10.7 Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis and typically affects weight-bearing joints such as the knees, hips, spine, and hands.
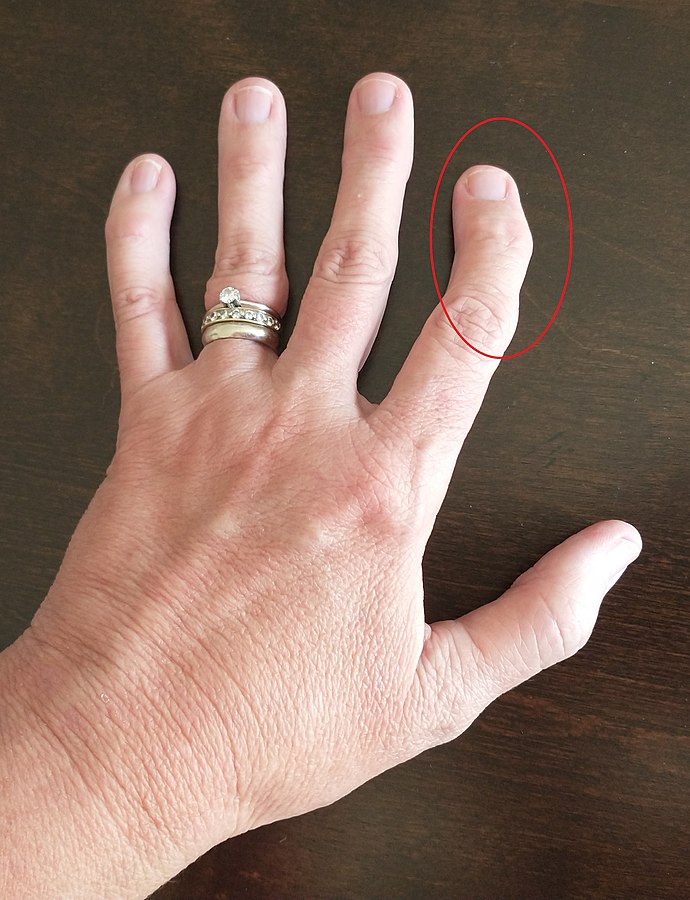
Risk factors for osteoarthritis include age, genetics, obesity, joint injuries, and occupations involving repetitive joint stress.[1] See Figure 10.34[2] for an image of a person with osteoarthritis in their finger.
Pathophysiology
Osteoarthritis is a degenerative joint disease characterized by the breakdown of joint cartilage and changes in the underlying bone. It occurs when cartilage wears away due to repetitive overuse of a joint and the inability of the cartilage to repair itself. As the cartilage breaks down, inflammatory processes within the joint occur as enzymes are released, causing the joints to swell and become stiff and painful. As the cartilage breaks down, osteophytes or bone spurs may occur, further restricting movement and causing additional pain. The joint spaces continue to narrow, resulting in reduced mobility and increased friction between the bones. Crepitus is a common symptom associated with osteoarthritis and is a popping, clicking, or crackling sound when moving a joint. It typically reflects air movement in the joint and is harmless.[3]
Assessment
While osteoarthritis primarily affects the musculoskeletal system, it can indirectly impact other body systems due to chronic pain, limited mobility, and the psychological toll it can take on an individual’s overall well-being. Assessment findings vary based on the severity and location of osteoarthritis. Common manifestations of osteoarthritis are summarized in Table 10.7a.
Table 10.7a. Manifestations of Osteoarthritis[4],[5],[6]
| Body System | Potential Assessment Findings |
|---|---|
| Musculoskeletal | Asymmetrical joint involvements with pain, especially after activity or prolonged rest; stiffness and reduced range of motion in affected joints; crepitus (grating or crackling sensation) with joint movement; and visible joint deformities or swelling |
| Integumentary | Warmth and redness over affected joints during periods of inflammation |
| Neurological | Numbness or tingling sensations due to nerve compression in affected joints |
| Psychological | Psychological impact such as anxiety, depression, or frustration due to chronic pain and limited mobility |
Diagnostic Testing
Diagnosis of osteoarthritis (OA) may include imaging studies and laboratory tests. X-rays may be ordered by the health care provider to visualize joint damage, joint narrowing, osteophyte formation, and potential changes in bone density. MRIs may also be ordered to examine soft tissue, cartilage breakdown, and the extent of joint damage. Laboratory tests, such as C-reactive protein and erythrocyte sedimentation rate, may also be ordered to rule out inflammatory arthritis.[7],[8]
Nursing Problems and Diagnoses
Nursing problems and diagnoses commonly associated with osteoarthritis focus on an individual’s functional ability, pain management, and adaptation to changes in lifestyle.
