9.11 Myasthenia Gravis
Myasthenia gravis (MG) is a chronic, autoimmune neuromuscular disease that causes weakness in voluntary muscles, including those required for breathing and swallowing. Onset of symptoms can be rapid.[1]
Pathophysiology
A key concept to understand related to MG is cholinesterase. Cholinesterase is a family of enzymes that break down the neurotransmitter acetylcholine (ACh) into choline and acetic acid. This reaction is necessary to allow a cholinergic neuron to return to its resting state after activation.[2]
MG affects the neuromuscular junction. Within a normal working nervous system, a chemical impulse causes the neurotransmitter acetylcholine (Ach) to be released into the neuromuscular junction. Acetylcholine attaches to the receptor sites of a muscle and stimulates a muscle contraction. Acetylcholine continually binds to the receptor sites to sustain muscle contraction.
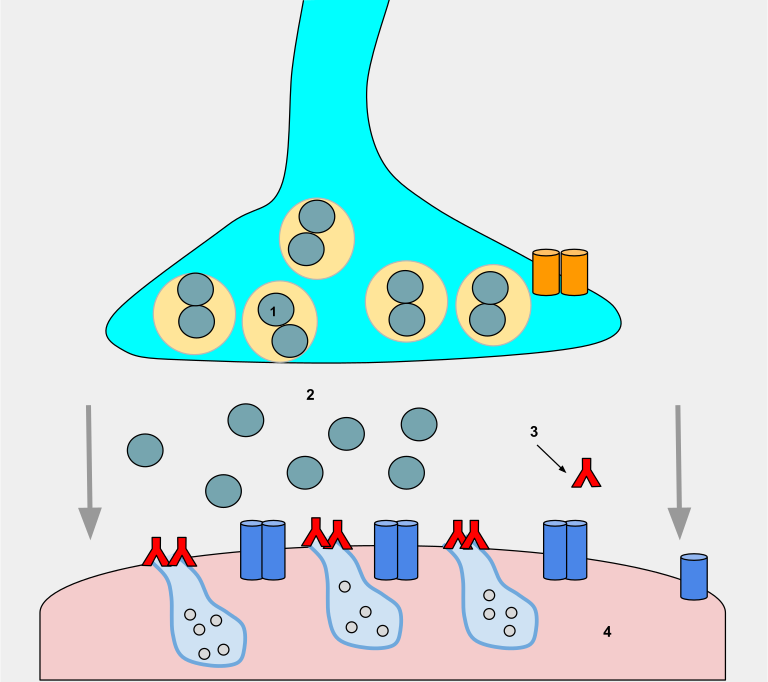
During MG, an autoimmune response causes antibodies to bind to muscle receptor sites. These antibodies block acetylcholine from binding to the muscle receptor sites, thus impairing the transmission of impulses across the neuromuscular junction and causing muscle weakness that worsens with physical activity. See Figure 9.29[3] for an illustration of antibodies (red Ys) binding to muscle receptor sites (light blue cavities on the pink muscle), thus preventing ACh (gray circles) from binding to the muscle receptors and triggering movement.
There is a relationship between the thymus gland and MG. Approximately 65% of people with MG have an abnormal thymus. The thymus is responsible for immunological self-tolerance, which is the capacity to recognize self versus nonself during immunological responses. It is suspected that this loss of the ability to recognize self versus nonself leads to the autoimmune attack on acetylcholine receptors that occurs during MG.[4]
Assessment
The clinical course of MG is variable. Individuals may experience periods of exacerbation and remission of symptoms. MG is a chronic disease, and remissions are rarely permanent. Comprehensive nursing assessment of a client with MG includes a detailed medical history, symptom description, and ability to complete daily activities. The physical exam assesses voluntary muscles for muscle strength and fatigability to identify severity of specific muscle weakness and the degree of functional impairment.
Hallmark characteristics of MG include muscle weakness affecting the eyes, face, neck, jaw, respiratory, and extremity muscles. Weakness increases with repetitive use and improves after periods of rest or sleep. The following box summarizes common manifestations of MG.
