10.10 Other Musculoskeletal Disorders
Additional musculoskeletal disorders are briefly discussed in this section.
Bone Cancer
There are three types of primary bone cancers: osteosarcoma, Ewing sarcoma, and chondrosarcoma. These are considered primary cancers because they originate in the bones. Osteosarcoma and Ewing sarcomas are cancers found in children, teenagers, and young adults. Ewing sarcoma is considered to be the more aggressive of the two cancers because it tends to metastasize quickly. Osteosarcoma is the most common type of bone cancer, and it begins in the tissues of growing bones. Chondrosarcoma develops in cells that produce cartilage and affects adults.
Bone cancer can also be caused by cancer that has metastasized from other areas of the body. For example, breast, lung, and prostate cancer commonly cause bone metastasis.
Symptoms of bone cancer may include fatigue, unintended weight loss, bone pain, swelling, tenderness, and weakened bone leading to fractures. Diagnostic testing may include a bone scan, X-ray, CT scan, MRI, PET scan, and bone biopsy. Treatment is based on the type of cancer, the stage of the cancer, and the client’s overall health and preferences. For example, some bone cancers are treated with surgery; some are treated with surgery and chemotherapy; and others are treated with surgery, chemotherapy, and radiation therapy.[1]
Cerebral Palsy
Cerebral palsy (CP) is a group of disorders that affects the ability to move and maintain balance and posture. “Cerebral” means having to do with the brain, and “palsy” means weakness or problems with using the muscles. CP is caused by abnormal brain development or damage to the developing brain that affects the ability to control muscles.[2]
The symptoms of CP vary from person to person. A person with severe CP might require the use of special equipment to walk or might not be able to walk at all and need lifelong care. A person with mild CP, on the other hand, might walk a little awkwardly, but otherwise not require specialized care. Doctors classify CP according to the main type of movement disorder involved. Depending on which areas of the brain are affected, one or more of the following movement disorders can occur[3]:
- Spasticity: Stiff muscles
- Dyskinesia: Uncontrollable movements
- Ataxia: Poor balance and coordination
There is no cure for CP, but treatment can improve the quality of life for people who have the condition. After CP is diagnosed, a team of health professionals works with the child and family to develop a plan to help the child reach their optimal potential. Common treatments include medications; surgery; braces; and physical, occupational, and speech therapy.[4]
See Figure 10.39[5] for an image of David Smith who has cerebral palsy and is a Paralympian. Paralympians are athletes with a range of impairments who compete in the Paralympics, a competition similar to the Olympics. Paralympic athletes inspire people around the world with their performances and focus on moving forward and never giving up.[6]

Clubfoot
Clubfoot is a congenital condition that causes the foot and lower leg to turn inward and downward. See Figure 10.40[7] for an image of an infant with a clubfoot. Clubfoot can range from mild and flexible to severe and rigid. Treatment by an orthopedic specialist involves using repeated applications of casts beginning soon after birth to gradually moving the foot into the correct position. Severe cases of clubfoot require surgery. After the foot is in the correct position, the child typically wears a special brace for up to three years.[8]

Contracture
A contracture is a condition of shortening and hardening of muscles, tendons, or other tissue, often leading to deformity and rigidity of joints. Contractures are caused by immobility and can happen in as little as two days if the joint remains immobile. It can be the result of several disorders such as a stroke, cerebral palsy, or muscular dystrophy. Contractures may be prevented and/or treated with braces, physical therapy, and range-of-motion exercises.[9] See Figure 10.41[10] for an image of a hand contracture.

