8.5 Acute Renal Failure
Acute renal failure (also known as acute kidney injury) is the sudden loss of kidney function. Acute renal failure can be reversible if it is detected early, and intervention is promptly initiated. The condition can happen over a few hours to a few days and reflects the rapid decline in the kidney’s ability to filter waste products and fluids from the blood, resulting in a buildup of waste products and toxins in the blood.
Pathophysiology and Risk Factors
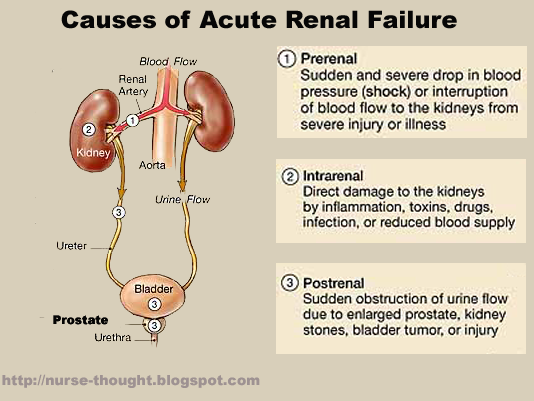
Acute renal failure is the result of three main types of injury to the kidneys referred to as prerenal, intrarenal, and postrenal:
- Prerenal: Prerenal injury is caused by factors external to the kidneys that reduce renal blood flow, resulting in decreased glomerular perfusion and filtration. Examples of prerenal factors are hypovolemia, decreased cardiac output, and vascular obstruction that decrease the amount of circulating volume of blood to the kidneys.
- Intrarenal: Intrarenal injury is caused by conditions that directly damage the renal tissue, resulting in impaired nephron function. Examples of intrarenal injury are prolonged ischemia to the kidneys, nephrotoxins (such as aminoglycoside antibiotics and contrast media), excess hemoglobin released from hemolyzed RBCs, or myoglobin released from necrotic muscle cells.
- Postrenal: Postrenal injury is caused by mechanical obstruction of urinary outflow, resulting in the reflux of urine into the renal pelvis and impaired kidney function. Examples of postrenal injury include benign prostatic hyperplasia, prostate cancer, kidney stones, trauma, and tumors in the urinary tract.
See Figure 8.13[1] for an image of these types of acute renal failure.
Several factors can increase the risk of developing acute renal failure. Acute renal failure is more common in aging individuals due to a natural decline in kidney function. Individuals with underlying health conditions such as chronic kidney disease, diabetes, hypertension, heart failure, liver disease, and autoimmune disorders are also at increased risk. Risk also increases for individuals experiencing dehydration, blood loss/trauma, severe infections, or exposure to toxins.[2],[3]
Assessment
Common symptoms of acute renal failure across body systems are summarized in Table 8.5.
Table 8.5. Manifestations of Acute Renal Failure Across Body Systems[4],[5],[6]
| Body System | Clinical Manifestations of Acute Renal Failure |
|---|---|
| Renal | Oliguria, anuria, and uremia (elevated urea and nitrogenous waste in the blood) |
| Cardiovascular | Hypertension, fluid overload, pitting edema, heart failure, arrhythmias, and pericarditis |
| Respiratory | Dyspnea (shortness of breath from pulmonary edema) and Kussmaul breathing (in severe metabolic acidosis) |
| Gastrointestinal | Nausea, vomiting, anorexia, gastrointestinal bleeding, and gastritis |
| Neurological | Confusion, asterixis (flapping tremor), peripheral neuropathy, seizures, and coma |
| Hematological | Anemia (due to decreased erythropoietin production) and bleeding tendencies/coagulopathies |
| Integumentary | Pruritus, dry skin, pallor, ecchymosis, and uremic frost (whitish coating of urea crystals on the skin when there is a significant buildup of urea in the bloodstream during severe kidney failure) |
| Musculoskeletal | Muscle weakness and muscle cramps |
| Endocrine | Fluid retention, electrolyte imbalances (i.e., hyperkalemia, hyponatremia), metabolic acidosis, and insulin resistance |
Diagnostic Testing
Laboratory studies and diagnostic imaging tests are used to identify the cause and severity of acute renal failure. Blood tests commonly performed include serum creatinine, blood urea nitrogen (BUN), and glomerular filtration rate (GFR) that demonstrate elevated creatinine and BUN with decreased GFR. Electrolyte and acid-base abnormalities during acute renal failure include elevated potassium levels, low sodium levels, and metabolic acidosis. A complete blood cell count (CBC) may reflect anemia as the result of decreased erythropoietin production. Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Urinalysis and renal ultrasound may also be performed to assess for potential causes of failure such as structural abnormalities, obstruction, or infection.[7]
Nursing Diagnoses
Nursing diagnoses for clients with acute renal failure help guide nursing care and address the specific needs of these individuals. Common nursing diagnoses for acute renal failure include the following:
- Decreased Urinary Output
- Electrolyte Imbalance
- Fluid Volume Excess
- Risk for Bleeding
- Imbalanced Nutrition
- Anxiety
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Examples of expected outcomes for clients with acute renal failure are as follows:
- The client will exhibit a gradual increase in urinary output to within normal limits, maintaining a minimum of 30 mL/hour, indicating improved renal perfusion and function within 24 hours.
