8.3 General Urinary System Assessment
When evaluating a client for possible disorders of the urinary system, the nurse acknowledges individual and population risk factors, cultural influence, and socioeconomic factors that may impact health.
Risk Factors
Several risk factors can contribute to the development of urinary system alterations, and these factors may vary in their impact from person to person[1],[2]:
- Age: As individuals age, the glomerular and tubular membranes thicken, and the tubules also decrease in length, decreasing glomerular filtration. Due to these physiological changes, many older adults experience nocturnal polyuria. Furthermore, most men experience benign prostate enlargement as they age, resulting in bladder outlet obstruction. This obstruction causes incomplete bladder emptying, resulting in symptoms of frequent urination in small amounts throughout the day and night.[3]
- Genetics: Family history of kidney disease can increase the risk of certain kidney conditions, such as polycystic kidney disease and chronic kidney disease.
- Concurrent Medical Conditions:
- Hypertension: Uncontrolled high blood pressure is a leading cause of kidney damage. High blood pressure can damage blood vessels in the kidneys, reducing their ability to function properly.
- Diabetes mellitus, type 1 and type 2: Elevated blood sugar can damage the small blood vessels of the kidneys over time.
- Atherosclerosis: Impacts blood flow to the kidneys.
- Autoimmune diseases: May damage the kidneys due to sustained inflammatory processes.
- Urinary tract infections: Recurrent infections may spread to the kidney, resulting in damage and scarring.
- Urinary obstructions: Blockages in the urinary tracts due to kidney stones, prostate enlargement, or tumors may lead to urinary tract infections and reduced kidney function.
- Drugs & Smoking: Many drugs, including prescription and illicit drugs, can damage the kidneys, especially if used for sustained periods. Smoking increases the risk of hypertension and atherosclerosis, subsequently resulting in damage to the kidneys.
- Toxins: Exposure to heavy metals and solvents may result in damage to the kidneys.
Cultural Factors
Cultural factors can influence various aspects of health, including urinary health. Cultural beliefs and health practices can impact an individual’s lifestyle choices. For example, some cultures may consume diets that are high in salt, processed foods, and protein that can potentially lead to hypertension and increased risk for kidney damage. Individuals who participate in fasting rituals may also sustain dehydration or electrolyte imbalances, which can result in kidney damage. Individuals who elect to use alternative healing methods or traditional medicines, such as specific herbs and rituals, may also experience increased risk to the kidneys. Delays in seeking medical treatment for kidney disorders can result in lasting kidney damage. Additionally, many ethnic groups such as African Americans, Hispanics, and Native Americans have a higher risk of developing kidney disease.[4]
Socioeconomic Factors
Socioeconomic factors play a significant role in shaping health outcomes, including the development and progression of urinary system alterations. Individuals with lower socioeconomic status often face barriers to accessing and paying for health care, have limited resources for preventive measures, and may be exposed to environmental factors that can contribute to kidney problems. They may work in environments with exposure to toxins or pollutants that increase risk of kidney diseases. Individuals may elect to avoid routine checkups and laboratory monitoring or delay medical treatment like dialysis due to costs. Omissions in care and timely intervention may result in sustained and exacerbated kidney damage. Additionally, individuals with lower health literacy may also experience increased challenges in navigating the health care system and following recommendations related to their urinary system health.[5]
Assessment
Healthy kidney functioning is essential for regulating fluid and electrolyte balances, blood pH balance, blood pressure, and red blood cell production. Assessment of urinary system functioning includes obtaining a health history, performing a physical examination, and reviewing diagnostic test results. A thorough assessment allows for early detection and management of potential urinary system issues and helps prevent the progression of alterations to more advanced stages.
Health History
Many health history factors can influence the emergence of a urinary system alteration. Completing a detailed health history can provide evidence of areas of potential concern. When nurses suspect a potential alteration, specific assessment questions may reveal clues as to a diagnosis. Questions examining recent urinary changes, including urinary output, increased urinary frequency, urinary incontinence, a sense of urgency, pain with urination, difficulty starting urine flow, or difficulty emptying one’s bladder, may offer guiding insight into a potential urinary system disorder.
Medications and diet can also impact urinary system health. Fluid and dietary intake should be closely examined for potential dehydration and the presence of salt and protein in meal choices. Additionally, any recent imaging studies are important to note because the use of contrast dyes can potentially damage the kidneys and diminish renal function.[6],[7]
Physical Assessment
Urinary system alterations can impact other body systems. Early identification of abnormal findings and notification of the health care provider can lead to prompt intervention and help prevent lasting damage to the kidneys and other organs. See Table 8.3 for a summary of abnormal findings by body system related to urinary system alterations.
