8.2 Review of Anatomy & Physiology of the Urinary System
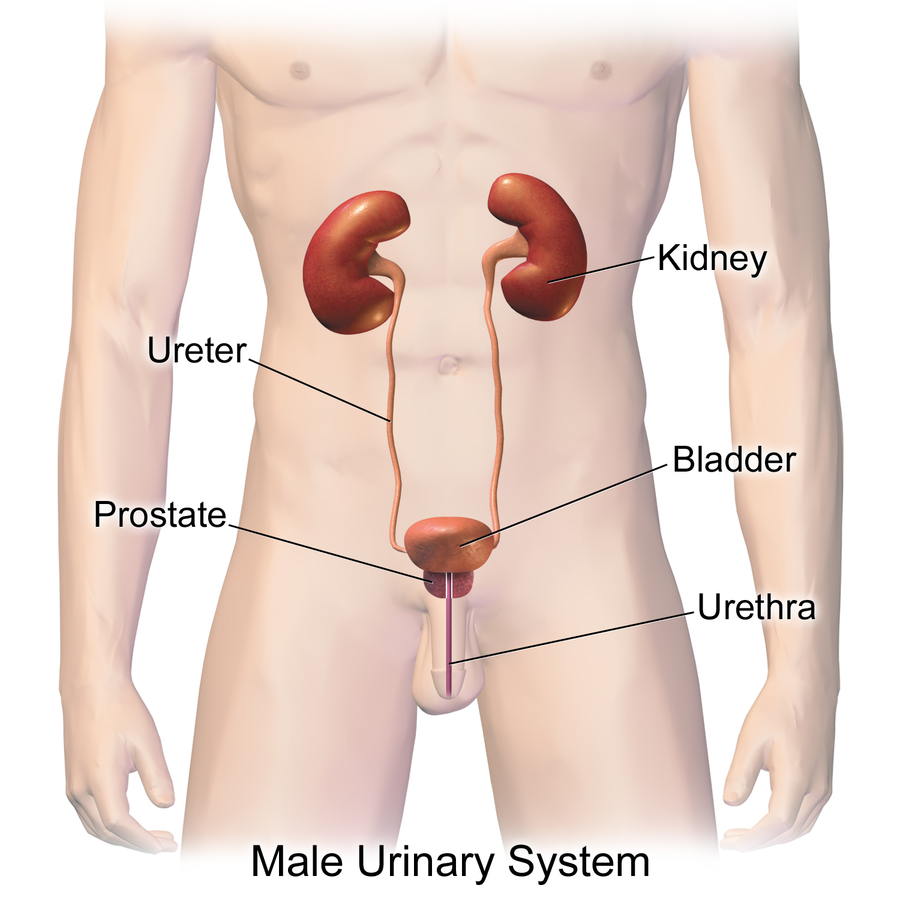
The urinary system, also referred to as the renal system or urinary tract, consists of the kidneys, ureters, bladder, and urethra. The kidneys form urine, and the ureters carry the urine away from kidneys to the urinary bladder, where it is stored until it is expelled during urination. The urethra carries the urine from the urinary bladder to outside of the body during urination.[1] See Figure 8.1[2] for an illustration of the male urinary system.