- The client’s electrolyte levels (potassium, sodium, calcium) will be within normal ranges within 48 hours, demonstrating restored electrolyte balance and renal function stability.
- By discharge, the client will maintain stable body weight, absence of edema, and balanced intake/output, indicating effective fluid volume management by the kidneys.
- The client will demonstrate an increase in nutritional intake, maintaining adequate calorie and nutrient intake, achieving weight stabilization, and reporting improved appetite and energy levels within one week.
Interventions
Medical Interventions
Medical interventions to treat acute renal failure focus on identifying and correcting the underlying causes, restoring kidney function, and preventing lasting damage to the kidneys. Common underlying causes of acute kidney failure requiring treatment include hypotension, sepsis, heart failure, renal obstructions, medication toxicity, and dehydration. Medical interventions may include fluid management, medication management, electrolyte management, nutritional support, dialysis, and surgery[8],[9],[10]:
- Fluid Management: Intravenous fluids may be administered cautiously to restore adequate circulating blood volume while also closely monitoring for fluid overload.
- Medication Management: Potentially nephrotoxic drugs are identified. Medications are prescribed to treat underlying causes, such as infection. Diuretics may be used cautiously to manage fluid overload in some cases.
- Electrolyte Management: High potassium levels are common during acute renal failure and can result in serious complications like cardiac dysrhythmias. Insulin with glucose and/or potassium binders may be prescribed to quickly lower potassium levels in the blood.
- Nutritional Support: Nutritional intake, especially protein, potassium, sodium, phosphorus, and fluids, may be restricted to support kidney function and prevent fluid overload.
- Surgery: In situations of obstruction or severe damage, surgical interventions like stent placement, nephrostomy, or other corrective procedures may be performed.
- Dialysis: Hemodialysis or peritoneal dialysis may be needed in cases of severe renal impairment due to the accumulation of significant waste and fluids. Continuous renal replacement therapy may be used when more gradual removal of fluids and wastes is needed due to hemodynamic instability. Read more information about different types of dialysis in the following box.
A Closer Look at Dialysis…
Dialysis is a procedure to artificially perform the functions of the kidneys when they are unable to effectively filter waste products and excess fluids from the blood. There are three main types of dialysis.
Hemodialysis
- Procedure: Hemodialysis involves using a machine called a dialyzer or artificial kidney. Blood is removed from the body through a catheter or arteriovenous fistula/graft, circulated through the dialyzer to remove waste and excess fluid, and then returned to the body. It is important for nurses to know what medications should be held prior to dialysis because they will be dialyzed out or may cause hypotension.
- Access: Vascular access is crucial and is typically established through a surgically created arteriovenous fistula or arteriovenous graft that is only used for dialysis. A central venous catheter may also be used.
- Frequency: Hemodialysis is usually performed several times a week in sessions lasting around three to four hours each, but frequency may vary based on the client’s needs and condition.
Peritoneal Dialysis
- Procedure: Peritoneal dialysis uses the peritoneum, a membrane lining the abdominal cavity, as a natural filter. A catheter is placed into the abdomen, and a special fluid (dialysate) is introduced and drained out after a dwell time, allowing waste products and excess fluids to pass from the blood into the dialysate.
- Access: A catheter is surgically placed in the abdomen to allow access for the dialysis solution. The fluid is typically straw colored in the dialysate.
- Frequency: Continuous Ambulatory Peritoneal Dialysis (CAPD) involves manual exchanges multiple times a day, while Continuous Cycling Peritoneal Dialysis (CCPD) uses a machine for automated exchanges during the night.
Continuous Renal Replacement Therapy (CRRT)
- Procedure: CRRT is a slow and continuous form of dialysis that occurs 24 hours a day, emulating the continuous filtration process of the kidneys. Blood is continuously removed from the body via a catheter and passed through a machine that filters waste products and excess fluids before returning the filtered blood to the client.