Common Manifestations of MG[5]
Early symptoms are as follows:
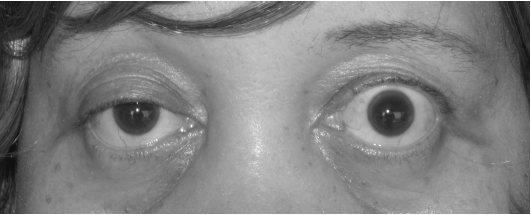
- Eye muscles with diplopia, double vision, and ptosis, drooping of the eyelids. (See Figure 9.30[6] for an image of ptosis.)
- Facial muscle weakness
- Generalized weakness
Ongoing symptoms include the following:
- Dysphonia (voice impairment) due to laryngeal muscle weakness
- Difficulty chewing foods
- Dysphagia (difficulty swallowing), causing high risk for aspiration
- Facial muscle weakness causing a characteristic “myasthenia snarl”
- Dysarthria (difficulty speaking because of weak muscles)
- Neck and limb muscle weakness
- Respiratory muscle weakness leading to breathing difficulty and possible respiratory failure
- Loss of bowel and bladder control
Exacerbations (worsening of symptoms) may be caused by an illness (e.g., viral or respiratory infections), fever, surgery, emotional stress, pregnancy, and drugs that affect neuromuscular transmission.
Potential Complications: Myasthenic Crisis and Cholinergic Crisis
Myasthenic crisis is a medical emergency with respiratory failure due to respiratory muscle weakness. Other signs and symptoms of myasthenia crisis include increased generalized muscle weakness; hypertension; loss of cough and gag reflex; tachycardia; and pale, cool skin. Treatment includes maintaining adequate respiratory function and may require intubation. Neostigmine may be administered.
Cholinergic crisis is respiratory failure resulting from a high dose of cholinesterase inhibitors. Other signs and symptoms of cholinergic crisis include generalized and increased muscle weakness; constricted pupils; bradycardia; increased secretions; diarrhea; abdominal cramping; and red, warm skin. Atropine may be administered and repeated if indicated, resulting in rapid improvement.
See Table 9.11a. for a comparison of myasthenic crisis and cholinergic crisis.
Table 9.11a. Symptoms of MG
| Myasthenic Crisis | Cholinergic Crisis |
|---|---|
| Tachycardia | Bradycardia |
| Flaccid muscles (including respiratory muscles) | Same |
| Pale and cool skin | Red and warm skin |
| No GI changes | Diarrhea and abdominal cramps |
| No changes in secretions | Increased secretions |
| Improves on edrophonium diagnostic test | Worsens on edrophonium diagnostic test |
Common Laboratory and Diagnostic Tests
Because MG affects acetylcholine, an acetylcholinesterase test, commonly referred to as a Tensilon test, is used to diagnose MG. The client is injected with an acetylcholinesterase inhibitor (AChE) called edrophonium chloride. This injection stops the breakdown of acetylcholine, thereby increasing its availability at the neuromuscular junction. The medication acts quickly, within 30 seconds, and only lasts up to 5 minutes. If the client experiences immediate improvement in muscle strength with the injection, it is considered a positive test for MG. If the client does not show transient improvement in muscle strength or improvement of ptosis or respiratory symptoms, then the test results do not indicate MG. During this test, atropine should be available in the event that side effects occur. Side effects are rare but life-threatening and include bradycardia, asystole, and bronchoconstriction.[7]
An EMG may demonstrate a decrease in successive action potentials as the nerves are repetitively stimulated. Read more about the EMG test in the “General Assessment of the Nervous System” section. A CT scan or MRI may be performed to assess for thymus enlargement.
A blood test may be performed to determine if acetylcholine receptor antibodies are present.
Nursing Diagnosis
Myasthenia gravis is a chronic disease, so most clients are managed on an outpatient basis. However, they may be admitted to acute care if secondary conditions occur.
