9.10 Multiple Sclerosis
Multiple sclerosis (MS) is a chronic disease triggered by an immune-mediated response that leads to progressive demyelination in the CNS. MS is the most common disabling neurological disease among young adults between the ages of 20 to 50 years. MS tends to occur among whites of Northern European ancestry, but it can affect people of all ethnicities. MS affects women two to three times more than men. Although the exact reason for this gender difference is not known, hormonal influences are thought to play a part.
Pathophysiology
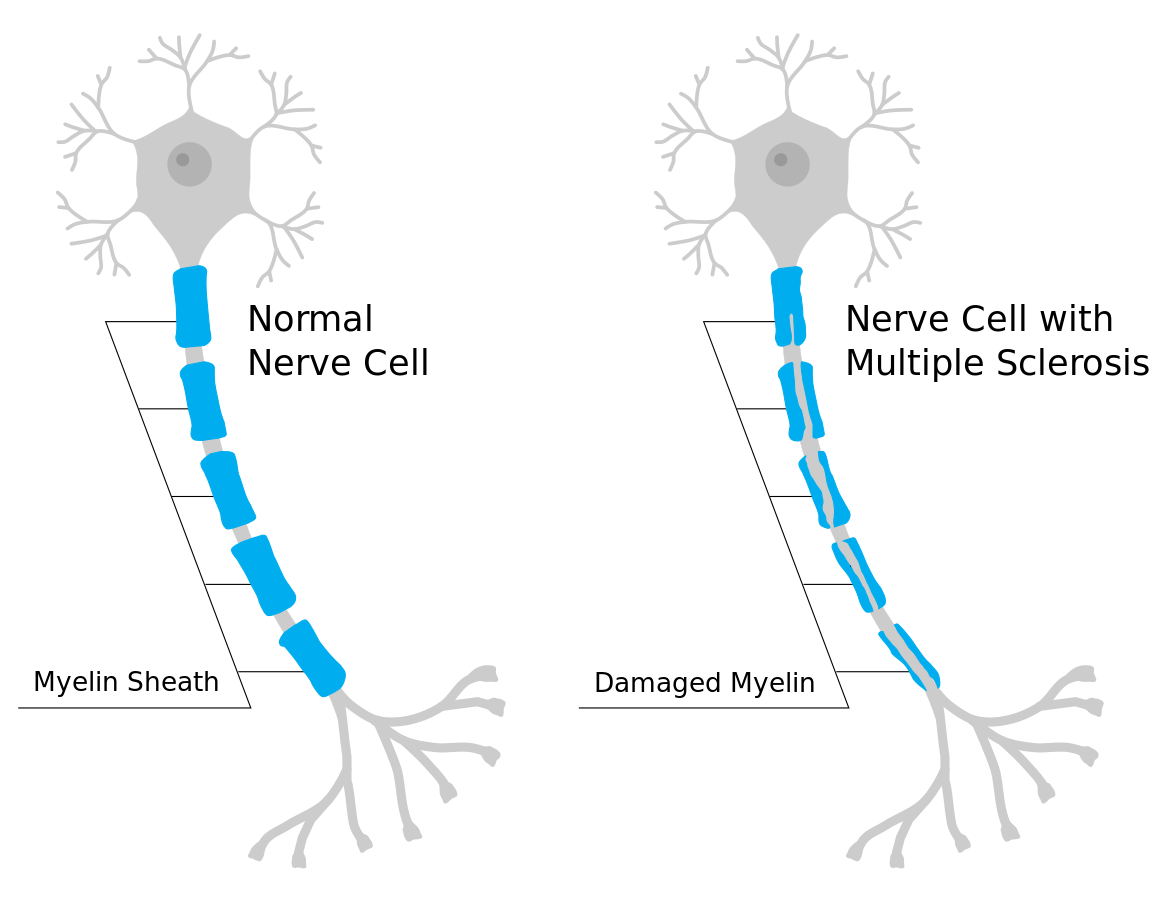
During MS, demyelination occurs. Demyelination refers to the loss or destruction of the myelin sheath. During demyelination, scar tissue forms and creates lesions. Myelin, commonly called the “white matter,” consists of fatty and protein substances that surround and protect nerve fibers of the brain and spinal cord. As this protective functional layer is lost, the transmission of nerve impulses between the brain, spinal cord, and the rest of the body becomes impaired. This impairment causes a delay or blockage of impulse transmission, resulting in impaired mobility and sensory functions. Initially, in the disease process, the body attempts remyelination, and the clinical symptoms may decrease to some degree. However, new lesions often develop, leading to neuronal injury and muscle atrophy. See Figure 9.27[1] for an illustration of damaged myelin that occurs in MS.
