11.10 Peptic Ulcer Disease
Peptic ulcer disease (PUD) is characterized by erosions or ulcers in the gastrointestinal tract. PUD most commonly affects the duodenum and stomach, but it may also occur in the esophagus or jejunum.[1]
There are a variety of causes of PUD, but the most common causes are NSAID use and/or infection with Helicobacter pylori (H. pylori) bacteria. Other causes of PUD are stress due to severe illness or burns, the use of chemotherapy or radiation, or certain cancers. Other medications linked to PUD are steroid medications, potassium chloride, and bisphosphonates.[2]
Risk factors for developing PUD are low socioeconomic status, smoking, alcohol use, and obesity. Additionally, men have ulcers in the duodenum more frequently than women.[3]
Pathophysiology
Although there are a variety of causes of PUD, this section will focus on PUD caused by NSAID use and H. pylori bacterial infection. When PUD is caused by NSAID use, it is related to the blockage of COX enzymes. The COX-1 enzyme is responsible for prostaglandin production that protects gastrointestinal mucosa from acid. NSAIDs block the COX-1 enzyme and its protective effects on the gastrointestinal tract, leaving it vulnerable to ulcer formation.[4]
H. pylori is a gram-negative bacteria that leads to inflammation in the mucosa of the gastrointestinal tract that ultimately leads to erosions and ulcerations. H. pylori also disrupts the release of bicarbonate, causing increased acidity and also cellular changes in the GI tract that increase the risk for cancer.[5]
Assessment
Physical Exam
The signs and symptoms of PUD are determined by the location of the ulcer. Clients with a gastric ulcer generally experience epigastric pain soon after consuming a meal. Clients with an ulcer located in the duodenum typically have pain two to three hours after eating a meal. Duodenal ulcers can also cause pain that awakens the client at night. In addition to abdominal pain, clients with PUD may experience bloating, feelings of fullness in the abdomen, nausea, and vomiting.[6]
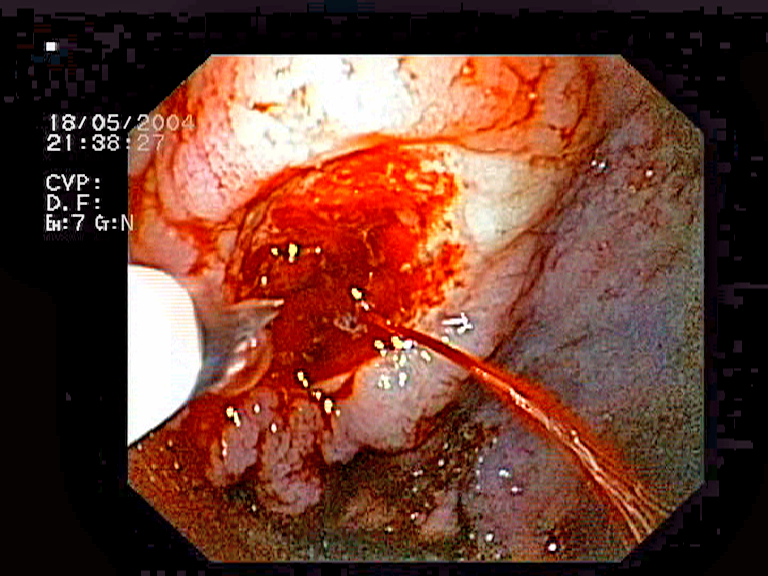
Complications of PUD, such as a perforated or bleeding ulcer, are suspected in clients with decreased red blood cell counts, blood in their stool or emesis, and unintended weight loss.[7] See Figure 11.32[8] for an image of a bleeding stomach ulcer.
Common Laboratory and Diagnostic Tests
Several laboratory and diagnostic tests may be ordered by the health care provider to diagnose PUD, but the gold standard is an esophagogastroduodenoscopy (EGD) because it allows visualization of ulcers. Biopsies can also be taken during an EGD to assess for the presence of H. pylori. If a client cannot undergo an EGD, a barium swallow is another diagnostic test used to diagnose PUD. In clients where a complication is suspected, such as perforation of the ulcer, a CT scan of the abdomen may be ordered. Client stool can also be tested for occult blood.[9],[10],[11]
In addition to diagnostic testing, blood work may also be performed[12],[13],[14]
- A complete blood count (CBC) may be ordered to assess for anemia related to bleeding ulcers.
- Blood testing can determine if there are antibodies to H. pylori present. Stool and urine tests are also available to check for the presence of H. pylori.
- Urea breath tests are very specific for the presence of H. pylori. In this test, the client ingests a urea-containing compound, and their breath sample is collected. If H. pylori is present, it will break down the urea, which can be detected in the sample.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing priorities for clients with PUD include managing pain, preventing complications, educating the client, and promoting nutrition.
Nursing diagnoses for clients with peptic ulcer disease are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Possible nursing diagnoses include the following[15]:
- Acute Pain
- Risk for Bleeding/Hemorrhage
- Readiness for Enhanced Knowledge
- Imbalanced Nutrition: Less than Body Requirements
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes for clients with PUD include the following:
- The client will rate their pain at 3 or less on a scale of 0 to 10 within four hours.