Common diagnoses for osteoarthritis include the following:
- Pain
- Impaired Mobility
- Self-care Deficit
- Risk for Falls
- Ineffective Coping
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Sample expected outcomes for a client with osteoarthritis are as follows:
- The client will report a chronic pain level acceptable to them within two weeks of implementing pain management strategies.
- The client will independently perform activities of daily living (e.g., walking, dressing, bathing) with minimal discomfort within two weeks.
- The client will demonstrate accurate use of assistive devices within one week.
- The client will verbalize three coping strategies related to self-management of osteoarthritis within one month.
Interventions
Medical Interventions
Medical interventions for osteoarthritis are diverse and aim to alleviate pain, improve joint function, and enhance the individual’s quality of life. Interventions may include medication therapy, physical therapy, weight management, and surgical interventions.[9],[10],[11]
Medication Therapy
Medication therapy for osteoarthritis may include several classes of medications:
- Pain Relievers: Acetaminophen is an analgesic that reduces pain. NSAIDs (i.e., ibuprofen or naproxen sodium) reduce pain, as well as inflammation. Celecoxib is a selective NSAID that helps reduce pain and inflammation but does not have the typical gastrointestinal side effects of other NSAIDs. It is typically avoided in individuals with hypertension, renal disease, or cardiovascular issues due to potential side effects. In cases of severe pain not adequately managed by other medications, opioids may be prescribed cautiously for short-term use to relieve pain. However, due to their potential for significant side effects and substance use disorder, they are usually considered only when other options have failed.
- Topical Medications: Creams, gels, or patches containing lidocaine, capsaicin, or diclofenac gel offer localized pain relief for joints with osteoarthritis.
- Disease-Modifying Drugs: In some cases, disease-modifying osteoarthritis drugs (DMOADs) like hyaluronic acid injections or glucosamine/chondroitin supplements are used to slow the progression of cartilage breakdown.
- Corticosteroid Injections: Injections of corticosteroids directly into the affected joint can provide short-term pain relief and reduce inflammation.
Physical Therapy/Assistive Devices
Tailored exercises and physical therapy programs help improve joint flexibility, strength, and range of motion. Therapists may also use modalities like heat, ice, or ultrasound for pain relief. In some cases, assistive devices like canes, braces, or splints can help reduce stress on affected joints and improve mobility.
Weight Management
Maintaining a healthy weight or losing excess weight reduces stress on weight-bearing joints, such as hips and knees, and can reduce the symptoms of osteoarthritis.
Surgical Interventions
In severe cases where conservative treatments fail, surgical options like arthroscopy (joint repair), arthroplasty (joint replacement) or joint fusion may be considered to relieve pain and improve joint function. Arthroscopy is a minimally invasive surgical procedure in which an endoscope is inserted by an orthopedic surgeon into the joint through a small incision. Small surgical instruments are inserted via additional incisions to remove or repair ligaments and other joint structures.