The cause of MS is complex and entails several immune, infectious, and genetic factors. However, MS is thought to primarily be an autoimmune disease where the body’s immune system mistakenly attacks the myelin in the brain and optic nerves, as well as the nerve cell bodies in the brain’s gray matter.[2] Ultimately, the outermost layer of the brain, the cerebral cortex, shrinks in size, known as cortical atrophy.[3]
Infectious factors such as measles, human herpesvirus-6, and Epstein-Barr virus (EBV) may also be involved in the development of MS. Research indicates that a previous infection with EBV (the virus that causes mononucleosis) contributes to the risk of developing MS.[4]
Genetic factors can also contribute to the development of MS. The risk of developing MS increases if first-degree relatives (parents, siblings, and offspring) have been diagnosed with MS.[5]
MS occurs more frequently in populations that live farther from the equator. Low vitamin D levels in the blood have been identified as a risk factor for the development of MS. Sun exposure (the natural source of vitamin D) may help to explain the northern distribution of MS.
Smoking increases a person’s risk for developing MS and is associated with rapid, severe disease progression. Smoking cessation before or after the onset of MS is associated with a slower progression of disability.
Types of MS
There are four major types of MS[6]:
- Relapsing-remitting: This is the most common type of MS. Exacerbations are “attacks” that cause new or worsening neurological symptoms. These attacks are also called relapses or exacerbations. They are followed by periods of partial or complete recovery (remission). In remissions, all symptoms may disappear, or some symptoms may continue and become permanent. However, during those periods of remission, the disease does not seem to progress.
- Primary progressive: This type causes a steady and gradual neurologic deterioration without remission of symptoms. Typically, clients do not manifest “acute attacks.”
- Secondary progressive: Some people develop a secondary progressive type after initially following the relapsing-remitting course. In the secondary progressive type, neurologic function and disability worsen progressively over time.
- Progressive-relapsing: This type is different from the relapsing-remitting type in that clients may have frequent relapses with partial recovery, but they do not return to baseline. Deterioration tends to occur over several years.
Assessment
Multiple sclerosis can act like many other neurologic diseases. There are a variety of potential manifestations of MS based on the location of the lesions and any periods of remission. It is important to collect a thorough history regarding the progression of symptoms and if they are constant or intermittent or if they are becoming increasingly worse. Ask about any aggravating factors that may trigger symptoms, such as fatigue, stress, or temperature extremes. In most instances, symptoms of MS are vague and nonspecific particularly in the early stages. Common initial symptoms are unilateral visual loss and associated visual changes such as blurred vision, diplopia, nystagmus (uncontrolled, repetitive movements of the eyes), and sometimes patchy blindness. Other symptoms of MS are summarized in the following box. See Figure 9.28[7] for an illustration of common symptoms of MS.
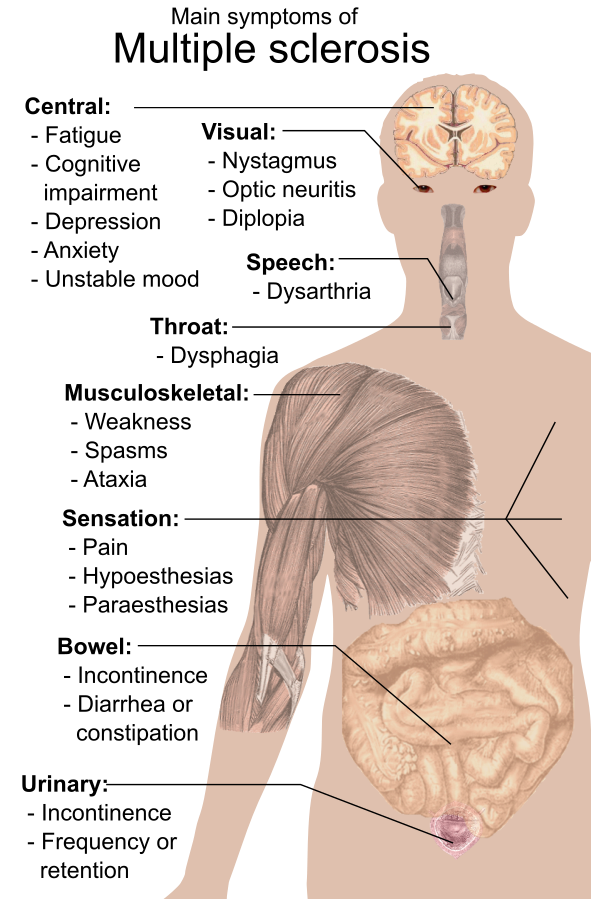
Signs and Symptoms of MS
- Visual and eye disturbances
- Fatigue, often worse in afternoon hours
- Muscle weakness
- Hypoesthesias (numbness)
- Paresthesias (tingling, numbness, itching, or burning)
- Pain (if lesions are on sensory pathways)
- Muscle spasticity in the extremities
- Ataxia (lack of coordination)
- Dysmetria (inability to direct or limit movement)
- Intention tremors (tremors while performing an activity, compared to resting tremors that occur during Parkinson’s disease)
- Dysarthria (difficulty speaking due to weak muscles)
- Tinnitus
- Vertigo
- Bowel and bladder dysfunction
- Partial or complete paralysis
- Alterations in sexual function, such as impotence
- Cognitive changes such as impaired judgment, memory loss, and decreased ability to problem solve
- Psychosocial or behavioral changes (depression, anxiety, irritability, euphoria, apathy, social isolation)
Common Laboratory and Diagnostic Tests
A combination of these tests is performed to diagnose MS in association with the client’s clinical presentation:
- Cerebrospinal fluid (CSF) analysis: Abnormally elevated proteins, increased white blood cells, increased myelin basic proteins, and increased immunoglobulins (especially IgG).