Dislocation and Subluxation
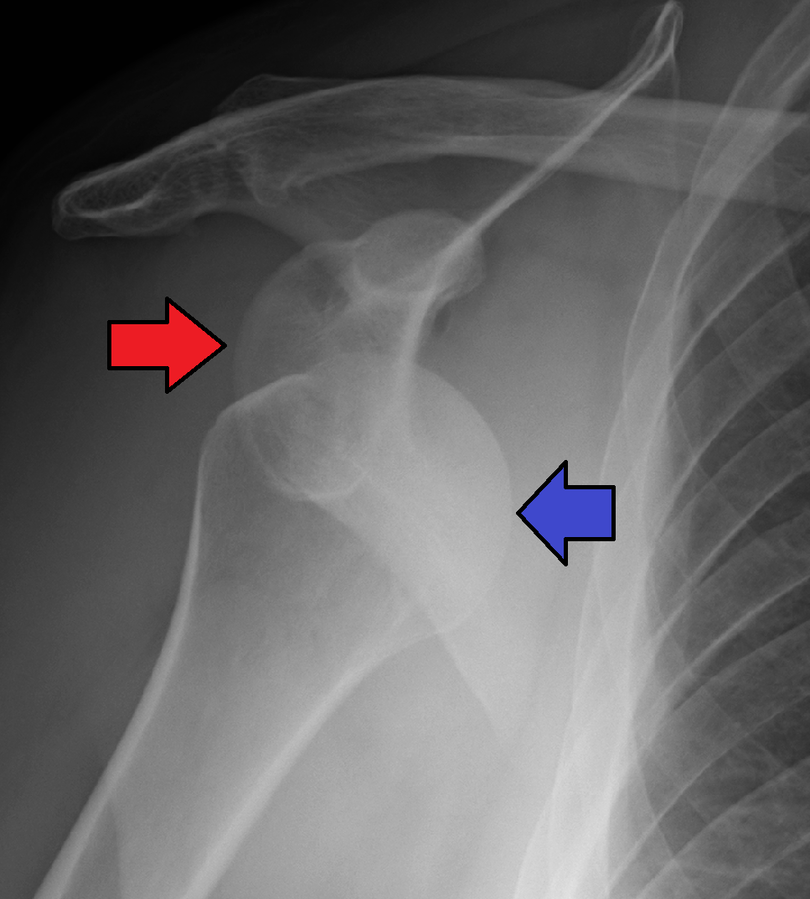
A dislocation is an injury, often caused by a fall or a blow to the joint, that forces the ends of bones out of position. Subluxation refers to partial dislocation of a joint, resulting in structural displacement. Dislocated joints are typically very painful, swollen, and visibly out of place. The client may not be able to move the affected extremity. See Figure 10.42[11] for an X-ray image of an anterior dislocation of the right shoulder where the ball (i.e., head of the humerus) has popped out of the socket (i.e., the glenoid cavity of the scapula). A dislocated joint requires immediate medical attention. Treatment depends on the joint and the severity of the injury and may include manipulation to reposition the bones, medication, a splint or sling, or rehabilitation. When properly repositioned, a joint will usually function and move normally again in a few weeks; however, once a joint is dislocated, it is more likely to become dislocated again. Instructing clients to wear protective gear during sports may help to prevent future dislocations.[12]
Fibromyalgia
Fibromyalgia is a condition that causes widespread pain, sleep problems, fatigue, and often emotional and mental distress. People with fibromyalgia may be more sensitive to pain than people without fibromyalgia, referred to as abnormal pain perception processing. The cause of fibromyalgia is not known, but it can be effectively treated and managed.(Centers for Disease Control and Prevention. (2022). Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm)
Common symptoms of fibromyalgia include the following:
- Pain and stiffness all over the body
- Fatigue and tiredness
- Depression and anxiety
- Sleep problems
- Problems with thinking, memory, and concentration
- Headaches, including migraines
- Tingling or numbness in hands and feet
- Pain in the face or jaw, including disorders of the jaw known as temporomandibular joint syndrome (TMJ)
- Digestive problems, such as abdominal pain, bloating, constipation, and irritable bowel syndrome (IBS)
Fibromyalgia is treated by a doctor or team of health care professionals who specialize in the treatment of fibromyalgia. A combination of treatments is typically prescribed, which may include the following[13]:
- Medications, including prescription drugs and over-the-counter pain relievers
- Aerobic exercise and muscle strengthening exercise
- Client education classes
- Stress management techniques such as meditation, yoga, and massage
- Good sleep habits to improve the quality of sleep
- Cognitive behavioral therapy, a type of talk therapy that helps people change the way they think about their life circumstances
Foot Drop
Foot drop is the inability to raise the front part of the foot due to weakness or paralysis of the muscles that lift the foot. As a result, individuals with foot drop often scuff their toes along the ground when walking or bend their knees to lift their foot higher than usual to avoid the scuffing. Foot drop is a symptom of an underlying problem and can be temporary or permanent, depending on the cause. The prognosis for foot drop depends on the cause. Foot drop caused by trauma or nerve damage usually shows partial or complete recovery, but in progressive neurological disorders, foot drop will be a symptom that is likely to continue as a lifelong disability. Treatment depends on the specific cause of foot drop. The most common treatment is to support the foot with lightweight leg braces. See Figure 10.43[14] for an image of a client with foot drop treated with a leg brace. Exercise therapy to strengthen the muscles and maintain joint motion also helps to improve a client’s gait.[15]

Gout
Gout is a type of inflammatory arthritis that causes pain and swelling in the joints, usually as flares that last for one or two weeks and then resolve. Gout flares often begin in the big toe or a lower limb. Gout occurs when high levels of serum uric acid form needle-shaped crystals in and around the joint and cause inflammation. Uric acid is a waste product produced by the breakdown of purine, a type of molecule found in many foods we eat. Gout is diagnosed with blood tests for uric acid. It is commonly treated with medications like nonsteroidal anti-inflammatories (NSAIDs) and colchicine.[16] It is common for gout to reoccur. Clients with recurring gout are treated with allopurinol to decrease chronic uric acid levels. See Figure 10.44[17] for an illustration of gout.