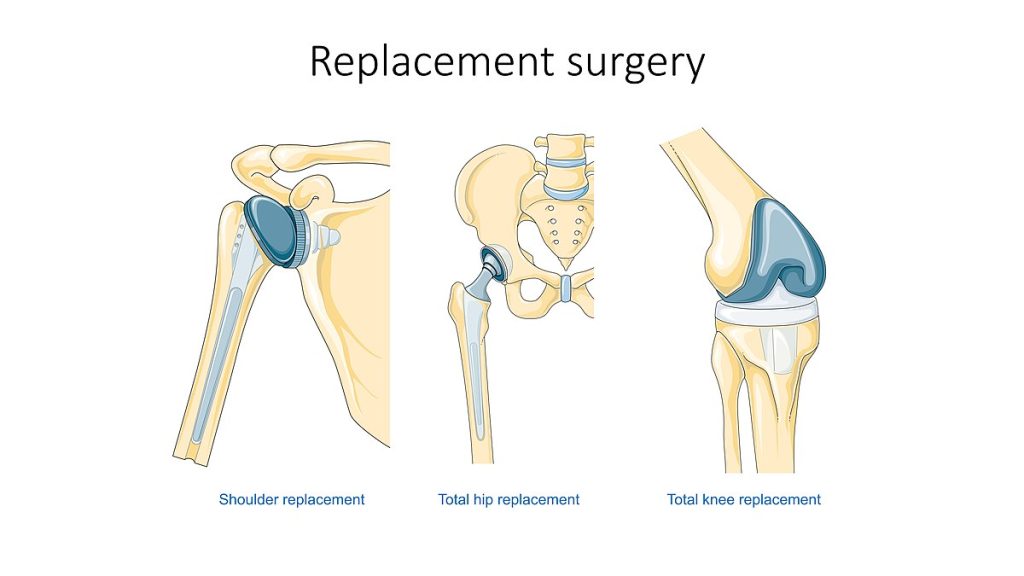
Arthroplasty refers to joint replacement surgery, an invasive procedure requiring extended recovery time. Hip and knee joints are commonly replaced, but other joints that can be replaced are shoulders, elbows, ankles, and wrists. This type of surgery involves replacing the articular surfaces of the bones with artificial components. For example, in hip arthroplasty, the worn or damaged parts of the hip joint, including the head and neck of the femur and the acetabulum of the pelvis, are removed and replaced with artificial joint components. The replacement head for the femur consists of a rounded ball attached to the end of a shaft that is inserted inside the femur. The acetabulum of the pelvis is reshaped, and a replacement socket is fitted into its place.[12] See Figure 10.35[13] for an illustration of joint replacement surgery.
Clients having arthroplasty may have outpatient surgery and go home the same day or stay in the hospital for one or two nights, depending upon their condition and recovery. See the following box for additional information on nursing considerations related to hip replacement surgery.
Hip Replacement Surgery (Arthroscopy)
Preoperative Care
Nurses provide preoperative education about the procedure and postoperative care for successful recovery and use of the new joint. Topics include assistive/ adaptive equipment, restricted movements to prevent dislocation of the joint, setting up of the home environment for after surgery, and medication planning such as pain management and anticoagulant therapy to prevent blood clots. Clients also complete preoperative testing, including blood tests (to rule out infection and determine baseline bleeding times) and an electrocardiogram (EKG) to evaluate their heart.
Hip Precautions
Hip precautions are implemented after surgery and taught to the client to avoid dislocation of the new hip joint[14]
- Avoid crossing the legs or feet.
- Sleep with a pillow between your legs.
- Do not flex the hip more than 90 degrees (i.e., do not lean too far forward from the waist or position the knee above the hip level when seated).
- Do not rotate the hip/leg inward toward your body.
Potential Complications
Nurses assess for potential complications and provide nursing care to prevent postoperative complications. See Table 10.7b for a summary of common complications, related focused assessments, and preventative measures.
Table 10.7b. Common Complications of Hip Replacement Surgery[15]
| Potential Complication | Focused Assessment | Preventative Measures |
|---|---|---|
| Deep Vein Thrombosis (DVT) and/or Pulmonary Embolism (PE) | The surgical limb is frequently assessed for signs of DVT, including unilateral calf pain, swelling, redness, and warmth.
Sudden symptoms of chest pain and/or shortness of breath should be immediately reported. |
|
| Excessive Bleeding | Monitor the surgical site dressing for excessive bleeding.
Monitor lab values (hemoglobin and hematocrit) for signs of anemia. |
|
| Surgical Site Infection | Monitor the client’s temperature, surgical limb, and white blood cell count for signs of infection. |
|
| Poor Pain Management | Frequently assess pain levels.
