9.8 Meningitis
Meningitis is an infectious inflammatory process that involves the meninges, the protective membranes covering the brain and spinal cord. See Figure 9.21[1] for an illustration of the meninges.
![“Meninges-en.svg.png” by VG by Mysid, original by SEER Development Team [1], Jmarchn is licensed under CC BY-SA 3.0 Illustration showing layers of tissue from skin to brain, with text labels for major structures including Meninges](https://wtcs.pressbooks.pub/app/uploads/sites/47/2024/03/Meninges-en.svg.png)
Pathophysiology
Inflammation is commonly caused by a bacterial or viral infection. Streptococcus pneumoniae and Neisseria meningitidis (meningococcus) are the most common infecting organisms, followed by Haemophilus influenzae and Group B streptococcus. In some cases, inflammation may be caused by a fungus or parasite. Because the infection is so close to the brain and spinal cord, it can be life-threatening because of nerve damage, swelling within the brain, and increased intracranial pressure (ICP).
Bacterial meningococcal meningitis is a medical emergency due to a high mortality rate that can occur within 24 hours. Approximately 1 in 6 people who have meningococcal meningitis die. It is a highly contagious disease that can occur in densely populated communities, such as college campuses and military barracks.[2] For this reason, the meningococcal vaccination is strongly recommended for populations at risk.
Viral meningitis is commonly caused by herpes simplex virus-2, varicella zoster, paramyxovirus, and human immunodeficiency virus (HIV). The severity of the symptoms is correlated to the type of virus. Although the virus alters brain cell function, neurological defects are usually temporary, and full recovery is gained after the inflammation resolves.[3]
Meningeal infections generally occur in two ways, through the bloodstream or by direct transmission. The infection can spread in the bloodstream from infections of other organs, such as the heart and lungs. It can also occur from direct transmission, such as traumatic injury to the facial bones, sinusitis, otitis, brain abscess, or from invasive procedures (such as lumbar puncture).[4]
Risk Factors
Risk factors for bacterial meningitis include respiratory infection, otitis media, tooth abscesses, and mastoiditis because the bacteria can cross the epithelial membrane of the brain and enter the subarachnoid space. Individuals who are immunosuppressed are also at increased risk, such as those on immunosuppressants, chemotherapy, chronic steroid therapy, or have HIV. Newborn babies are at risk from maternal infection with Group B streptococcus.[5]
Signs and Symptoms
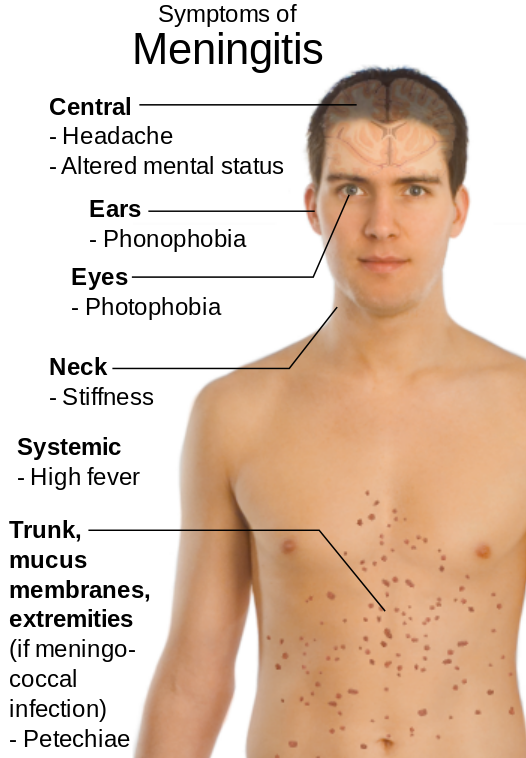
Signs and symptoms of meningitis are based on its cause. Classic symptoms of bacterial meningitis include a severe headache, rigidity of the neck, high fever, acute onset confusion, phonophobia, photophobia, nausea/vomiting, and petechiae on the trunk and extremities. Later stages include hemiparesis and hemiplegia.[6] See Figure 9.22[7] for an illustration of the signs and symptoms of meningitis.
Assessment
Clients presenting with signs and symptoms of meningitis may be assessed for Kernig and Brudzinski signs. The Brudzinski sign is when neck flexion causes the individual to automatically flex their hips and knees. The Kernig sign refers to pain that is elicited on passive extension of the client’s knees. However, these findings occur in a small percentage of clients. It is also important to consider that a high fever may not occur in older adults or those who are immunosuppressed or taking antibiotics.
View supplementary YouTube videos[8],[9] for symptoms of meningitis: Brudzinski’s Sign and Kernig’s Sign.
Other conditions can also occur due to meningitis. If inflammation spreads to the cerebral cortex, seizure activity may occur. Inflammation can also stimulate the hypothalamus to release antidiuretic hormone (ADH), resulting in hyponatremia due to increased water retention, further increasing the risk of elevated intracranial pressure (ICP).
Clients with meningitis are typically admitted to intensive care units for ICP monitoring. If left untreated, increased ICP can cause herniation of the brain, resulting in death.
Common Laboratory and Diagnostic Tests
Analysis of cerebrospinal fluid (CSF) is the classic diagnostic test for meningitis. CSF testing commonly includes opening fluid pressure, white blood cell count, protein, and glucose.
Gram stains and cultures may be obtained from the throat, nose, and urine if associated infections are suspected. Blood cultures are often collected.