Read additional information about medications used to treat gout in “Antigout Medications” in the “Analgesics and Musculoskeletal System” chapter in Open RN Nursing Pharmacology, 2e.
Osteomyelitis
Osteomyelitis is an infection in a bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Infections can also begin in the bone itself if an injury exposes the bone to bacteria. Smokers and people with chronic health conditions, such as diabetes or kidney failure, are at higher risk of developing osteomyelitis. People who have diabetes may develop osteomyelitis in their feet if they develop foot ulcers. Although once considered incurable, osteomyelitis can now be successfully treated with surgery and intravenous antibiotics typically administered over a long period of time, such as four to six weeks.[18]
Muscular Dystrophy
Muscular dystrophy (MD) refers to a group of diseases caused by abnormal muscle development due to gene mutations. Muscular dystrophy can run in families, or a person can be the first in their family to have muscular dystrophy. Over time, muscle weakness decreases mobility and makes it difficult to perform everyday tasks. There are many types of muscular dystrophy, each affecting specific muscle groups. Each type has signs and symptoms that appear at different ages and vary in severity.[19]
An example of one type of MD is Duchenne muscular dystrophy (DMD), a genetic disorder characterized by progressive muscle degeneration and weakness due to the alterations of a muscle protein called dystrophin. DMD symptom onset is in early childhood, usually between the ages two and three. The disease primarily affects boys. Muscle weakness is the principal symptom of DMD and begins by first affecting the proximal muscles (those closest to the core of the body) and later affecting the distal limb muscles. The child with DMD might have difficulty jumping, running, and walking. Other symptoms include enlargement of the calves, a waddling gait, and lumbar lordosis (an inward curve of the spine). The heart and respiratory muscles are affected as well. Progressive weakness and scoliosis result in impaired pulmonary function, which can eventually cause acute respiratory failure. Treatment of DMD requires multidisciplinary care to coordinate specialized assessments and interventions needed to maximize function and quality of life. Due to recent advances in cardiology and pulmonology, people with DMD are living longer than ever and often well into adulthood.[20]
The impact of DMD can be significantly minimized by keeping the body as flexible, upright, and mobile as possible. As muscle deteriorates, a person with muscular dystrophy often develops contractures. If not treated, contractures can become severe, causing discomfort and restricting mobility and flexibility. Contractures can affect the knees, hips, feet, elbows, wrists, and fingers. However, there are many ways to minimize and postpone contractures. Range-of-motion exercises performed on a regular schedule help delay contractures by keeping tendons from shortening prematurely. Braces on the lower legs also can help keep the limbs stretched and flexible, delaying the onset of contractures. Eventually, a wheelchair is needed, typically by about age 12. Although a child and their parents may dread using a wheelchair, many people find that when they start to use one, they are more mobile, energetic, and independent than when trying to walk without assistance.[21] See Figure 10.45[22] for an image of a child with MD using a specialized wheelchair called an “Easy Stand” that supports him while sitting and also allows him to stand for periods of time.