- MRI of the brain and spinal cord: Lesion formation in at least two areas is diagnostic for MS.
- Visual evoked potential test: Noninvasively invoking a visual response identifies impaired transmission along the optic nerve pathway.
View an animated image[8] of monthly MRIs that demonstrate exacerbation and remission of lesions:
Nursing Diagnoses
Priority nursing diagnoses for clients with MS may include the following[9]:
- Impaired Physical Mobility
- Fatigue
- Activity Intolerance
- Impaired Communication
- Ineffective Coping
- Anxiety
Outcome Identification
Overall goals for clients with MS include optimal levels of physical, cognitive, and emotional functioning:
- Minimize the frequency and severity of symptoms and relapses associated with MS, including fatigue, muscle weakness, and sensory disturbances
- Improve or maintain the client’s mobility and independence
- Promote emotional well-being
- Prevent complications such as falls, infections, and ulcers
- Enhance the overall quality of life for individuals with MS, encouraging them to participate in meaningful activities and relationships
Sample outcome criteria for clients with MS include the following:
- The client will identify four strategies for managing fatigue after the teaching session.
- The client will participate in two recommended mobility treatment programs within the next month.
- The client will report an improved sense of energy scoring at least 5 on 1-10 energy rating scale (10 being the highest level of energy, 1 being the lowest level).
Interventions
Clients with MS require multidisciplinary care due to the complexity of care and the variation of the disease and treatment.
Symptomatic management focuses on muscle spasticity, fatigue, bladder and bowel dysfunction, and ataxia. Physical and occupational therapy for clients with MS include range-of-motion exercises, ambulation within their abilities, positioning, and transferring. Other interventions include cognitive-behavioral therapy and vocational rehabilitation.
Medical Interventions
Medication Therapy
There is no cure for MS; therefore, the goals of medical treatment are to prevent and treat acute exacerbations, delay the progression of the disease, and manage chronic symptoms. There are a variety of medications used to treat and control the disease progression in clients with MS. The majority of the medications are immunomodulators or anti-inflammatory drugs. Both types of medication can affect the immune system and increase their risk for secondary infection. Muscle relaxants may be prescribed to reduce muscle spasticity, which can contribute to pain. Paresthesias may be treated with anticonvulsants or tricyclic antidepressants. Constipation from bowel dysfunction may be treated with stool softeners and laxatives as part of a bowel management program. Bladder dysfunction may be treated with antispasmodics (such as baclofen) or bladder relaxing medications (such as oxybutynin and tolterodine). See Table 9.10 for a summary of common medications used to manage MS.
Table 9.10. Common Medications for Management of Multiple Sclerosis
| Medication | Mechanism of Action and Considerations |
|---|---|
| Interferon-beta preparations (immunomodulator) | Reduces progression of disease and has antiviral effects. Can cause bone marrow suppression and increase risk of infection. |
| Glatiramer acetate | A synthetic protein similar to myelin used to decrease the number of plaques and increase time between relapses. |
| IV antineoplastic (mitoxantrone) | An anti-inflammatory agent used to resolve relapses and reduce neurologic disability. Risk of leukemia and cardiac toxicity. |
| IV monoclonal antibody(natalizumab) | Binds to WBCs to prevent further damage to the myelin. |
| Fingolimod, teriflunomide, and dimethyl fumarate | Protect brain and spinal cord cells by inhibiting immune cells and providing antioxidants. May cause bradycardia. |
| Baclofen or tizanidine | Muscle relaxant used to reduce muscle spasticity. |
| Anticonvulsant (carbamazepine) or tricyclic antidepressant (amitriptyline) | Reduce paresthesia. |
| Propranolol and clonazepam | Treat cerebellar ataxia. |
| Corticosteroids | Treat acute relapses. Shorten duration by exerting anti-inflammatory effects and acting on T cells and cytokines. |
Physical Therapy, Occupational Therapy, and Speech Therapy
Referral to physical therapy, occupational therapy, and speech therapy are part of the collaborative effort to provide therapies for optimal function. Occupational and physical therapists can develop exercise programs to assist the client with stretching and strengthening to manage spasticity and tremor. The occupational therapy can also assist the client with visual deficits with scanning techniques, modifications in environment, and use of an eye patch if diplopia is present. Speech therapists can help people who have difficulty speaking to communicate effectively and strengthen the muscles used in speech.