Monitor participation levels in physical therapy. |
|
| Constipation and Ileus
|
Perform abdominal assessment, including auscultation of bowel sounds. Monitor the date of the last bowel movement. |
|
| Hypotension and Fall Risk
|
Monitor balance and orthostatic blood pressure. |
|
| Dislocation | Assess for leg shortening with external or internal rotation if the client reports sudden onset of pain, a “snapping” feeling, or the sudden inability to walk or bear weight on the affected leg. |
|
| Skin Breakdown | Monitor pressure points for skin breakdown, including the heels. |
|
For more information about health teaching topics for clients after a hip replacement surgery, read the following article from Medline Plus: How to Take Care of Your New Hip Joint.
Nursing Interventions
Nursing interventions for clients with osteoarthritis focus on managing pain, promoting mobility and fulfillment of activities of daily living, and providing health teaching.
Pain Management
Nurses assess the client’s pain level and evaluate their response to prescribed medications. Clients are educated about the proper use of prescribed pain medications and their potential side effects. Clients are also taught about nonpharmacological pain management techniques like heat/cold therapy or guided imagery.
Read additional information about specific analgesics in the “Analgesic and Musculoskeletal Medications” section of Open RN Nursing Pharmacology, 2e.
Mobility Therapy
Nurses collaborate with physical therapists and reinforce personalized exercise programs focusing on joint mobility, flexibility, and strengthening. Clients are also taught proper body mechanics to reduce joint strain during daily activities. If assistive devices (i.e., canes, braces, or walkers) are prescribed, nurses reinforce their safe and effective use to improve mobility and reduce stress on affected joints.
Health Teaching
Nurses provide education about osteoarthritis, including its progression, treatment options, and self-care strategies. Guidance on lifestyle changes like weight management, healthy eating habits, and regular exercise is provided. Potential fall hazards in the home are discussed and recommendations for preventing falls, like removing throw rugs, are provided.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
- Arthritis Foundation. (n.d.). Osteoarthritis. https://www.arthritis.org/diseases/osteoarthritis ↵
- “Osteoarthritis_in_the_left_hand_index_finger.jpg” by Whoisjohngalt is licensed under CC BY-SA 4.0 ↵
- Drum, E. E., Kovats, A., Jones, M. D., Dennis, S., Naylor, J., Mills, K., & Thom, J. M. (2023). Creaky knees: Is there a reason for concern? A qualitative study of the perspectives of people with knee crepitus. Musculoskeletal Care, 21(4), 1114–1124. https://doi.org/10.1002/msc.1793 ↵
- Arthritis Foundation. (n.d.). Osteoarthritis. https://www.arthritis.org/diseases/osteoarthritis ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2023, September). Osteoarthritis. https://www.niams.nih.gov/health-topics/osteoarthritis ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2024, January 8]. Osteoarthritis; [cited 2023, December 15]. https://medlineplus.gov/osteoarthritis.html ↵
- Johns Hopkins Medicine. (n.d.). Diagnosing bone disorders. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/diagnosing-bone-disorders ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2024, January 8]. Osteoarthritis; [cited 2023, December 15]. https://medlineplus.gov/osteoarthritis.html ↵
- Arthritis Foundation. (n.d.). Osteoarthritis. https://www.arthritis.org/diseases/osteoarthritis ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2023, September). Osteoarthritis. https://www.niams.nih.gov/health-topics/osteoarthritis ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2024, January 8]. Osteoarthritis; [cited 2023, December 15]. https://medlineplus.gov/osteoarthritis.html ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Replacement surgery - Shoulder total hip and total knee replacement -- Smart-Servier.jpg” by Laboratoires Servier is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Taking care of your new hip joint; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/patientinstructions/000171.htm ↵
- Perkins, A. (2021). Total hip replacement explained. Nursing Made Incredibly Easy!, 19(1), 28-35. https://www.nursingcenter.com/cearticle?an=00152258-202101000-00007&Journal_ID=417221&Issue_ID=5727808 ↵
The most common form of arthritis and typically affects weight-bearing joints such as the knees, hips, spine, and hands.
A popping, clicking, or crackling sound when moving a joint.
A common procedure performed by orthopedic surgeons to view the inside of a joint to diagnose and/or to repair joint problems.
Refers to joint replacement surgery, an invasive procedure requiring extended recovery time.