Kidneys
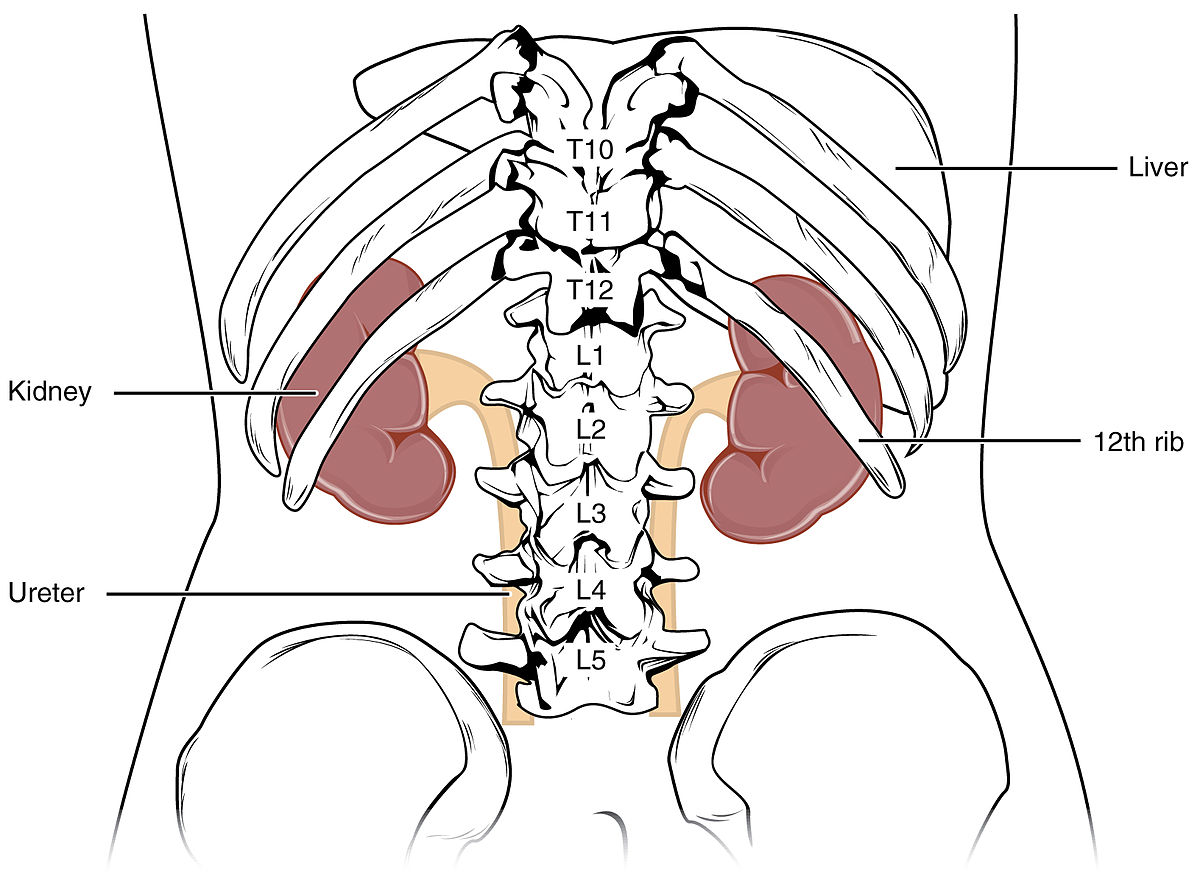
The kidney is an organ that filters waste from the blood and produces urine. Kidneys lie on either side of the spine behind the abdominal cavity, well-protected by muscle, fat, and ribs. Because they lie posterior to the peritoneum membrane, their location is described as retroperitoneal. They are roughly the size of your fist. The male kidney is typically a bit larger than the female kidney. The kidneys are well-vascularized, receiving about 25 percent of the blood pumped out of the heart with each heartbeat. Figure 8.2[3] displays the location of the kidneys.
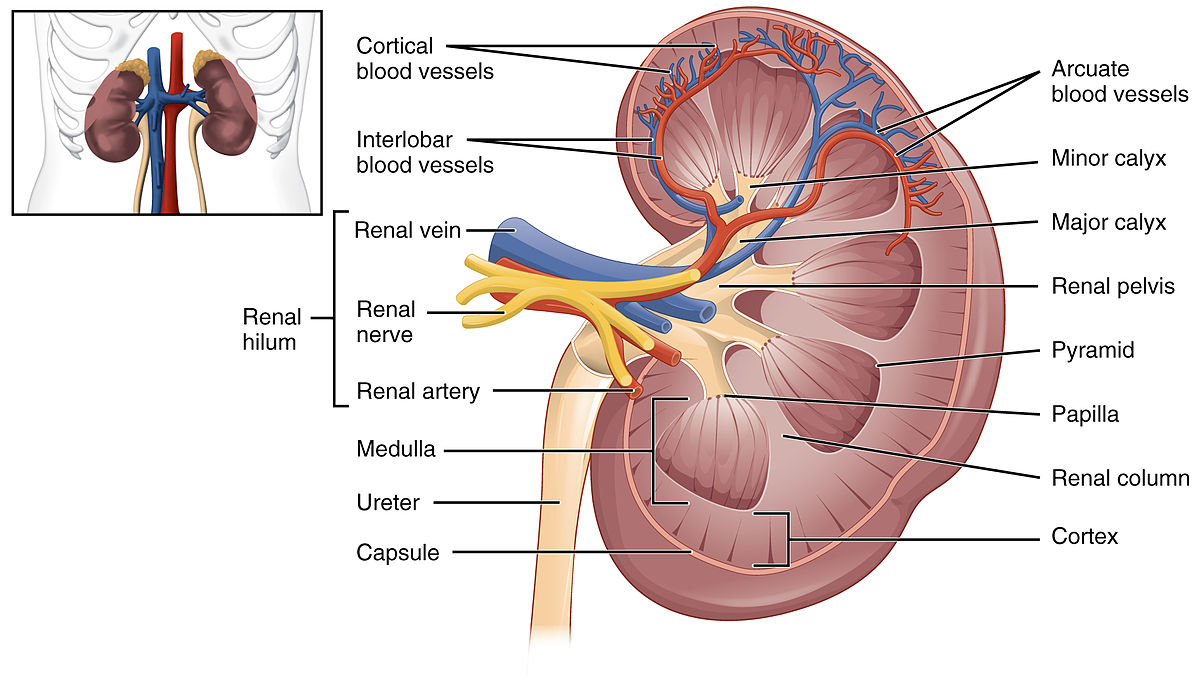
