8.8 Pyelonephritis
Pyelonephritis refers to a bacterial infection that typically starts as a urinary tract infection (UTI) that progresses up the ureters to the kidneys.
Pathophysiology and Risk Factors
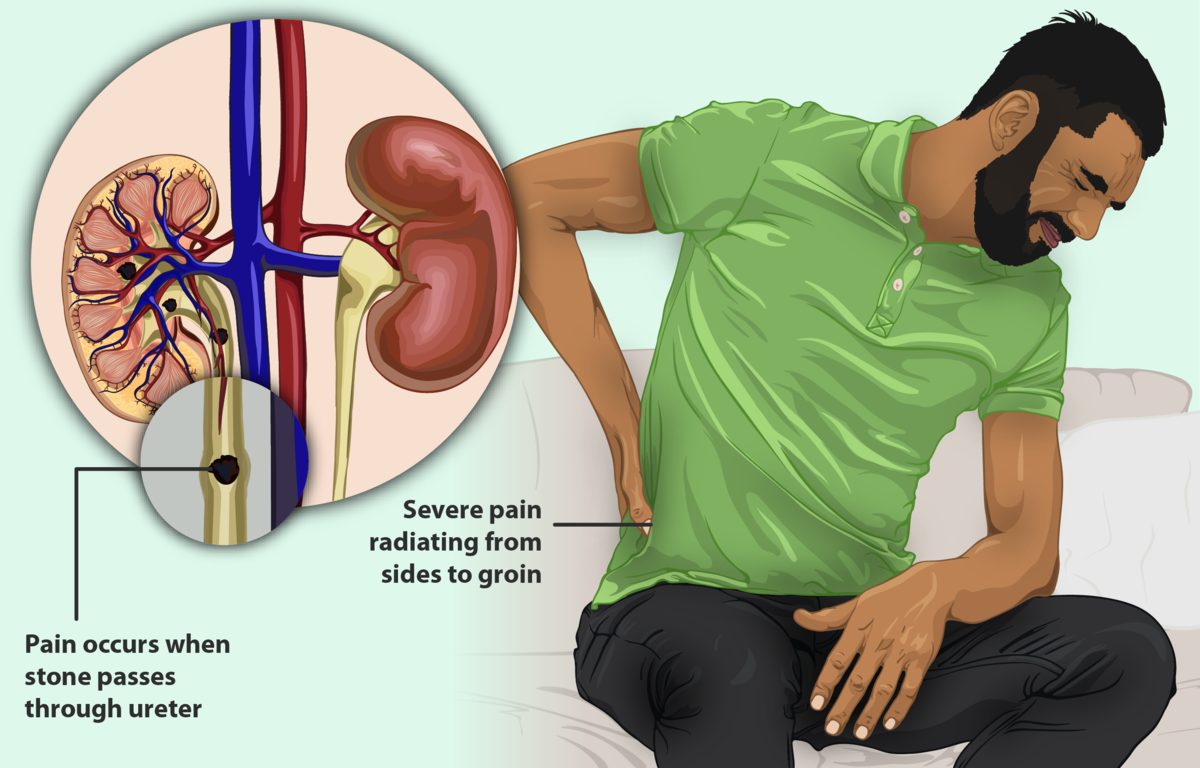
After the bacteria reach the kidneys, they multiply and cause inflammation, often causing classic symptoms of lower back/flank pain and systemic infection. See Figure 8.14[1] for an illustration of a client experiencing flank pain. The inflammatory response within the renal pelvis causes tissue damage and increased permeability of the blood vessels.
Risk factors for developing pyelonephritis include urinary tract obstructions like kidney stones, repeated urinary tract infections, diabetes, pregnancy, and conditions that weaken the immune system. If an infection is not properly treated, the bacteria will continue to multiply, resulting in a sustained infection, kidney abscess, sepsis, or chronic kidney damage.[2]
Assessment
Pyelonephritis is a bacterial kidney infection, resulting in inflammation of the functional parts of the kidney, including the renal cortex (the outermost part of the kidney) and the renal medulla. It is caused by the ascent of bacteria through the urinary tract, thus replicating signs and symptoms of urinary tract infections but leading to severe complications if left untreated. See Table 8.8 for clinical manifestations of pyelonephritis.
Table 8.8. Signs and Symptoms of Pyelonephritis[3],[4]
| Body System | Common Signs and Symptoms in Pyelonephritis |
|---|---|
| General | High-grade fever, chills, general malaise, and fatigue |
| Urinary | Flank/low back pain, dysuria, frequency, urgency, hematuria (blood in urine), and costovertebral angle tenderness (tenderness to palpation over the kidneys) |
| Gastrointestinal | Nausea and vomiting |
| Cardiovascular | Blood pressure fluctuations and tachycardia due to systemic infection |
| Neurological | Confusion (in severe cases with sepsis) |
| Respiratory | Elevated respiratory rate (in severe cases with sepsis) |
Diagnostic Testing
Diagnostic testing for pyelonephritis involves various methods to diagnose and assess the extent of the infection. To diagnose pyelonephritis, providers typically order a urinalysis and urine culture to initially assess for infection. Additional laboratory blood tests may be performed such as a complete blood cell count (to assess white blood cell count), creatinine and BUN levels to assess kidney function, and C-reactive protein (to assess for inflammation). Blood cultures may be performed to assess for systemic infection that can lead to sepsis.
