10.8 Osteoporosis
Osteopenia is an abnormal reduction of bone mass that can lead to osteoporosis. Osteoporosis is a progressive bone disease characterized by a decrease in bone density and deterioration of bone tissue, leading to bone fragility and increased risk of fractures in the hips, spine, and wrist.
Pathophysiology
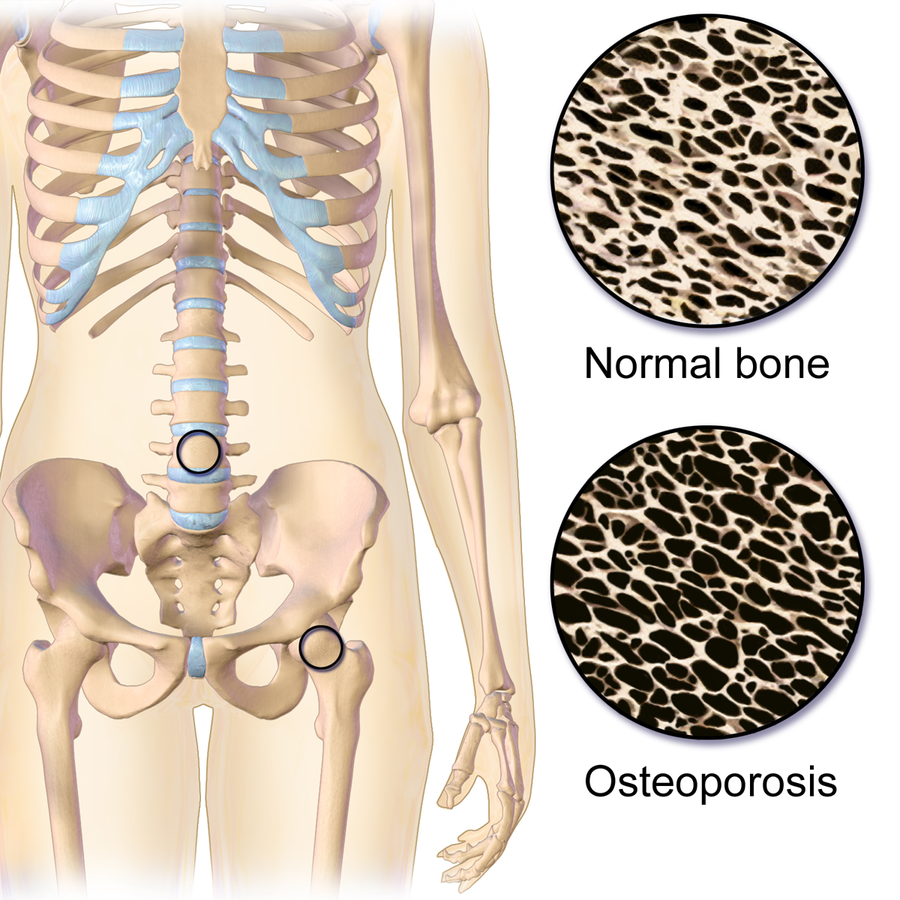
The pathophysiology of osteoporosis involves an imbalance between bone resorption and bone formation. Bone resorption outpaces bone formation, leading to a reduction in bone mass and structural deterioration. See Figure 10.36 for an illustration of osteoporosis.
Risk factors for osteoporosis include age, gender (women are at a higher risk, especially after menopause), genetics, hormonal changes, inadequate calcium and vitamin D intake, certain medications like corticosteroids, and lifestyle factors like smoking, excessive alcohol consumption, and lack of exercise.
Fractures related to osteoporosis can have severe consequences, affecting mobility, causing chronic pain, and leading to complications that impact overall quality of life.[1],[2]
Assessment
Osteoporosis is often considered a “silent disease” because it typically progresses without noticeable symptoms in its early stages. Individuals may remain unaware of their condition until a fracture occurs, often resulting from a simple fall or even during routine daily activities. Common manifestations of osteoporosis are summarized in Table 10.8.
Table 10.8. Manifestations of Osteoporosis[3],[4],[5]
| Body System | Potential Assessment Findings |
|---|---|
| Skeletal | Decreased bone mineral density (seen in DEXA scans); decreased height; vertebral compression fractures; hip, wrist, or other fractures from minor trauma or falls; and kyphosis |
| Respiratory | Reduced lung capacity or respiratory complications due to spinal deformities caused by vertebral compression fractures or abnormal curvature of the spine |
Diagnostic Testing
Diagnostic testing for osteoporosis primarily involves assessing bone density and evaluating fracture risk[6],[7],[8]:
- DEXA scans are the gold standard for diagnosing osteoporosis. The scan provides a T-score, comparing an individual’s bone density to that of a young, healthy adult and indicating the risk of fracture. A T-score between -1 and -2.5 indicates osteopenia, and a T-score of lower than -2.5 is diagnostic for osteoporosis.
- Quantitative ultrasound (QUS) measures bone density with sound waves at peripheral sites such as the heel. It can provide an estimate of fracture risk.
- A FRAX screening tool may be used to assess an individual’s overall fracture risk. The FRAX tool is a fracture risk calculator that estimates a client’s ten-year probability of a hip fracture or other major fracture. Completion of the FRAX tool allows providers to help make appropriate recommendations about lifestyle modification and risk mitigation.