Table 8.3. Abnormal Findings by Body System Related to Urinary System Disorders[8],[9],[10]
| Body System | Abnormal Findings Related to Urinary Disorders |
|---|---|
| Urinary System | Hematuria, oliguria, polyuria, dysuria, frequency, urgency, cloudy or foul-smelling urine, pus in urine, or presence of bloody/purulent discharge on urinary meatus. |
| Cardiovascular | Edema (due to fluid retention), hypertension, abnormal heart rhythm (due to electrolyte imbalances), or heart murmur (related to fluid overload). |
| Gastrointestinal | Nausea, vomiting, constipation. |
| Skin | Pallor, yellow/grayish color, dry skin, or pruritus. |
| Neurological | New onset confusion or altered mental status, seizures, or other neurological symptoms. Uremic encephalopathy is a cerebral dysfunction caused by the accumulation of toxins resulting from acute or chronic kidney failure. |
| Musculoskeletal | Bone pain or tenderness (related to mineral imbalances during acute or chronic kidney failure), muscle cramps, fatigue, or weakness. |
Review health history questions and physical assessment of the genitourinary system in the “Gastrointestinal and Genitourinary Assessment” section of the “Abdominal Assessment” chapter of Open RN Nursing Skills, 2e.
Life Span Considerations
The following characteristics should be considered for older adult and pediatric populations.[11],[12],[13]
Older Adult Considerations
- As individuals age, the glomerular and tubular membranes thicken, and the tubules also decrease in length, causing decreased glomerular filtration. Due to these physiological changes, many older adults experience nocturnal polyuria.
- Most men experience benign prostate enlargement as they age, resulting in bladder outlet obstruction. This obstruction causes incomplete bladder emptying, resulting in symptoms of frequent urination in small amounts throughout the day and night.
- In elderly clients, changes in mental status may be the presenting symptom of a urinary tract infection.
- Aging results in a decline in function for the urinary and renal systems. In addition, underlying diseases, sleep patterns, habits and use of medications may result in nocturia.
- Urinary urgency, urinary frequency, urinary retention, and urinary incontinence are also common concerns for older adults.
- As individuals get older, changes in bladder muscle tone and function and weakened pelvic floor muscles can increase the incidence of urinary incontinence.
Pediatric Considerations
- Children have a faster metabolic rate and expend more calories, resulting in a higher requirement for fluids.
- Infants have a greater body surface area, compared to their weight, which may lead to water loss from skin.
- Due to immature tubular function, sodium may be dysregulated.
- Loss of water from a decreased ability to concentrate urine may affect small children.
- Immature glomerular filtration, tubular secretion, and reabsorption reduce renal excretion of medications.
- Expected urinary output is calculated in mL/kg/hr. The expected urine output for an infant and child is 1-2mL/kg/hr. For an adolescent, urine output should be 0.5-1mL/kg/hr.
- In infants, the reflex to urinate is active, but as toddlers mature, they learn how to override the reflex and control the external sphincter, thus delaying voiding until it is appropriate to do so (commonly referred to as “potty training”).
- To assess for urine output in infants and toddlers, assess the frequency of wet diapers and the daily number of wet diapers. In hospitalized infants and toddlers, the diapers may be weighed for precise measurements of urine output.
- Enuresis in children is considered normal unless it continues past seven or eight years of age, when it should be addressed with a pediatrician.
Diagnostic Testing
Definitive signs of a urinary system alterations are often reflected in blood and urine tests. Tests are ordered by health care providers based on signs and symptoms that may reflect a suspected disorder.
Blood Tests
Common blood tests for diagnosing and monitoring kidney function include serum creatinine, blood urea nitrogen (BUN), and glomerular filtration rate. Other blood tests used to diagnose and monitor urinary system alterations include electrolyte panel, albumin, serum protein, and complete blood count[14]:
- Serum Creatinine: Creatinine is a waste product that is produced by the breakdown of muscle and must be filtered out by the kidneys. Elevated creatinine levels may indicate kidney dysfunction because of their decreased ability to effectively filter creatinine out of the bloodstream.
- Blood Urea Nitrogen (BUN): BUN is a measurement of the amount of nitrogen present in the bloodstream. Nitrogen is produced from urea, a waste product from the liver when proteins are broken down. Elevated BUN levels can indicate kidney damage because of decreased ability to filter urea out of the bloodstream. However, BUN levels can also be elevated due to dehydration or from increased protein in the diet.
