the ages of 16 and 30 or older than 65 for serious falls), alcohol use, and not wearing proper gear, such as a seat belt or protective sports equipment.
The symptoms of SCO depend on the extent and location of the injury. The higher up on the spinal cord an injury occurs, the greater affect on the body. For example, an injury higher on the spinal cord can cause tetraplegia (paralysis in most of the body and all limbs). An injury that occurs lower on the spinal cord may only affect the lower body and legs, referred to as paraplegia. Paralysis may occur immediately upon injury or develop over time from bleeding and swelling in the spinal cord resulting in cell death.[23]
Read more information about “Paralysis” in the “Musculoskeletal System Alterations” chapter.
SCI may be described as complete or incomplete[24]:
- An incomplete injury means the spinal cord is still able to send some messages to or from the brain. People with incomplete injuries still have some feeling, function, and muscle control below the site of their injury.
- A complete injury means that there is no nerve communication below the injury site, so muscle control, feeling, and function below the injury are lost.
Medical tests for SCI are as follows[25]:
- Magnetic resonance imaging (MRI) can show brain and spinal trauma from injury, herniated discs (problems with the cartilage located between the vertebrae), vascular (blood vessel) irregularities, bleeding, inflammation that might compress the spine and spinal cord, and injury to the ligaments that support the cervical spine.
- Computerized tomography (CT) scans can detect bone fractures, bleeding, and spinal stenosis (narrowing of the spinal canal).
- X-rays can show vertebrae misalignment and fractures.
SCI can result in the following problems requiring treatment[26]:
- Breathing problems: About one third of people with an SCI will need temporary or permanent assistance breathing, and some require mechanical ventilation. Injury to the spinal cord between the C1-C4 can stop breathing because these nerves cause the diaphragm to move and the lungs to expand.
- Pneumonia: Respiratory complications are the leading cause of death in people with SCI, commonly as a result of pneumonia. Individuals requiring a mechanical ventilator are at increased risk of developing pneumonia. Pneumonia can often be preventing with aspiration precautions.
- Circulatory problems: Changes in circulation can lead to unstable blood pressure, arrhythmias, and blood clots due to blood flow stasis in the large veins in the legs. Anticoagulants and compression stockings help reduce the risk for blood clots.
- Stiffness and changes in muscle tone: Reflexes may become exaggerated over time in clients with SCI, causing muscle stiffness and an increase in muscle tone (spasticity) that may require special treatment. Muscles below the injury site may deteriorate when they are not used.
- Autonomic dysreflexia: Autonomic dysreflexia is a life-threatening reflex action that primarily affects clients with injuries to the neck or upper back. Symptoms may include flushing or sweating, a pounding headache, anxiety, sudden increase in blood pressure, vision changes, or goose bumps on the arms and legs. If possible, the person should be kept in a sitting position to keep blood flowing to the legs and feet and help reduce blood pressure. Read more about this condition in the “Autonomic Dysreflexia” subsection.
- Pressure Injuries: Pressure injuries may occur from continuous pressure on the skin and reduced blood flow to the area, especially in clients with paraplegia and tetraplegia. Repositioning every one to two hours can prevent the development of pressure injuries.
- Pain: Some people with SCI develop neurogenic pain, an intense burning or stinging sensation that may be constant or intermittent. Neurogenic pain can be triggered by a variety of factors and may be felt in parts of the body that have otherwise lost sensation. Treatments to manage chronic pain include medications, acupuncture, spinal or brain electrical stimulation, and surgery.
- Bladder and bowel problems: Individuals with SCI may require a urinary catheter and a bowel management program with routine use of laxatives.
- Sexual function: Depending on the severity and location of the SCI, sexual function and fertility may be affected. A urologist and other specialists can suggest options to support sexual functioning and health.
- Depression: People living with SCI may develop depression due to lifestyle changes after the injury. Therapy and medicine can help treat depression and other mental health conditions.
Rehabilitation programs for people with SCI combine physical therapies and counseling designed to provide social and emotional support to optimize the person’s independence and quality of life. The rehabilitation team may include social workers, physical and occupational therapists, nurses, psychologists, vocational counselors, nutritionists, a case worker, and other specialists.[27]
Traumatic Brain Injury
A traumatic brain injury (TBI) can be caused by a forceful bump, blow, or jolt to the head or body or from an object that pierces the skull and enters the brain. Some types of mild TBI, like a concussion, can cause temporary or short-term problems with normal brain function, including problems with how the person thinks, understands, moves, communicates, and acts. A serious TBI can lead to severe, permanent disability or death.[28]
Symptoms of a TBI may include loss of consciousness, headache, blurred vision, unequal pupil size, nausea, vomiting, clear fluids draining from the nose or ears, photophobia, tinnitus, or other neurological symptoms. TBI is diagnosed using standardized concussion tools and diagnostic testing such as CT scans and MRIs, if necessary.[29]
There are many types of TBIs, including concussions, hematomas, skull fractures, and chronic traumatic encephalopathy[30]:
- Concussion: A concussion is a temporary, mild TBI that may take several months to heal. A concussion can be caused by a blow to the head, sports injury, fall, motor vehicle accident, weapons blast, or a rapid acceleration/deceleration of the brain within the skull, such as an infant being shaken.
- Hematoma: A hematoma refers to bleeding in and around the brain caused by a ruptured blood vessel. Different types of hematomas form depending on where the blood collects. For example, subdural hematomas are common in the elderly after experiencing a TBI from a fall. It involves bleeding below the dura mater, the membrane directly under the skull.