The outer region of the kidney is called the renal cortex, and the inner region is called the medulla. See Figure 8.3[4] for an illustration of the internal structures of the kidney. The renal hilum is the entry and exit site for vessels, nerves, and ureters. The renal arteries (colored red) come directly from the descending aorta, and the renal veins (colored blue) return filtered blood to the inferior vena cava.
Arterioles and Nephrons
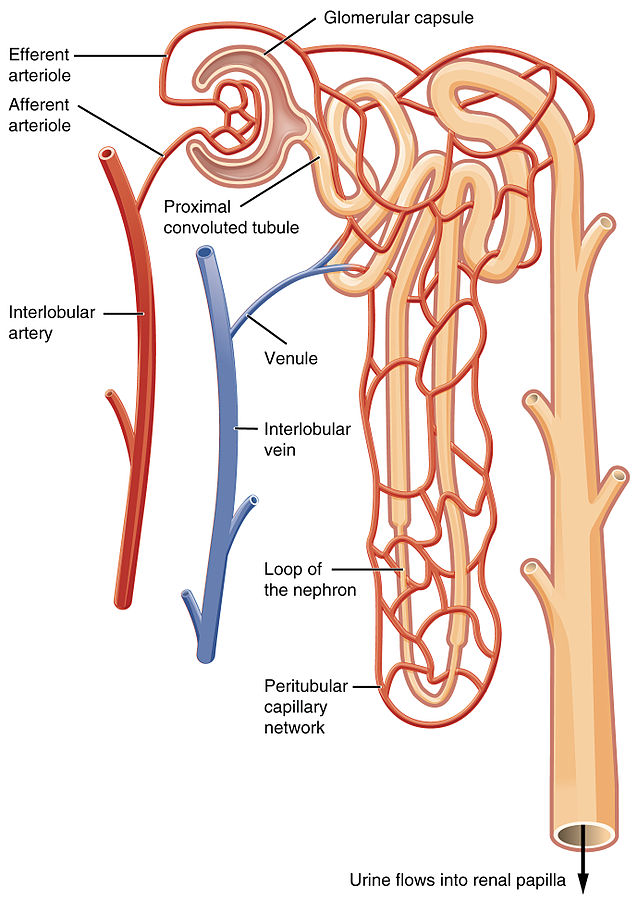
The renal artery branches down into small arteries called afferent arterioles that bring blood to the nephron. Afferent arterioles service about 1.3 million nephrons in each kidney. See Figure 8.4[5] for an illustration of blood flow from the renal artery to the afferent arterioles to a nephron.