Myasthenia Gravis
Myasthenia gravis (MG) is a chronic, autoimmune, neuromuscular disease that causes weakness in voluntary muscles, including those required for breathing and swallowing. Onset of symptoms can be rapid[23]
Paralysis
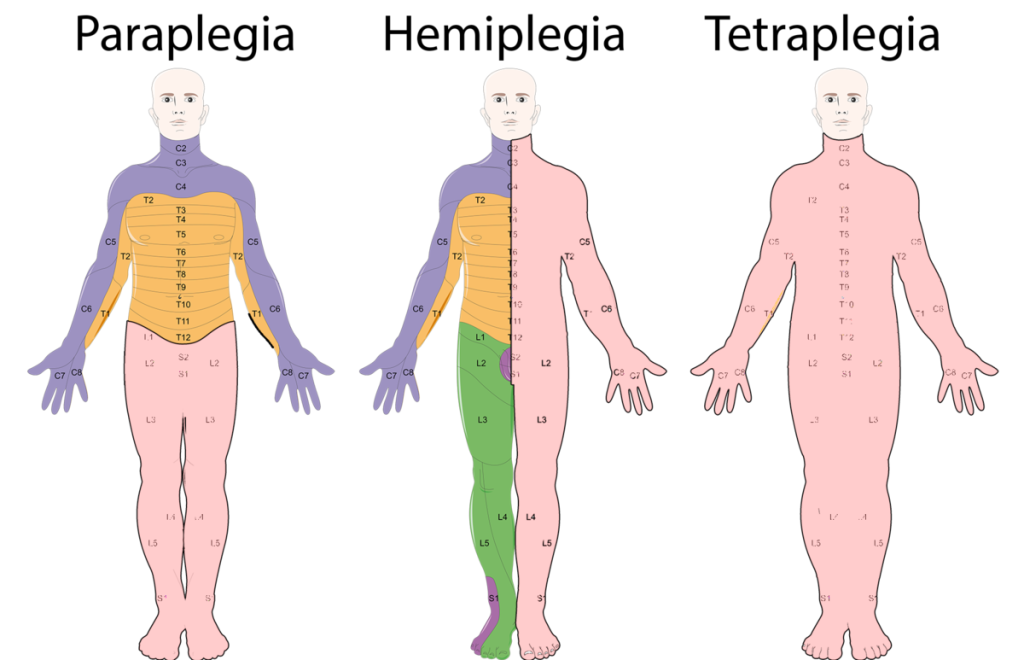
Paralysis occurs when an injury or medical condition disrupts the nerve signals to the muscles, resulting in being unable to make voluntary movements. Common causes of paralysis include spinal cord injuries and strokes. Paralysis can be localized, where it affects specific areas of the body, such as the face. For example, Bell’s palsy temporarily paralyzes facial muscles. Paralysis can also be generalized where it affects a larger area of the body. There are categories of generalized paralysis based on its extent. Common categories include hemiplegia, paraplegia, and quadriplegia/tetraplegia[24]:
- Hemiplegia: Paralysis affects one side of the body, for example, an arm and a leg on the same side.
- Paraplegia: Paralysis affects both legs and sometimes the torso.
- Quadriplegia or Tetraplegia: Cervical nerves are damaged, causing paralysis in all limbs, with little or no movement from the neck down.
See Figure 10.46[25] for an illustration of paraplegia, hemiplegia, and tetraplegia (quadriplegia), where pink indicates the area of muscle paralysis. Because muscle paralysis is caused by disruption of nerve signals, the cervical (C), thoracic (T), and lumbar (L) nerves are labeled in the image.
Paralysis is also classified by its effect on muscles in terms of being flaccid or spastic[26]:
- Flaccid: The muscles atrophy (i.e., shrink) due to loss of function.
- Spastic: The muscles tighten, causing uncontrollable jerks and spasms.
There is no cure for permanent paralysis caused by spinal nerve damage because the spinal cord can’t heal itself. However, rehabilitative services like physical and occupational therapy can help people with paralysis live independently and enjoy a quality life. Equipment used for rehabilitative/restorative care may include the following[27]:
- Adaptive equipment: Equipment that allows people to feed themselves or drive.
- Assistive equipment: Equipment that enhances mobility, such as wheelchairs, scooters, crutches, and canes.
- Orthotic/prosthetic devices: Devices that support the limbs and prevent contractures, such as braces.