- Glomerular Filtration Rate (GFR): GFR estimates how well the kidneys are filtering waste from the blood. eGFR is a standardized calculation reflecting the amount of creatinine in the blood based on the client’s age and gender. In adults with healthy kidneys, the glomerular filtration rate is 90 mL per minute or higher. Kidney damage causes this number to decrease. See more information about GFR rates and kidney damage in the “Chronic Kidney Disease” section of this chapter.
- Electrolyte Panel (Sodium, Potassium, Calcium, Phosphorus): The kidneys help regulate electrolyte balance in the bloodstream. Clients with kidney dysfunction often experience elevated levels of potassium, phosphate, and magnesium and decreased levels of sodium and calcium. Abnormal electrolyte levels affect the transmission of impulses in the nerves and muscles throughout the body, which can have serious implications. For example, potassium imbalance can cause life-threatening cardiac dysrhythmias.
- Serum Albumin: Albumin is a protein in the blood that helps maintain fluid balance inside and outside of blood vessels. Healthy kidneys retain albumin and keep normal levels in blood vessels, thus keeping fluid inside the blood vessels. Kidney damage results in the kidneys being unable to retain albumin, causing low levels of albumin in blood vessels. When albumin levels are decreased, fluid leaks out of blood vessels into interstitial areas around tissues, referred to as “third spacing.”
- Serum Protein: Individuals with kidney dysfunction can also experience abnormal levels of other blood proteins like globulins due to impaired filtering.
- Complete Blood Cell Count (CBC): Many clients with kidney dysfunction have decreased production of erythropoietin by the kidneys, which stimulates red blood cell production. As a result, they often experience anemia due to decreased red blood cell (RBC) levels.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Urine Tests
Common urine tests diagnosing and monitoring urinary system alterations include urinalysis, urine culture and sensitivity, composite urine collection, and creatinine clearance.
- Urinalysis (UA): A urine sample is collected and analyzed for several elements, including the following:
- Color, Odor, and Turbidity: Color ranges from pale yellow to amber. Changes in color can indicate conditions like dehydration or hematuria (blood in the urine). Urine can have a mild ammonia-like odor, but malodorous urine is a sign of infection. Normal urine is clear. Turbidity (cloudiness) can indicate the presence of particles like bacteria, white blood cells, or crystals.
- Specific Gravity: Specific gravity refers to the concentration of solutes in the urine, a measurement that reflects the kidney’s ability to concentrate urine. Low specific gravity values indicate dilute urine, and high levels indicate concentrated urine.
- pH: pH measures the acidity or alkalinity of the urine. Normal pH ranges from 4.6 to 8.0. Abnormal pH can be the result of diet, medications, or conditions like infection, acidosis, or alkalosis.
- Glucose: Normally, there is no glucose in urine. Glucose in urine indicates high blood glucose levels and possible diabetes mellitus.
- Ketones: Normally, there are no ketones in the urine. The presence of ketones indicates the body is metabolizing fats for energy, which can be caused by fasting, a carbohydrate-restricted diet, or a complication of diabetes mellitus called diabetic ketoacidosis.
- Protein: Elevated levels of protein in the urine can indicate kidney damage.
- Leukocyte Esterase & Nitrates: The presence of leukocyte esterase and nitrates indicates a bacterial infection.
- Cells, Casts, Crystals, and Bacteria: The presence of red blood cells, white blood cells, or epithelial cells in the urine suggests underlying conditions like kidney disease or urinary tract issues. Different types of casts (hyaline, granular, cellular, etc.) can indicate damage within the kidney tubules. Crystals can form due to changes in urine composition, indicating potential conditions like urinary tract infections, kidney stones, or metabolic disorders. The presence of bacteria can indicate a urinary tract infection or contamination of the urine sample by normal flora.
- Urine Culture and Sensitivity: A urine culture and sensitivity test is used to identify the presence of bacteria or other microorganisms in the urine and determine the most effective antibiotics for treating a bacterial infection.
- Composite Urine Collections: Composite urine collections involve combining multiple urine samples collected over a specific time period to create a single representative sample for analysis. Two types of composite urine collections are timed urine collections and pooled or mixed collections.