Surgical Interventions
In severe cases, neurosurgery or deep brain stimulation may be performed to provide relief from tremors.
Nursing Interventions
As with medical management, therapeutic interventions and nursing actions for clients with multiple sclerosis focus on promoting optimal mobility and function, prevention of exacerbations and complications, management of symptoms, and achieving optimal well-being. See the following box for an overview of nursing interventions.
Nursing Interventions for Clients with MS[10]
- Encourage independent activity independence to stay active as long as possible to maintain their strength.
- Implement energy conservation techniques to manage fatigue. Encourage clients to cluster their activities and provide frequent rest periods to conserve their energy for important tasks. Keep frequently used items in familiar places.
- Provide health teaching on bowel and bladder training. Include scheduled toileting to minimize and avoid incontinence.
- Ensure adequate fluid intake of 2,000-3,000 mL/day.
- Check the temperature of bath water and heating pads. Encourage clients to lower the maximum temperature on water heaters at home to prevent burns.
- Implement fall precautions in the home (remove rugs and clutter).
- Encourage daily exercises, including stretching and strengthening.
- Encourage independent activity to stay active for as long as possible and to maintain strength.
- Assess skin breakdown that may occur due to immobility and incontinence.
- Avoid vigorous activities that increase body temperature. Increased body temperature may lead to exacerbations (relapses), increased fatigue, diminished motor ability, and decreased visual acuity.
- Use eye patches for diplopia and alternate every few hours.
- Promote adequate rest and stress management techniques.
- Encourage participation in social activities to prevent social isolation.
- Refer to MS support groups to promote effective coping.
Health Promotion & Teaching
The effects of MS can be physically and mentally debilitating. Nurses provide support, education, and advocacy for clients and families affected by this disease. They each the client and their caregiver about the purpose of medications, side effects, and therapeutic response, and encourage calling the health care provider if questions or problems with medications occur.
Nurses also ensure the client understands techniques for self-care, daily life skills, and the use of any adaptive equipment. Information on bowel and bladder management, nutrition, and skin care is provided. MS affects the entire family mainly due to its unpredictability and uncertainty of the course, so nurses assist family members in identifying support systems and refer them to additional counseling as indicated.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with a family member or other member of the client’s interdisciplinary team.
- “Myelin_sheath_damage_in_multiple_sclerosis.svg" by Mjeltsch is licensed under CC BY-SA 4.0 ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Multiple sclerosis. https://www.ninds.nih.gov/health-information/disorders/multiple-sclerosis ↵
- National Multiple Sclerosis Society. (n.d.). What causes MS? https://www.nationalmssociety.org/What-is-MS/What-Causes-MS ↵
- National Multiple Sclerosis Society. (n.d.). What causes MS? https://www.nationalmssociety.org/What-is-MS/What-Causes-MS ↵
- National Multiple Sclerosis Society. (n.d.). What causes MS? https://www.nationalmssociety.org/What-is-MS/What-Causes-MS ↵
- National Multiple Sclerosis Society. (n.d.). What causes MS? https://www.nationalmssociety.org/What-is-MS/What-Causes-MS ↵
- “Symptoms_of_multiple_sclerosis.svg” by Mikael Häggström is in the Public Domain. ↵
- “Monthly_multiple_sclerosis_anim_bg.gif” by Gabby8228 (talk) is licensed under CC BY-SA 3.0 ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Vera, M. (2023, October 13). 7 multiple sclerosis nursing care plans. https://nurseslabs.com/multiple-sclerosis-nursing-care-plans/ ↵
A chronic disease triggered by an immune-mediated response that leads to progressive demyelination in the CNS.
The loss or destruction of the myelin sheath.
The most common type of MS characterized by exacerbations that cause new or worsening neurological symptoms following by periods of partial or complete recovery.
The type of MS which causes a steady and gradual neurologic deterioration without remission of symptoms.
A type of MS that develops following a relapsing-remitting course in which neurologic function and disability worsen progressively over time.
A type of MS in which clients may have frequent relapses with partial recovery, but they do not return to baseline.
Numbness.
Tingling, numbness, itching, or burning.
Poor balance and coordination.
Inability to direct or limit movement.
Unclear articulation of speech.