- Voice-activated technology: Technology that doesn’t require the need for touch or movement, such as computers, lighting systems, and phones.
See Figure 10.47[28] for an image of Mark Manion, founder of “Mark Speaks Out.” Mark was permanently disabled during a cross-country biking trip when he was struck by a drunk driver. He travels the country educating and inspiring audiences on how he has effectively coped with his life circumstances.

Rhabdomyolysis
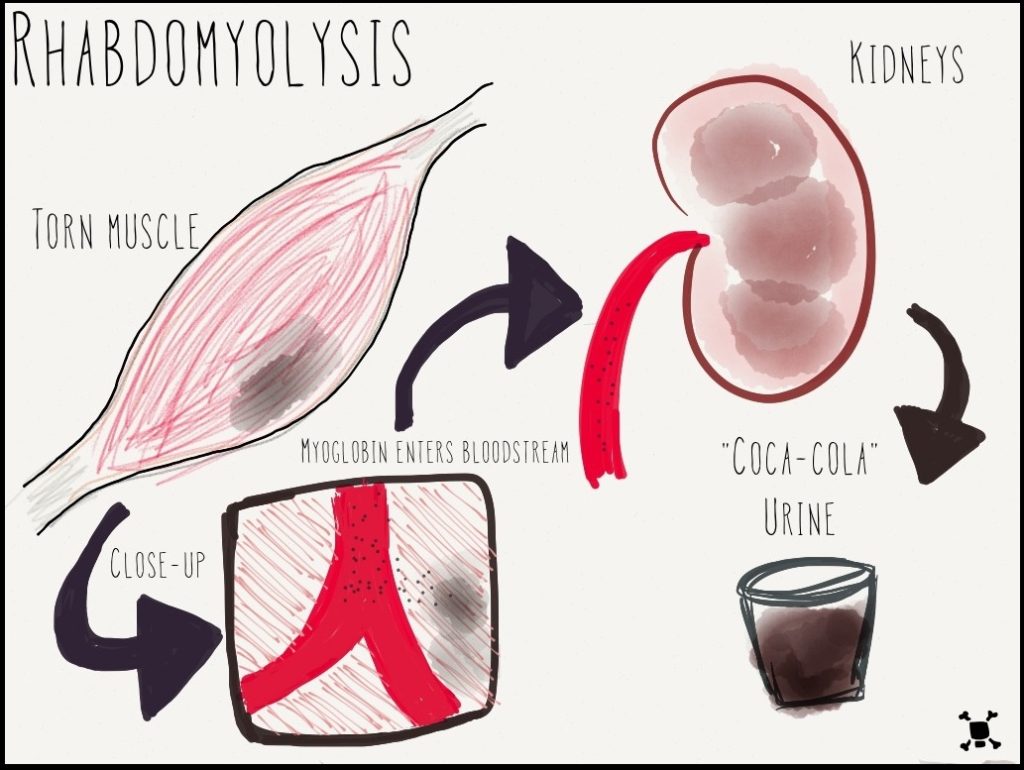
Rhabdomyolysis refers to the breakdown of muscles that causes damage to the kidney. When muscle is damaged, a protein called myoglobin is released into the bloodstream and is filtered out of the body by the kidneys. Myoglobin breaks down into substances that damage kidney cells.[29] See Figure 10.48[30] for an illustration of rhabdomyolysis.