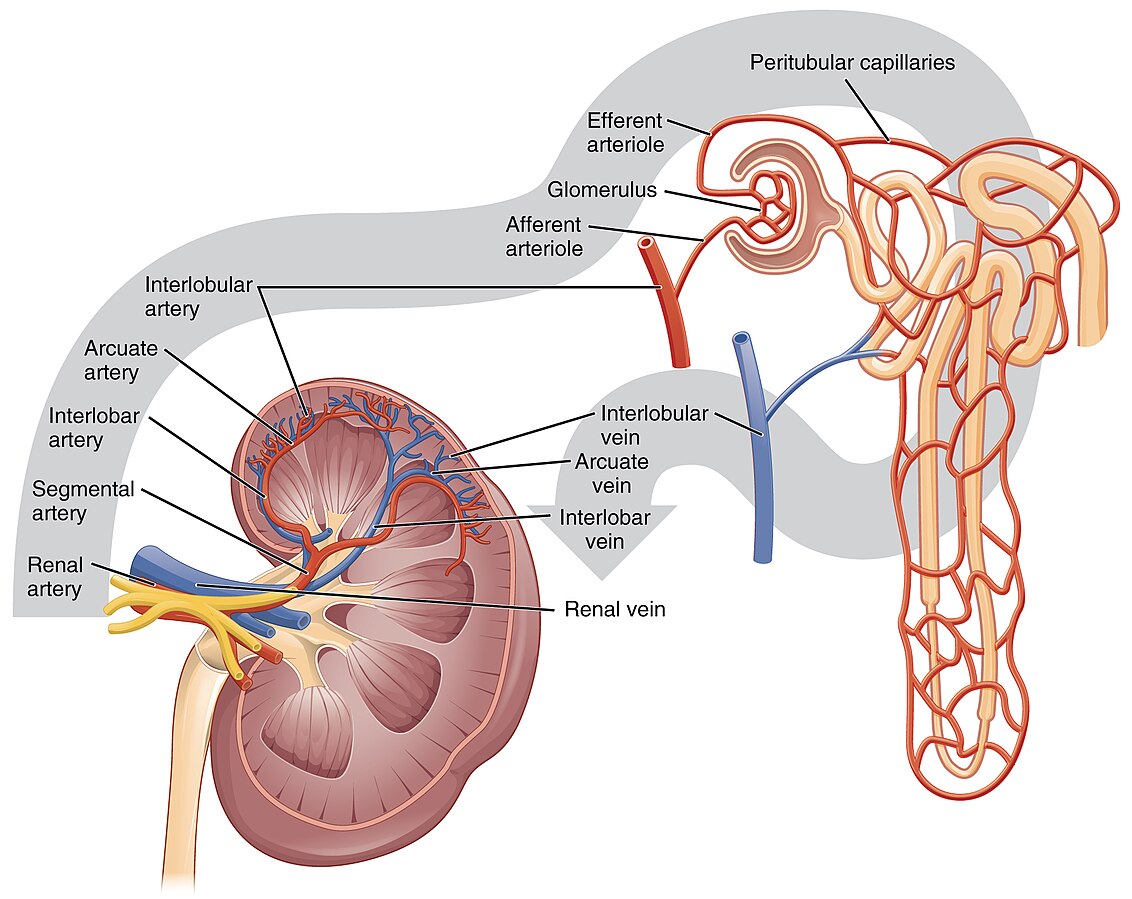
The nephron is the functional unit of the kidney and filters the blood, removes wastes, and balances fluid and electrolyte levels. A nephron has two parts called a renal corpuscle and a renal tubule. The renal corpuscle consists of a cluster of high-pressure capillaries called the glomerulus, surrounded by a glomerular capsule. An afferent arteriole leads into the renal corpuscle, and an efferent arteriole leaves the renal corpuscle. See Figure 8.5[6] for an illustration of blood flow through the nephron. The capillaries in the glomerulus initially filter the blood based on particle size.