Common nursing diagnoses related to MG include the following[8]:
- Ineffective Airway Clearance related to weak oropharyngeal muscle contractions and decreased ability to cough and swallow
- Risk for Aspiration related to dysphagia and decreased gag reflex
- Fatigue related to disease process and muscular weakness
- Risk for Falls due to weakness and fatigue
Outcome Identification
Overall goals for clients with MG focus on functioning at an optimal level and reducing risk of complications. Sample outcome criteria include the following:
- The client will demonstrate effective coughing after the teaching session.
- The client will demonstrate safe swallowing techniques after the teaching session.
- The client will maintain normal breath sounds.
- The client will verbalize three strategies to manage fatigue after the teaching session.
Interventions
Medical Interventions
Medical management is directed at improving muscle function through the administration of anticholinesterase medications and by reducing and removing circulating antibodies. Clients with MG are managed on an outpatient basis unless hospitalization is required for managing symptoms or complications such as a myasthenic crisis or cholinergic crisis.
Common medications used to manage MG are summarized in Table 9.11b.
Table 9.11b. Medications Used to Treat MG
| Medications | Mechanisms of Action and Nursing Considerations |
|---|---|
| Anticholinesterase Medications
Pyridostigmine bromide Neostigmine bromide Neostigmine methyl sulfate |
These drugs block the action of the enzyme anticholinesterase, producing improvement of symptoms.
Medications must be given on time to maintain stable blood levels. Delays in administration may exacerbate muscle weakness. May be administered intravenously if the client cannot take oral medication. |
| Immunosuppressants
Corticosteroids |
Prescribed if there is no improvement in symptoms from the anticholinesterase drugs to suppressing the client’s autoimmune response.
Goal of therapy is to reduce the number of abnormal antibodies and prevent them from attaching to ACh receptor sites. |
| Nonsteroidal Immunosuppressants
Azathioprine Cyclophosphamide |
Prescribed to suppress autoimmune activity when clients do not respond to corticosteroid therapy. Inhibits T lymphocytes and reduces acetylcholine receptor antibodies.
Can produce extreme immunosuppression and toxic side effects. Leukopenia and hepatotoxicity are serious adverse effects. Monitor white blood cell count and liver function tests. |
Nonpharmacologic management includes plasmapheresis (plasma exchange). During plasmapheresis, the client’s plasma and plasma components are removed, including the antibodies and then the cleansed plasma is returned to the client. This exchange produces a temporary reduction in the level of the acetylcholine circulating antibodies.
Surgical Management
Thymectomy (surgical removal of the thymus gland) may be performed to decrease the autoimmune response.
Physical, Occupational, Speech, and DietaryTherapy
Referral for physical, occupational, and speech therapy can provide a collaborative effort in meeting the complex needs of the client and ensure treatment directed at optimal functioning. Referrals to dieticians help improve nutritional intake for clients who have difficulty swallowing and eating.
Nursing Interventions
Nursing interventions for hospitalized clients with exacerbations of MG or myasthenia crisis are summarized in the following box.
Nursing Interventions for MG[9],[10]
- Monitor the ability to adequately cough and deep breathe.
- Monitor for respiratory failure.
- Maintain suctioning and emergency equipment at the bedside.
- Monitor vital signs.
- Monitor swallowing ability to prevent aspiration.
- Provide nutritional support with small, frequent meals; soft foods; and high-calorie snacks. Encourage the client to keep their chin down when swallowing and to sit up when eating.
- Assess muscle strength.
- Provide teaching on conserving strength and balancing activity/rest periods.
- Plan short activities that coincide with times of maximal muscle strength.
- Encourage rest to reduce fatigue that may trigger a crisis.
- Reposition frequently to prevent pressure injuries.
- Monitor for myasthenic and cholinergic crisis.
- Provide artificial tears during the day. May use eye patch to prevent corneal damage.
- Administer anticholinesterase medications as prescribed.
Health Teaching
Nurses provide health teaching on health promotion to achieve optimal functioning and prevent complications from occurring. Topics include the following:
- Emphasize the importance of rest and avoidance of fatigue to prevent exacerbations. Be alert to other factors that can cause exacerbations, such as infection, surgery, pregnancy, and exposure to extreme temperatures.