Rhabdomyolysis may be caused by injury or any other condition that damages skeletal muscle. Potential causes of rhabdomyolysis include the following conditions[31]:
- Trauma or crush injuries
- Use of drugs such as cocaine, amphetamines, statins, heroin, or phencyclidine (PCP)
- Genetic muscle diseases
- Extremes of body temperature
- Ischemia or death of muscle tissue
- Low phosphate levels
- Seizures or muscle tremors
- Severe exertion, such as marathon running or calisthenics
- Lengthy surgical procedures
- Severe dehydration
Symptoms of rhabdomyolysis include dark, red, or cola-colored urine; decreased urine output; weakness; and myalgia (i.e., muscle pain). Rhabdomyolysis is diagnosed with blood tests, including creatine kinase (CK), myoglobin, and creatinine, as well as urine tests such as urinalysis and urine myoglobin. Rhabdomyolysis is treated with intravenous fluids that contain bicarbonate. In cases causing severe kidney damage, dialysis may be required.[32]
Strains and Sprains
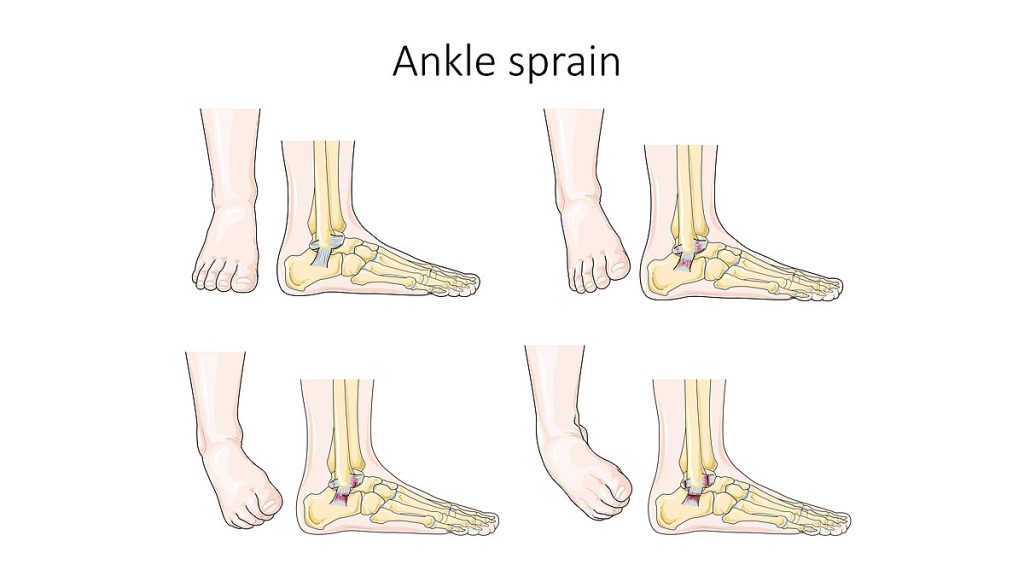
A strain is an injury to a muscle or tendon from being overstretched or torn, causing pain. Strains can be caused by an injury, overusing a muscle, or using a muscle in the wrong way (such as twisting the back while lifting a heavy object). A sprain is an injury to a joint when a ligament is stretched or torn. See Figure 10.49[33] for an illustration of an ankle sprain.
Initial treatments for strains and sprains are similar and can be easily recalled by the mnemonic called RICE, which stands for the following[34]:
- Rest: Rest the strain or sprain for at least 24 hours. The health care provider may recommend not putting any weight on the injured area for 48 to 72 hours, so crutches may be needed for lower extremity injuries.
- Ice: Apply ice as soon as possible after the injury to reduce swelling. The ice should not be applied directly to the skin but should be wrapped in a cloth to avoid tissue injury. Ice should be applied for 5 to 20 minutes, four to eight times a day, for the first 48 hours or until swelling improves.
- Compression: Compress the area with an elastic wrap or bandage to reduce swelling.
- Elevate: Elevate the injured limb above the heart whenever possible to help prevent or limit swelling.
Tendonitis
Tendonitis refers to inflammation of a tendon, causing pain around a joint. Tendonitis usually happens after repeated injury to an area such as the wrist or ankle. Common forms of tendonitis are named after the sports that increase their risk, such as tennis elbow, golfer’s elbow, pitcher’s shoulder, swimmer’s shoulder, and jumper’s knee. Health care providers diagnose tendonitis based on medical history, a physical exam, and possible imaging tests. Initial treatment is focused on reducing pain and swelling with RICE (rest, ice, compression, and elevation). Other treatments may include ultrasound, physical therapy, steroid injections, and surgery in severe cases.[35]
Vertebral Disorders
The spine is composed of many vertebrae stacked on top of one another, forming the vertebral column. There are several disorders that can occur in the vertebral column causing abnormal curvature of the spine such as kyphosis, lordosis, and scoliosis. See Figure 10.50[36] for an illustration of kyphosis, lordosis, and scoliosis.