Nursing Diagnoses
Nursing diagnoses for clients with osteoporosis can help guide nursing care and address the specific needs of these individuals. Common nursing diagnoses for osteoporosis include the following:
- Risk for Injury
- Impaired Nutrition: Less Than Body Requirements
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Sample expected outcomes for a client diagnosed with osteoporosis include the following:
- The client will verbalize three preferred sources of calcium-rich foods by the end of the teaching session.
- The client will verbalize three modifications to their home environment to prevent falls by the end of the teaching session.
Interventions
Medical Interventions
Medical interventions for osteoporosis aim to strengthen bones, reduce fracture risk, and improve overall bone health.
Medication Therapy
Common medications used to treat osteoporosis include the following:
- Bisphosphonates: Bisphosphonates (e.g., alendronate and risedronate) slow bone loss and reduce fracture risk by inhibiting bone breakdown.
- Denosumab: Denosumab is a monoclonal antibody injection given twice yearly, which helps to prevent osteoclast cells from developing.
- Hormone Therapy: In some cases, selective estrogen receptor modulators (SERMs) may be prescribed for postmenopausal women to help maintain bone density. An example of a SERM is raloxifene.
- Synthetic Forms of Parathyroid Hormone: Teriparatide and abaloparatide stimulate bone formation.
- Calcitonin: Calcitonin prevents bone loss and increases bone density.
- Calcium & Vitamin D Supplements: Calcium and vitamin D supplements may be prescribed to supplement dietary intake.
Lifestyle Modifications
Weight-bearing exercises and resistance training help maintain bone density and strength. Clients are encouraged to eat a balanced diet rich in calcium and vitamin D. Clients who smoke are advised to stop smoking, and excessive alcohol consumption should be avoided because it can weaken bones.
Surgical Intervention
In some cases of fractures caused by osteoporosis, surgical intervention may be required. Common fractures requiring surgical intervention include hip fractures and vertebral fractures. Vertebroplasty involves the injection of bone cement into fractured vertebrae to stabilize the fracture areas.[9],[10],[11],[12]
Nursing Interventions
Nursing interventions for osteoporosis focus on health teaching, preventing complications, and promoting overall client well-being.
Health Teaching
Nurses educate clients about modifiable risk factors for osteoporosis. Guidance is provided on preventive measures like adequate calcium and vitamin D intake, weight-bearing exercises, and fall prevention strategies. Calcium and vitamin D dietary sources include dairy products, leafy greens, and calcium-fortified foods like orange juice. Weight-bearing exercises like walking, jogging, dancing, as well as strength resistance training, can improve bone strength and density. Nurses consider the client’s abilities and preferences when discussing exercise programs and consider referrals to a physical therapist for additional recommendations for exercise programs and balance exercises. Routine bone density screenings are encouraged, especially for postmenopausal women, for the early detection of osteoporosis.
For clients who have been diagnosed with osteoporosis, nurses identify potential fall hazards in the home and provide recommendations for modifications to prevent falls that can cause fractures (e.g., removing rugs, improving lighting, and installing handrails). Techniques for using assistive devices like canes and walkers are reinforced to prevent falls.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Osteoporosis
RN Recap: Osteoporosis
View a brief YouTube video overview of osteoporosis[13]:
- National Institute on Aging. (2022). Osteoporosis. National Institutes of Health. https://www.nia.nih.gov/health/osteoporosis/osteoporosis ↵
- MedlinePlus [Internet]. (2017). Osteoporosis. https://medlineplus.gov/osteoporosis.html ↵
- National Institute on Aging. (2022). Osteoporosis. National Institutes of Health. https://www.nia.nih.gov/health/osteoporosis/osteoporosis ↵
- MedlinePlus [Internet]. (2017). Osteoporosis. https://medlineplus.gov/osteoporosis.html ↵
- American Academy of Orthopaedic Surgeons. (2021). Osteoporosis. https://orthoinfo.aaos.org/en/diseases--conditions/osteoporosis/ ↵
- InformedHealth.org. (2017). Understanding tests used to detect bone problems. Institute for Quality and Efficiency in Health Care (IQWiG). https://www.ncbi.nlm.nih.gov/books/NBK279413/ ↵
- Johns Hopkins Medicine. (n.d.). Diagnosing bone disorders. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/diagnosing-bone-disorders ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2023). Osteoarthritis. https://www.niams.nih.gov/health-topics/osteoarthritis ↵
- National Institute on Aging. (2022). Osteoporosis. National Institutes of Health. https://www.nia.nih.gov/health/osteoporosis/osteoporosis ↵
- MedlinePlus [Internet]. (2017). Osteoporosis. https://medlineplus.gov/osteoporosis.html ↵
- American Academy of Orthopaedic Surgeons. (2021). Osteoporosis. https://orthoinfo.aaos.org/en/diseases--conditions/osteoporosis/ ↵
- Arthritis Foundation. (n.d.). Osteoarthritis. https://www.arthritis.org/diseases/osteoarthritis ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 10 - Osteoporosis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/WFuPGu_58xY?si=St-9SiFSAra6tUa9 ↵
Abnormal reduction of bone mass.
A progressive bone disease characterized by a decrease in bone density and deterioration of bone tissue, leading to bone fragility and increased risk of fractures in the hips, spine, and wrist.
A test which is the gold standard for diagnosing osteoporosis.
Measures bone density at peripheral sites such as the heel with sound waves.
A fracture risk calculator that estimates a client’s ten-year probability of a hip fracture or other major fracture.
The injection of bone cement into fractured vertebrae to stabilize the fracture areas