Blood tests include white blood cell count, liver enzymes, serum electrolytes, and HIV testing. X-rays may be performed of the chest, sinuses, and mastoids if associated infections are suspected. Clients older than 60 years, those with increased ICP, or those who are immunosuppressed may have a CT scan before a lumbar puncture is performed because of the risk of brain herniation.[10],[11]
Nursing Diagnoses
Nursing diagnoses focus on neurologic dysfunction and tissue perfusion caused by the infectious, inflammatory process and may include the following[12]:
- Ineffective Cerebral Tissue Perfusion related to cerebral edema
- Ineffective Airway Clearance related to neuromuscular damage
- Hyperthermia related to infection
- Acute Pain related to increased intracranial pressure
- Interrupted Family Processes related to the critical nature of the situation and uncertain prognosis
Outcome Identification
Clients who have early recognition and treatment of meningitis tend to have good prognosis. Those who present with an altered state of consciousness have high morbidity and mortality. Nurses are key in facilitating prompt medical evaluation and initiation of prescribed treatment. Therefore, outcome identification for clients with meningitis include attaining adequate cerebral tissue performance either through prevention or reduction in increased ICP, maintaining normal body temperature, protecting against injury, enhancing coping measures, restoring normal cognitive functions, and preventing complications.
Sample outcome criteria for clients with meningitis include the following:
- The client will maintain or restore motor, cognitive, and sensory function within 24 hours.
- The client will achieve a normal body temperature within 48 hours.
- The client will express relief from pain within two hours.
Interventions
Medical Interventions
One of the most important interventions aimed at avoiding life-threatening complications from bacterial meningitis is prompt administration of broad-spectrum antibiotics until results from culture and Gram’s stain testing are available. After results are reported, an appropriate anti-infective drug is prescribed to treat the specific type of meningitis. The treatment of bacterial meningitis typically requires two to three weeks of IV antibiotics.
Intravenous corticosteroids such as dexamethasone are also administered to clients with community-acquired bacterial meningitis to prevent hearing loss and other neurological complications. Other medications may be prescribed for associated conditions, such as mannitol to treat increased ICP and anticonvulsant medications to treat seizures.
Additionally, individuals who have been in close contact with a person infected with N. meningitidis should receive prophylactic antibiotic treatment such as rifampicin, ciprofloxacin, or ceftriaxone.[13]
Nursing Interventions
Priority nursing interventions when caring for clients with meningitis are administering medication therapy and monitoring and documenting the client’s neurologic status. Other nursing interventions include monitoring vitals, decreasing environmental stimuli, and raising the head of the bed to 30 degrees or more to decrease ICP. Increased ICP can cause increased blood pressure and decreased heart rate. Blood pressure may also change if syndrome of inappropriate antidiuretic hormone (SIADH) secretion develops. Additionally, clients with bacterial meningitis should be placed on droplet transmission precautions.
Health Teaching
Nurses teach clients that vaccines are the most effective way to protect against certain types of bacterial meningitis. Vaccines for three types of bacteria that can cause meningitis include the following[14]:
- Meningococcal vaccines help protect against N. meningitidis
- Pneumococcal vaccines help protect against S. pneumoniae
- Haemophilus influenzae serotype b (Hib) vaccines help protect against Hib
Adults and parents of children are encouraged to remain current on their recommended vaccination schedules to prevent meningitis.
Read more about Immunization Schedules on the CDC website.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with a family member or other member of the client’s interdisciplinary team.
![]() RN Recap: Meningitis
RN Recap: Meningitis
View a brief YouTube video overview of meningitis[15]:
- “Meninges-en.svg.png” by VG by Mysid, original by SEER Development Team [1], Jmarchn is licensed under CC BY-SA 3.0 ↵
- World Health Organization. (2023). Meningitis. https://www.who.int/news-room/fact-sheets/detail/meningitis ↵
- World Health Organization. (2023). Meningitis. https://www.who.int/news-room/fact-sheets/detail/meningitis ↵
- World Health Organization. (2023). Meningitis. https://www.who.int/news-room/fact-sheets/detail/meningitis ↵
- World Health Organization. (2023, April 17). Meningitis. https://www.who.int/news-room/fact-sheets/detail/meningitis ↵
- World Health Organization. (2023). Meningitis. https://www.who.int/news-room/fact-sheets/detail/meningitis ↵
- “Symptoms_of_Meningitis.svg.png” by Mikael Häggström is in the Public Domain ↵
- Patient Examination Videos - Educor. (2022, April 14). Brudzinksi's sign [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=-ueX6ZL6TPc ↵
- Patient Examination Videos - Educor. (2022, April 14). Kernig's sign [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=XKu8FxO8i6I ↵
- Hersi, K., Gonzalez, F. J., Kondamudi, N. P., et al. (2023). Meningitis (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568762/ ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Hersi, K., Gonzalez, F. J., Kondamudi, N. P., et al. (2023). Meningitis (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568762/ ↵
- Center for Disease Control (n.d.) Meningococcal: Public health response for outbreaks. https://www.cdc.gov/meningococcal/php/public-health-strategy/index.html ↵
- Center for Disease Control (n.d.) Meningococcal: Public health response for outbreaks. https://www.cdc.gov/meningococcal/php/public-health-strategy/index.html ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 9 - Meningitis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/nkI4vCUi0xI?si=4UV75koNifoVDq_B ↵
An infectious inflammatory process that involves the meninges, the protective membranes covering the brain and spinal cord.
When neck flexion causes the individual to automatically flex their hips and knees.
Refers to pain that is elicited on passive extension of the client’s knees.