- Instruct the client and family about drug actions and side effects.
- Some medications should be avoided or used cautiously because they can worsen symptoms, such as calcium channel blockers, certain classes of antibiotics, hormonal contraceptives, statins, antacids and laxatives that contain magnesium, and transdermal nicotine.
- Take medication in a timely manner. It is advisable to time the dose one hour before meals for optimal chewing and swallowing. Instruct the client to inform the dentist, ophthalmologist, and pharmacist of their MG diagnosis.
- Instruct clients about the symptoms that require emergency treatment.
- Encourage clients to locate a neurologist familiar with MG management.
- Advise clients to wear a medical bracelet identifying the diagnosis of MG. Suggest an “emergency code” to alert family if they are too weak to speak (such as ringing the phone twice and hanging up).
- Instruct the family about cardiopulmonary resuscitation techniques, performance of the Heimlich maneuver, and EMS activation.
- Refer the client to a vocational rehabilitation center for guidance for modifying the home or work environment, such as a raised seat and handrail for the toilet.
- Advise clients to schedule appropriate annual health screenings and maintain recommended vaccinations.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with a family member or other member of the client’s interdisciplinary team.
View a supplementary Wikimedia video[11] on MG: Myasthenia-gravis.
![]() RN Recap: Myasthenia Gravis
RN Recap: Myasthenia Gravis
View a brief YouTube video overview of myasthenia gravis[12]:
- National Institute of Neurological Disorders and Stroke. (2023). Myasthenia gravis. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis ↵
- Colović, M. B., Krstić, D. Z., Lazarević-Pašti, T. D., Bondžić, A. M., & Vasić, V. M. (2013). Acetylcholinesterase inhibitors: pharmacology and toxicology. Current neuropharmacology, 11(3), 315–335. https://doi.org/10.2174/1570159X11311030006 ↵
- “Wikipedia_Project_Myasthenia_gravis_(5).svg” by Libbyspek is licensed under CC BY-SA 4.0 ↵
- American Association of Neuroscience Nurses. (2013). Care of the patient with myasthenia gravis. https://aann.org/uploads/Publications/CPGs/AANN14_CPGMysGravis.pdf ↵
- American Association of Neuroscience Nurses. (2013). Care of the patient with myasthenia gravis. https://aann.org/uploads/Publications/CPGs/AANN14_CPGMysGravis.pdf ↵
- “Ptosis_myasthenia_gravis.jpg” by Mohankumar Kurukumbi, Roger L Weir, Janaki Kalyanam, Mansoor Nasim, Annapurni Jayam-Trouth is licensed under CC BY 2.0 ↵
- Rousseff, R. T. (2021). Diagnosis of myasthenia gravis. Journal of Clinical Medicine. 10(8), 1736. https://doi.org/10.3390/jcm10081736 ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Howard, J. F., Jr. (Ed.). (2009). Myasthenia gravis: A manual for the health care provider. https://myasthenia.org/Portals/0/Provider%20Manual_ibook%20version.pdf ↵
- American Association of Neuroscience Nurses. (2013). Care of the patient with myasthenia gravis. https://aann.org/uploads/Publications/CPGs/AANN14_CPGMysGravis.pdf ↵
- Osmosis.org. (2016, December 12). Myasthenia-gravis.webm [Video]. Wikimedia. CC BY-SA 4.0. https://commons.wikimedia.org/wiki/File:Myasthenia-gravis.webm ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 9 - Myasthenia gravis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/Wbnvm2xCJPY?si=XO91PBIAwYcSdxHD ↵
A chronic, autoimmune, neuromuscular disease that causes weakness in voluntary muscles, including those required for breathing and swallowing.
Double vision.
Drooping of the eyelids.
Voice impairment.
Difficulty swallowing.
Unclear articulation of speech.
Medical emergency with respiratory failure due to respiratory muscle weakness.
Respiratory failure resulting from a high dose of cholinesterase inhibitors.
The withdrawal of whole blood and the removal of red blood cells and then reinfusion of the plasma back into the client.
Surgical removal of the thymus gland.