Imaging studies may also be ordered to examine the size of the kidneys, any structural abnormalities, and the extent of the infection. Occasionally, nuclear medicine imaging may be ordered to help detect areas of reduced function or scarring.[5]
Nursing Problems & Diagnoses
Nursing problems and diagnoses for clients with pyelonephritis help guide nursing care and address the specific needs of these individuals.
Common diagnoses include the following:
- Acute Pain
- Impaired Urinary Elimination
- Imbalanced Nutrition: Less Than Body Requirements
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Examples of expected outcomes for clients with pyelonephritis are as follows:
- The client will report a decreased pain level of ≤3 on a 0-10 scale (0 being no pain, 10 being the worst pain imaginable) in the flank region within 24 hours.
- The client will report decreased dysuria within 72 hours.
- By the end of hospitalization or treatment, the client will remain free from signs and symptoms of infection, such as fever or increased white blood cell count.
Interventions
Medical Interventions
Medical interventions for pyelonephritis aim to treat the underlying infection, alleviate symptoms, and prevent complications. Clients with severe cases of pyelonephritis may require hospitalization for close monitoring and IV antibiotic/fluid therapy. Additional interventions may be implemented to drain renal abscess and treat sepsis if present.[6],[7]
Medication Therapy
Antibiotics, analgesics, and intravenous fluids may be prescribed to treat pyelonephritis[8],[9]:
- Antibiotic Therapy: Antibiotics target the specific bacteria causing the infection. Empirical treatment is often initiated based on the suspected pathogen and adjusted due to the effectiveness of the therapy. Commonly prescribed antibiotics include fluoroquinolones, cephalosporins, or trimethoprim-sulfamethoxazole.
- Analgesics: Analgesics such as NSAIDs (nonsteroidal anti-inflammatory drugs) or other pain medications may be prescribed to alleviate flank pain associated with pyelonephritis.
- Intravenous Fluids: IV fluids may be administered to maintain hydration and ensure adequate urine output. This helps to flush out bacteria from the urinary tract and support kidney function.
Surgical Intervention
In situations where an obstruction from a kidney stone is causing recurrent infections, surgery may be necessary to remove the stone if it is too large to pass on its own or removed by another means.
Nursing Interventions
Nursing interventions for pyelonephritis are centered on managing medication, addressing pain, and providing health teaching to prevent chronic kidney disease.
Medication Management
During inpatient care, nurses administer prescribed antibiotics and monitor urine culture results for potential antibiotic resistance. IV fluids may be administered, especially if there is poor oral intake.
Pain Management
Prescribed pain medications are administered as indicated to alleviate flank pain, such as NSAIDs, acetaminophen, or other analgesics. Nurses also encourage nonpharmacological pain interventions such as repositioning and heat application. Encourage using pillows for support or lying in a semi-Fowler’s position. A heating pad or warm compress may be applied to the affected flank area per the health care provider’s recommendations to help alleviate discomfort.
Health Teaching
Nurses provide health teaching on several topics related to pyelonephritis in terms of self-management and health promotion. Emphasize the importance of completing the full course of prescribed antibiotics to completely eradicate the infection and prevent recurrent infections that could lead to chronic kidney disease. Encourage hydration by drinking plenty of water to maintain adequate urinary flow and flush out bacteria. Explain the importance of regular and complete emptying of the bladder to prevent UTIs. Provide guidance on lifestyle changes such as maintaining a balanced diet, avoiding excessive salt intake, and avoiding habits detrimental to kidney health, such as smoking and excessive alcohol consumption.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
- "A_man_with_Kidney_Stones.png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Cleveland Clinic. (2023, January 31). Kidney infection (pyelonephritis). https://my.clevelandclinic.org/health/diseases/15456-kidney-infection-pyelonephritis ↵
- Cleveland Clinic. (2023, January 31). Kidney infection (pyelonephritis). https://my.clevelandclinic.org/health/diseases/15456-kidney-infection-pyelonephritis ↵
- Mayo Clinic. (2022, August 6). Kidney infection. https://www.mayoclinic.org/diseases-conditions/kidney-infection/symptoms-causes/syc-20353387 ↵
- Cleveland Clinic. (2023, January 31). Kidney infection (pyelonephritis). https://my.clevelandclinic.org/health/diseases/15456-kidney-infection-pyelonephritis ↵
- Cleveland Clinic. (2023, January 31). Kidney infection (pyelonephritis). https://my.clevelandclinic.org/health/diseases/15456-kidney-infection-pyelonephritis ↵
- Mayo Clinic. (2022, August 6). Kidney infection. https://www.mayoclinic.org/diseases-conditions/kidney-infection/symptoms-causes/syc-20353387 ↵
- Cleveland Clinic. (2023, January 31). Kidney infection (pyelonephritis). https://my.clevelandclinic.org/health/diseases/15456-kidney-infection-pyelonephritis ↵
- Mayo Clinic. (2022, August 6). Kidney infection. https://www.mayoclinic.org/diseases-conditions/kidney-infection/symptoms-causes/syc-20353387 ↵
Infection of the kidneys.
Tenderness to palpation over the kidneys.