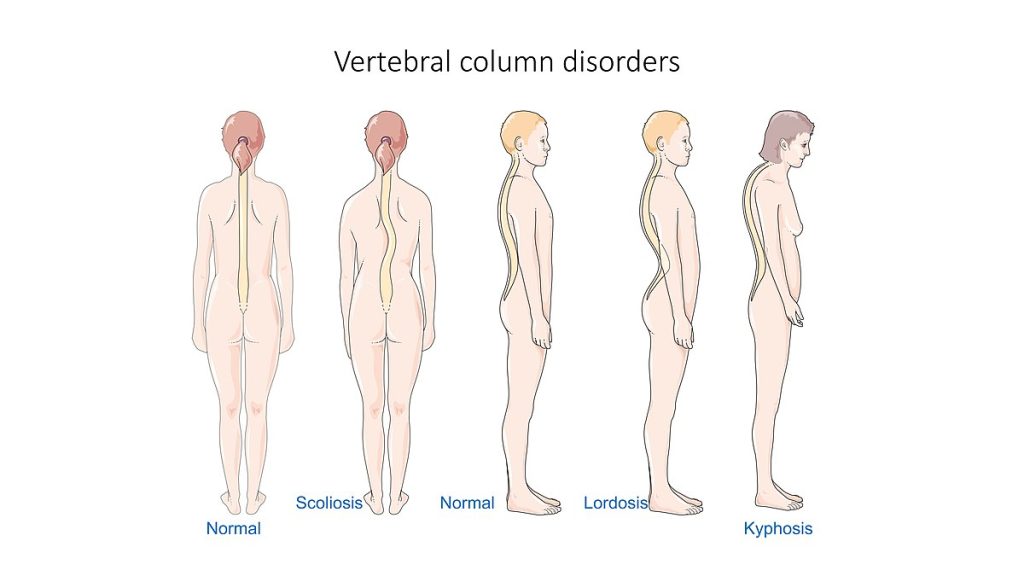
Kyphosis is a curving of the spine that causes a bowing or rounding of the back, often referred to as a “buffalo hump,” that can lead to a hunchback or slouching posture. Kyphosis can be caused by osteoarthritis, osteoporosis, or other conditions. Pain in the middle or lower back is the most common symptom. Treatment depends upon the cause, the severity of pain, and the presence of any neurological symptoms.[37]
Lordosis is the inward curve of the lumbar spine just above the buttocks. A small degree of lordosis is normal, especially during the third trimester of pregnancy. Too much curving of the lower back is often called swayback. Most of the time, lordosis is not treated if the back is flexible because it is not likely to progress or cause problems.[38]
Scoliosis causes a sideways curve of the spine. It commonly develops in late childhood and the early teens when children grow quickly. Symptoms of scoliosis include leaning to one side and having uneven shoulders and hips. Treatment depends on the client’s age, the amount of expected additional growth, the degree of curving, and whether the curve is temporary or permanent. Clients with mild scoliosis might only need checkups to monitor if the curve is getting worse, whereas others may require a brace or have surgery.[39]
- Mayo Clinic. (2023, May 11). Bone cancer. https://www.mayoclinic.org/diseases-conditions/bone-cancer/symptoms-causes/syc-20350217 ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- “David_Smith_and_his_Boccia_medals_(cropped).jpg” by Richard Gillin from St Albans, UK is licensed under CC BY-SA 2.0 ↵
- International Paralympic Committee. (n.d.). FAQ. https://www.paralympic.org/frequently-asked-questions ↵
- “813 Clubfoot.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Club foot; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/001228.htm ↵
- Friedlander, T., Masterson, R., & Mahesh, K. (2023, July 20). Contractures. PM&R KnowledgeNow. https://now.aapmr.org/contractures/#:~:text=Soft%20tissue%20changes%20that%20contribute,fibers%20occurs%20within%2024%20hours ↵
- “Freeman-Sheldon_syndrome.JPG” by MI Poling at English Wikipedia is licensed under CC BY-SA 2.5 ↵
- “AnterDisAPMark.png” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2019, Feb 7]. Dislocations; [reviewed 2016, Oct 26; cited 2020, Sep 18]. https://medlineplus.gov/dislocations.html ↵
- Centers for Disease Control and Prevention. (2022). Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm ↵
- “AFO brace for foot drop.JPG” by Pagemaker787 is licensed under CC BY-SA 4.0 ↵
- National Institute of Neurological Disorders and Stroke. (2019, March 27). Foot drop information page. https://www.ninds.nih.gov/Disorders/All-Disorders/Foot-Drop-Information-Page ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2020, February). Gout. National Institutes of Health. https://www.niams.nih.gov/health-topics/gout ↵
- “Gout_Signs_and_Symptoms.jpg” by www.scientificanimations.com is licensed under CC BY-SA 4.0 ↵
- Mayo Clinic. (2022, November 8). Osteomyelitis. https://www.mayoclinic.org/diseases-conditions/osteomyelitis/symptoms-causes/syc-20375913 ↵
- Centers for Disease Control and Prevention. (2022, November 21). What is muscular dystrophy? https://www.cdc.gov/ncbddd/musculardystrophy/facts.html ↵
- Muscular Dystrophy Association. (n.d.). Duchenne muscular dystrophy. https://www.mda.org/disease/duchenne-muscular-dystrophy ↵
- Muscular Dystrophy Association. (n.d.). Duchenne muscular dystrophy. https://www.mda.org/disease/duchenne-muscular-dystrophy ↵