- Timed Urine Collection: This method involves collecting all urine produced over a specified time period, such as over 24 hours or a shorter duration (e.g., 2, 4, or 12 hours). This collection is used for evaluating substances in the urine like creatinine, protein, or certain hormones that require accurate measurements of total urine output within a specific time frame.
- Pooled or Mixed Urine Samples: In this approach, smaller urine samples are collected at various intervals, such as morning, afternoon, and evening. These samples are pooled together to create a composite sample. This method can be used for general analysis or to monitor changes in urinary components throughout the day, such as variations in electrolyte levels or hormones.
- Creatinine Clearance: Creatinine clearance is a urine test used to estimate the glomerular filtration rate (GFR). Creatinine clearance is calculated based on the amount of creatinine cleared from the blood by the kidneys over a 24-hour period. The test requires collecting a 24-hour urine sample, as well as a blood sample to calculate the clearance rate. The calculation is (urine concentration x urine volume) divided by the serum creatinine concentration. A lower creatinine clearance reflects reduced kidney function, and a higher creatinine clearance reflects improved kidney function.[15]
Imaging Studies
Common imaging studies used to diagnose urinary system alterations include bladder ultrasound, KUB imaging, IV urography/IV pyelogram, CT scan, and cystoscopy[16],[17]:
- Bladder Ultrasound: A bladder ultrasound assesses the bladder’s size, shape, and emptying ability and is useful for identifying thickened tissue, masses, or obstructions within the urinary tract. Bladder ultrasounds can also measure post-void residuals, reflux of urine from the bladder into the ureters, and the presence of urinary tract inflammation.
- Kidneys, Ureters, Bladder (KUB): KUB refers to radiographic imaging of the abdomen with or without contrast dye to assess the kidneys, ureters, and bladder.
- IV Urography/ IV Pyelogram: IV urography, also called IV pyelogram, uses contrast dye administered intravenously and radiographic imaging taken at specific intervals to visualize the urinary system, including the kidneys, ureters, and bladder, as the contrast dye is filtered by the kidneys and eliminated from the body. Nursing priorities prior to procedures that use contrast dye include assessing for allergies and reviewing kidney function test results. Nurses also teach clients about the importance of water consumption following the procedure to aid in flushing the dye from the kidneys.
- Computed Tomography (CT) Scan: A CT scan is an imaging procedure that uses a combination of X-rays and computer technology to produce a variety of images of the urinary tract looking for disease, cancer, obstructions, and other disorders.[18]
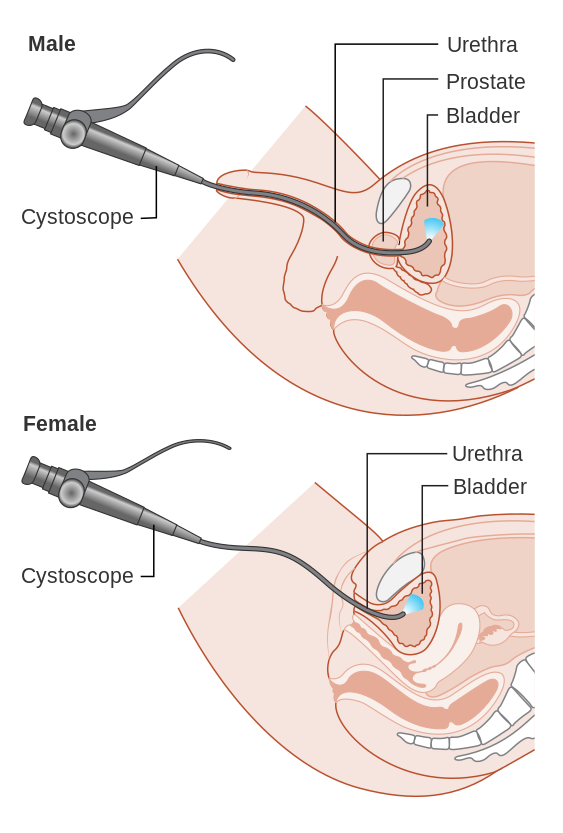
- Cystoscopy: A cystoscopy is performed by a urologist who uses a cystoscope to look inside the urethra and bladder. A cystoscope is a long, thin optical instrument with an eyepiece at one end, a rigid or flexible tube in the middle, and a tiny lens and light at the other end of the tube. The urologist fills the bladder with fluid and looks at detailed images of the urethra and bladder on a computer monitor. During a cystoscopy, the urologist can see kidney stones, tumors, strictures or narrowing of the urethra, and other signs of blockage, such as an enlarged prostate gland. Treatments may also be performed during the procedure, such as removing a stone, taking a sample of the urethra or bladder tissue for a biopsy, injecting medicines into the bladder to treat urinary leakage, or removing abnormal tissue.[19] See Figure 8.12[20] for an illustration of cystoscopy.