- The client will demonstrate stool/vomit that is free from blood until their next follow-up appointment.
- The client will describe common causes and treatment of peptic ulcer disease after the teaching session.
- The client will achieve a weight within a healthy range appropriate for their height within six months or less.
Interventions
Medical Interventions
Medical treatment for PUD can be categorized as lifestyle changes, medication therapy, and surgical management.[16]
Lifestyle Changes
Clients are taught lifestyle changes that can improve their outcomes, such as the following:
- Smoking cessation
- Avoiding digestive system irritants such as alcohol, caffeine, and heavily spiced foods
- Losing weight
Medications
Typical treatments for PUD are medications that decrease acid production and secretion. Commonly prescribed medications are proton pump inhibitors (PPIs) and H2 receptor antagonists (H2RAs). PPIs reduce the production of stomach acid, which not only provides symptomatic relief, but also promotes healing of ulcers. However, long-term use of PPIs has been associated with an increased occurrence of fractures, so calcium supplements may be recommended.[17] In addition to increase occurrence of fractures, research also indicates a higher risk of developing dementia with long-term use of PPIs.[18]
If PUD was caused by NSAIDs or other medications, these medications should be discontinued when possible or taken at a lower dosage. If clients have other medical conditions requiring NSAID treatment, prostaglandin analogs such as misoprostol may be prescribed to help prevent ulcer formation.[19]
If PUD was caused by the presence of H. pylori, treatment consists of prescriptions of a PPI with antibiotics to eradicate the bacteria.[20]
For more information on the medications used to treat PUD, visit the “Antiulcer Medications” section in the “Gastrointestinal System” chapter in Open RN Nursing Pharmacology, 2e.
Surgery
Surgery may be indicated for clients with PUD who do not respond to medications or have complications present. Common surgical procedures to treat PUD are vagotomy or a partial gastrectomy. A vagotomy severs part of the nerve supply to the stomach, which decreases acid production. A partial gastrectomy involves removing the ulcerated portion of the stomach.[21]
Nursing Interventions
When providing nursing care to a client with PUD, nursing interventions can be divided into nursing assessments, nursing actions, and client teaching[22],[23]:
Nursing Assessments
- Assess the client’s nutritional status because it can be impacted by the symptoms of PUD. Clients may exhibit weight gain if eating causes a reduction in ulcer pain or weight loss if eating causes increased pain.
- Perform a comprehensive pain assessment because pain caused by PUD can be similar to pain caused by a myocardial infarction. Sudden changes in pain can occur with ulcer perforation.
- Monitor vital signs, as changes could indicate a potential complication such as perforation of the ulcer or hemorrhage.
- Assess emesis/stool for the presence of blood.
- Assess lab values such as hemoglobin and hematocrit for decreases associated with a bleeding/hemorrhaging ulcer.
Nursing Actions
- Administer medications as prescribed by the provider.
- Encourage smoking cessation.
- During inpatient care, a nasogastric tube may be ordered.
Client Teaching
Teaching topics for clients with PUD typically include the following topics:
- Avoid taking aspirin and other NSAIDs or reduce their dosage, if possible.
- Avoid acidic, spicy, or oily foods, as these can exacerbate symptoms.
- Avoid caffeinated beverages and decaffeinated coffee, as these can increase the production of stomach acid.
View a supplementary video on PUD: Peptic Ulcer.[24]
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
![]() RN Recap: Peptic Ulcer Disease
RN Recap: Peptic Ulcer Disease
View a brief YouTube video overview of peptic ulcer disease[25]:
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Qureshi, O., & Dua, A. (2024). COX Inhibitors. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK549795/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- “Bleeding_gastric_ulcer.png” by Jeremias is licensed under CC BY-SA 3.0 ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Sankararaman, S., & Moosavi, L. (2024). Urea Breath Test. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK542286/ ↵
- Belleza, M. (2024). Peptic ulcer disease. https://nurseslabs.com/peptic-ulcer-disease/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Sankararaman, S., & Moosavi, L. (2024). Urea Breath Test. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK542286/ ↵
- Belleza, M. (2024). Peptic ulcer disease. https://nurseslabs.com/peptic-ulcer-disease/ ↵
- Belleza, M. (2024). Peptic ulcer disease. https://nurseslabs.com/peptic-ulcer-disease/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Northuis, C. A., Bell, E. J., Lutsey, P. L., George, K. M., Gottesman, R. F., Mosley, T. H., Whitsel, E. A., & Lakshminarayan, K. (2023). Cumulative use of proton pump inhibitors and risk of dementia: The Atherosclerosis Risk in Communities Study. Neurology, 101(18), e1771-e1778. https://doi.org/10.1212/WNL.0000000000207747 ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2023). Peptic Ulcer Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK534792/ ↵
- Belleza, M. (2023). Peptic ulcer disease. https://nurseslabs.com/peptic-ulcer-disease/ ↵
- Mercy Baltimore, MD. (n.d.). Peptic ulcer [Video]. Wistia. All rights reserved. https://mdmercy.com/mercy-services/conditions/peptic-ulcer-disease ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 11 - Peptic ulcer disease [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/dr3SpNbKiCM?si=qdFBSRmyshrHXWNy ↵
Characterized by erosions or ulcers in the gastrointestinal tract.