- Skull fracture: Skull fractures are cracks in one or more of the bones that form the skull. They can cause damage to the membranes, blood vessels, and brain under the fracture. Helmets and seat belts significantly help prevent skull fractures and TBI.
- Chronic traumatic encephalopathy: Chronic traumatic encephalopathy occurs in people with extraordinary exposure to multiple blows to the head, such as boxers and football players. It is a delayed consequence after many years and a progressive neurological disorder associated with symptoms that may include problems with thinking, understanding, and communicating; motor disorders (affecting movement); problems with impulse control and depression; confusion; and irritability.
Treatments are based on the cause and severity of the TBI. For example, mild concussions are commonly treated with rest and pain reliever medications, whereas severe TBIs may require surgery to drill a hole into the skull to drain fluids to relieve pressure inside the skull.[31]
- National Institute of Neurological Disorders and Stroke (n.d.). Amyotrophic lateral sclerosis (ALS). https://www.ninds.nih.gov/health-information/disorders/amyotrophic-lateral-sclerosis-als ↵
- “AutoDys2019.jpg” by Felicia M. Michael, Samir P. Patel and Alexander G. Rabchevsky is licensed under CC BY 4.0 ↵
- Dr. Matt & Dr. Mike. (2020, September 8). Autnomic dysreflexia [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=eocOmytfg8s ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (n.d.). Carpal tunnel syndrome. https://www.niams.nih.gov/health-topics/carpal-tunnel-syndrome ↵
- “Carpal_Tunnel_Syndrome.jpg” by www.scientificanimations.com is licensed under CC BY-SA 4.0 ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (n.d.). Carpal tunnel syndrome. https://www.niams.nih.gov/health-topics/carpal-tunnel-syndrome ↵
- Center for Disease Control. (n.d.). Campylobacter: Guillain-Barré syndrome. https://www.cdc.gov/campylobacter/signs-symptoms/guillain-barre-syndrome.html ↵
- Center for Disease Control. (n.d.). Campylobacter: Guillain-Barré syndrome. https://www.cdc.gov/campylobacter/signs-symptoms/guillain-barre-syndrome.html ↵
- Center for Disease Control. (n.d.). Campylobacter: Guillain-Barré syndrome. https://www.cdc.gov/campylobacter/signs-symptoms/guillain-barre-syndrome.html ↵
- Zero to Finals. (2021, January 10). Understanding Guillain-Barré syndrome [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=KUEunZYZgII ↵
- MedlinePlus [Internet]. (2023). Migraine. https://medlineplus.gov/ency/article/000709.htm ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine ↵
- MedlinePlus [Internet]. (2023). Migraine. https://medlineplus.gov/ency/article/000709.htm ↵
- MedlinePlus [Internet]. (2023). Migraine. https://medlineplus.gov/ency/article/000709.htm ↵
- MedlinePlus [Internet]. (2023). Migraine. https://medlineplus.gov/ency/article/000709.htm ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine ↵
- MedlinePlus. (n.d.). Migraine. https://medlineplus.gov/ency/article/000709.htm ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Migraine. https://www.ninds.nih.gov/health-information/disorders/migraine ↵
- National Institute of Neurological Diseases and Stroke. (n.d.). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury ↵
- National Institute of Neurological Diseases and Stroke. (n.d.). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury ↵
- National Institute of Neurological Diseases and Stroke. (n.d.). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury ↵
- National Institute of Neurological Diseases and Stroke. (n.d.). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury ↵
- National Institute of Neurological Diseases and Stroke. (n.d.). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury ↵
- National Institute of Neurological Diseases and Stroke. (n.d.). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury ↵
- National Institute of Neurological Disorders and Stroke. (2023). Traumatic brain injury (TBI). National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi ↵
- National Institute of Neurological Disorders and Stroke. (2023). Traumatic brain injury (TBI). National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi ↵
- National Institute of Neurological Disorders and Stroke. (2023). Traumatic brain injury (TBI). National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi ↵
- National Institute of Neurological Disorders and Stroke. (2023). Traumatic brain injury (TBI). National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi ↵
Also known as Lou Gehrig's disease, is a neurological disorder that affects motor neurons and the control of voluntary muscle movement and breathing.
A medical emergency that occurs in clients who have sustained a spinal cord injury above T6.
A common neurological and musculoskeletal disorder that occurs when the median nerve, which runs from the forearm into the palm of the hand, becomes pressed or squeezed at the wrist.
A rare autoimmune disease that causes muscle weakness and sometimes paralysis.
A type of headache characterized by recurrent attacks of moderate to severe throbbing and pulsating pain on one side of the head.
Damage to the bundle of nerves and nerve fibers that sends and receives signals from the brain.
Paralysis in most of the body and all limbs.
An injury that occurs lower on the spinal cord may only affect the lower body and legs.
The spinal cord is still able to send some messages to or from the brain.
Means that there is no nerve communication below the injury site so muscle control, feeling, and function below the injury is lost.
Narrowing of the spinal canal.
An intense burning or stinging sensation that may be constant or intermittent.
Can be caused by a forceful bump, blow, or jolt to the head or body or from an object that pierces the skull and enters the brain.
A temporary, mild TBI that may take several months to heal.
Bleeding in and around the brain caused by a ruptured blood vessel.
Cracks in one or more of the bones that form the skull.
Occurs in people with extraordinary exposure to multiple blows to the head, such as boxers and football players.