- Cerqueira, D., Tavares, J. R., & Machado, R. C. (2014). Predictive factors for renal failure and a control and treatment algorithm. Revista Latino- Americana de Enfermagem, 22(2), 211-7. https://doi.org/10.1590/0104-1169.3048.2404 ↵
- Kuma, A., & Kato, A. (2022). Lifestyle-related risk factors for the incidence and progression of chronic kidney disease in the healthy young and middle-aged population. Nutrients, 14(18), 3787. https://doi.org/10.3390/nu14183787 ↵
- Kallas, H. E., Chintanadilok, J., Maruenda, J., Donahue, J. L., & Lowenthal, D. T. (1999). Treatment of nocturia in the elderly. Drugs & Aging, 15(6), 429–437. https://doi.org/10.2165/00002512-199915060-00003 ↵
- Hassan, M. O., & Balogun, R. A. (2022). The effects of race on acute kidney injury. Journal of Clinical Medicine, 11(19), 5822. https://doi.org/10.3390/jcm11195822 ↵
- Anandh, U., Meena, P., Karam, S., & Luyckz, V. (2022). Social, political, and legal determinants of kidney health: Perspectives from lower- and middle-income countries with a focus on India. Frontiers in Nephrology, 2, 1-11. https://doi.org/10.3389/fneph.2022.1024667 ↵
- National Kidney Foundation. (n.d.). Kidney disease: The basics. https://www.kidney.org/news/newsroom/fsindex ↵
- Inker, L. A., & Perrone, R. D. (2023). Assessment of kidney function. https://www.uptodate.com/ ↵
- National Kidney Foundation. (n.d.). Kidney disease: The basics. https://www.kidney.org/news/newsroom/fsindex ↵
- Inker, L. A., & Perrone, R. D. (2023). Assessment of kidney function. https://www.uptodate.com/ ↵
- Maddukuri, G. (2022). Evaluation of the renal patient. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/approach-to-the-genitourinary-patient/evaluation-of-the-renal-patient ↵
- State-wide Emergency Care of Children Working Group. (2024). CHQ-NSS-51033 Anatomical and Physiological Differences in Children. Children's Health Queensland Hospital and Health Service. https://www.childrens.health.qld.gov.au/__data/assets/pdf_file/0031/179725/how-children-are-different-anatomical-and-physiological-differences.pdf ↵
- Lu, H., & Rosenbaum, S. (2014). Developmental pharmacokinetics in pediatric populations. Journal of Pediatric Pharmacology Therapeutics, 19(4), 262-76. https://doi.org/10.5863/1551-6776-19.4.262 ↵
- Kujubu, D. A. (2009). Chapter 19: Nocturia in elderly persons and nocturnal polyuria. American Society of Nephrology. https://www.asn-online.org/education/distancelearning/curricula/geriatrics/Chapter19.pdf ↵
- Gounden, V., Bhatt, H., & Jialal, I. (2024). Renal Function Tests. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK507821/ ↵
- Gounden, V., Bhatt, H., & Jialal, I. (2024). Renal Function Tests. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK507821/ ↵
- Centers for Disease Control and Prevention. (n.d.). Kidney testing: Everything you need to know. https://www.cdc.gov/kidney-disease/ ↵
- American Kidney Fund. (2023). Tests for kidney disease. https://www.kidneyfund.org/all-about-kidneys/tests-kidney-disease ↵
- Johns Hopkins Medicine. (n.d.). Computed tomography (CT or CT scan) of the kidney. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ct-scan-of-the-kidney ↵
- National Institute of Diabetes and Digestive and Kidney Disorders. (2021). Cystoscopy & ureteroscopy. National Institutes of Health. https://www.niddk.nih.gov/health-information/diagnostic-tests/cystoscopy-ureteroscopy ↵
- “Diagram_showing_a_cystoscopy_for_a_man_and_a_woman_CRUK_064.svg” by Cancer Research UK is licensed under CC BY-SA 4.0 ↵
A cerebral dysfunction caused by the accumulation of toxins resulting from acute or chronic kidney failure.
Abnormal accumulation of fluid within interstitial spaces causing swelling within tissues.
Cloudiness of urine caused by the presence of suspended particles that are not easily seen.