- “3576255511_4c36222845_b.jpg” by EasyStand is licensed under CC BY-NC-ND 2.0 ↵
- National Institute of Neurological Disorders and Stroke. (2023, November). Myasthenia gravis. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- “Neurological_Levels_%26_Types_of_Paralysis.png” by Servier Medical Art is licensed under CC BY 2.0 ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- “USMC-100519-M-3215R-002.jpg” by unknown author for United States Marine Corps is licensed in the Public Domain ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- “Rhabdo.jpg” by AquapatMedia is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- “Ankle_sprain_--_Smart-Servier.jpg” by SMART-Servier Medical Art, part of Laboratoires Servier is licensed under CC BY-SA 3.0 ↵
- Mayo Clinic. (2022, March 22). Sprain: First aid. https://www.mayoclinic.org/first-aid/first-aid-sprain/basics/art-20056622 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2022, Apr. 4]. Tendinitis; [cited 2017, Mar. 16]. https://medlineplus.gov/tendinitis.html ↵
- “Vertebral column disorders - Normal Scoliosis Lordosis Kyphosis -- Smart-Servier.jpg” by Laboratoires Servier is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Kyphosis; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/001240.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Lordosis - lumbar; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/003278.htm ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Apr 29]. Scoliosis; [reviewed 2016, Oct 18; cited 2020, Sep 18]. https://medlineplus.gov/scoliosis.html ↵
A group of disorders that affects the ability to move and maintain balance and posture.
Stiff muscles.
Uncontrollable movements.
Poor balance and coordination.
A congenital condition that causes the foot and lower leg to turn inward and downward.
A condition of shortening and hardening of muscles, tendons, or other tissue, often leading to deformity and rigidity of joints.
Displacement of a bone from its normal position in a joint.
Refers to partial dislocation of a joint resulting in structural displacement.
A condition that causes widespread pain, sleep problems, fatigue, and often emotional and mental distress.
The inability to raise the front part of the foot due to weakness or paralysis of the muscles that lift the foot.
A type of inflammatory arthritis that causes pain and swelling in the joints, usually as flares that last for one or two weeks and then resolve.
An infection in a bone.
A group of diseases caused by abnormal muscle development due to gene mutations. Muscular dystrophy can run in families, or a person can be the first in their family to have muscular dystrophy.
A chronic, autoimmune, neuromuscular disease that causes weakness in voluntary muscles, including those required for breathing and swallowing.
Occurs when an injury or medical condition disrupts the nerve signals to the muscles, resulting in being unable to make voluntary movements.
The muscles atrophy (i.e., shrink) due to loss of function.
The muscles tighten, causing uncontrollable jerks and spasms.
Refers to the breakdown of muscles that causes damage to the kidney.
Muscle pain.
An injury to a muscle or tendon from being overstretched or torn, causing pain.
An injury to a joint when a ligament is stretched or torn.
Refers to inflammation of a tendon, causing pain around a joint.
A curving of the spine that causes a bowing or rounding of the back, often referred to as a "buffalo hump" that can lead to a hunchback or slouching posture.
The inward curve of the lumbar spine just above the buttocks.
A sideways curve of the spine.