- Access: Similar to hemodialysis, a catheter is placed in a large vein, typically the jugular or femoral vein, for vascular access.
- Frequency: CRRT is continuous and runs over an extended period, often days to weeks, providing slower and gentler fluid and solute removal compared to traditional hemodialysis.
View a supplementary YouTube video[11] on dialysis: Procedure of DIALYSIS.
Nursing Interventions
Nursing interventions for acute renal failure are aimed at managing symptoms, supporting kidney function, preventing complications, and promoting overall client well-being.
Medication Management
During inpatient care, nurses administer medications while considering safe dosage ranges based on kidney function tests like serum creatinine. Health teaching is provided regarding the purpose of medications, common side effects, and when to notify the provider.
Monitor Fluid and Electrolyte Balance
Fluid intake and urine output are closely monitored and documented. Although nurses may delegate the measurement and documentation of fluid intake and output to unlicensed assistive personnel (UAPs), they must ensure it is measured and documented accurately. Registered nurses analyze intake/output data per shift, as well as trended data over 24 hours, and promptly communicate fluid imbalance concerns to the health care provider. If fluid imbalance occurs, appropriate strategies are implemented (such as fluid restriction and diuretic administration for fluid overload, or IV fluid administration for hypovolemia).
Weight is also closely monitored as an indicator of fluid balance. Daily weights are commonly prescribed for clients receiving dialysis.
Electrolyte levels are closely monitored (i.e., potassium, sodium, calcium, phosphorus, and magnesium), and abnormal levels are promptly communicated to the health care provider. Nurses also collaborate with dieticians to plan appropriate diet selections, considering potential restrictions in protein, sodium, potassium, and phosphorus.
Health Teaching
Health teaching is provided regarding medications, dietary and fluid restrictions, and follow-up care. Signs and symptoms requiring immediate medical attention are reinforced.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Acute Renal Failure
RN Recap: Acute Renal Failure
View a brief YouTube video overview of acute renal failure[12]:
- This is a derivative of “causesofacuterenalfailure.png” by Cassio Lymn and is used under Fair Use. Access for free at https://fundamentalsofnursingblog.wordpress.com/2016/12/15/acute-kidney-injury/ ↵
- Goyal, A., Daneshpajouhnejad, P., Hashmi, M. F., et al. (2023). Acute Kidney Injury. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441896/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. (2023). Acute kidney failure. https://medlineplus.gov/ency/article/000501.htm ↵
- Goyal, A., Daneshpajouhnejad, P., Hashmi, M. F., et al. (2023). Acute Kidney Injury. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441896/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. (2023). Acute kidney failure. https://medlineplus.gov/ency/article/000501.htm ↵
- Mayo Clinic. (2024). Acute kidney failure. https://www.mayoclinic.org/diseases-conditions/kidney-failure/diagnosis-treatment/drc-20369053 ↵
- Goyal, A., Daneshpajouhnejad, P., Hashmi, M. F., et al. (2023). Acute Kidney Injury. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441896/ ↵
- Goyal, A., Daneshpajouhnejad, P., Hashmi, M. F., et al. (2023). Acute Kidney Injury. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441896/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. (2023). Acute kidney failure. https://medlineplus.gov/ency/article/000501.htm ↵
- Mayo Clinic. (2024). Acute kidney failure. https://www.mayoclinic.org/diseases-conditions/kidney-failure/diagnosis-treatment/drc-20369053 ↵
- 7activestudio. (2016, November 27). Procedure of DIALYSIS [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=EU2skU3bgS8&t=19s ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 8 - Acute renal failure [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/9Dh3VnhlcXc?si=XF9UdrOEx0CH9aa9 ↵
The sudden loss of kidney function.
Elevated urea and nitrogenous waste in the blood.
Flapping tremor.
Whitish coating of urea crystals on the skin when there is a significant buildup of urea in the bloodstream during severe kidney failure.
A procedure to artificially perform the functions of the kidneys when they are unable to effectively filter waste products and excess fluids from the blood.
Involves the use of using a machine called a dialyzer or artificial kidney. Blood is removed from the body through a catheter or arteriovenous fistula/graft, circulated through the dialyzer to remove waste and excess fluid, and then returned to the body.
Dialysis using the peritoneum, a membrane lining the abdominal cavity, as a natural filter.
Peritoneal dialysis involving manual exchanges multiple times a day.
Peritoneal dialysis using a machine for automated exchanges during the night.
A slow and continuous form of dialysis that occurs 24 hours a day, emulating the continuous filtration process of the kidney.