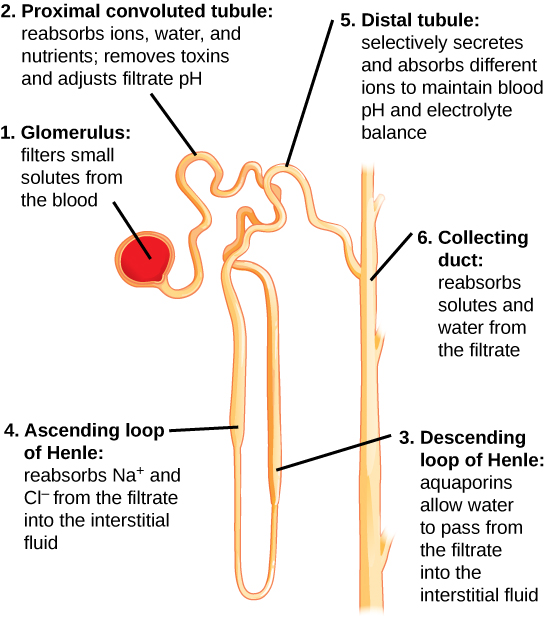
After blood is filtered by the glomerulus, it continues to pass through the renal tubule. Very thin and a little over an inch long, the renal tubule has three segments that the filtrate flows through called the proximal convoluted tubule, the loop of the nephron (referred to as the “loop of Henle”), and the distal convoluted tubule. Different portions of the renal tubule have different permeabilities for solutes and water, and efferent arterioles recover most of the water and electrolytes and return them back into the circulation. The remaining wastes pass as urine from the nephrons into collecting ducts and eventually into the ureters for elimination from the body. Within the renal tubule sodium, chloride, water, calcium, bicarbonate, glucose, protein, and blood components are typically reabsorbed whereas potassium, phosphorus, hydrogen, creatinine, and urea are typically excreted.
Ureters
As urine is formed, it drains into the calyces of the kidney, which merge to form the funnel-shaped renal pelvis in the hilum of each kidney. The hilum narrows to become the ureter of each kidney. As urine passes through the ureter, it does not passively drain into the bladder but rather is propelled by waves of peristalsis. The ureters are approximately 30 cm long. The muscular layer of the ureter creates the peristaltic contractions to move the urine into the bladder without the aid of gravity.
Bladder
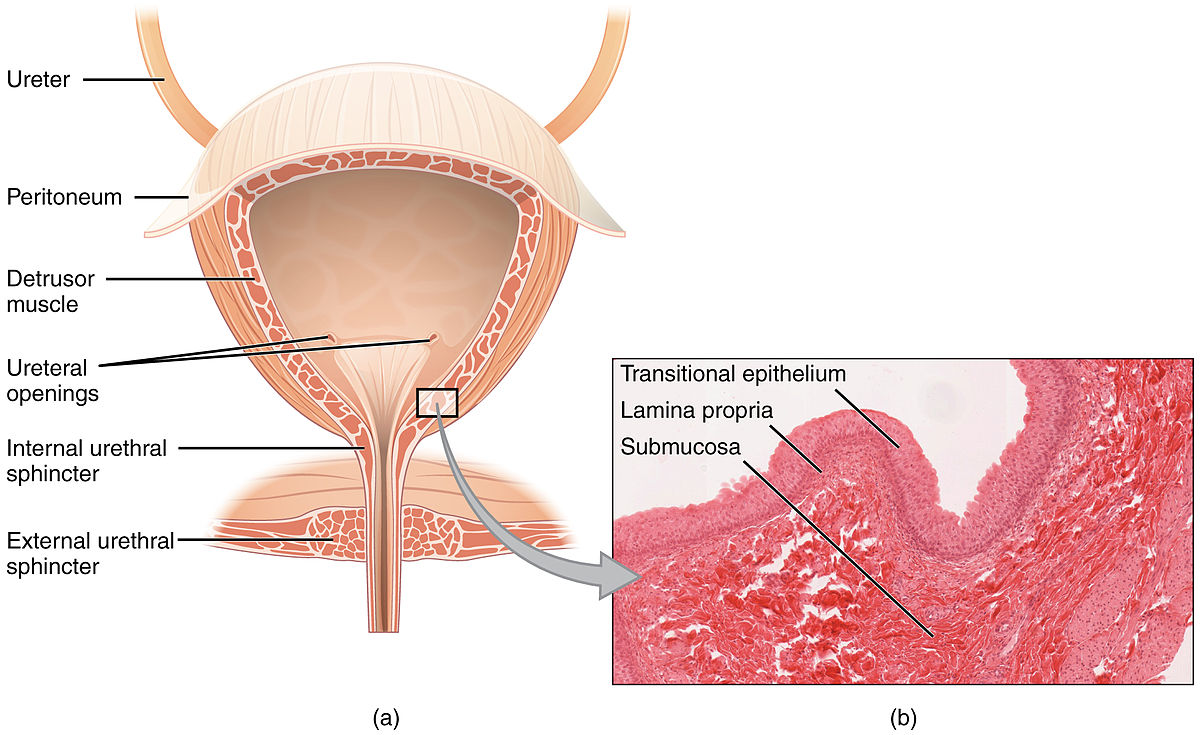
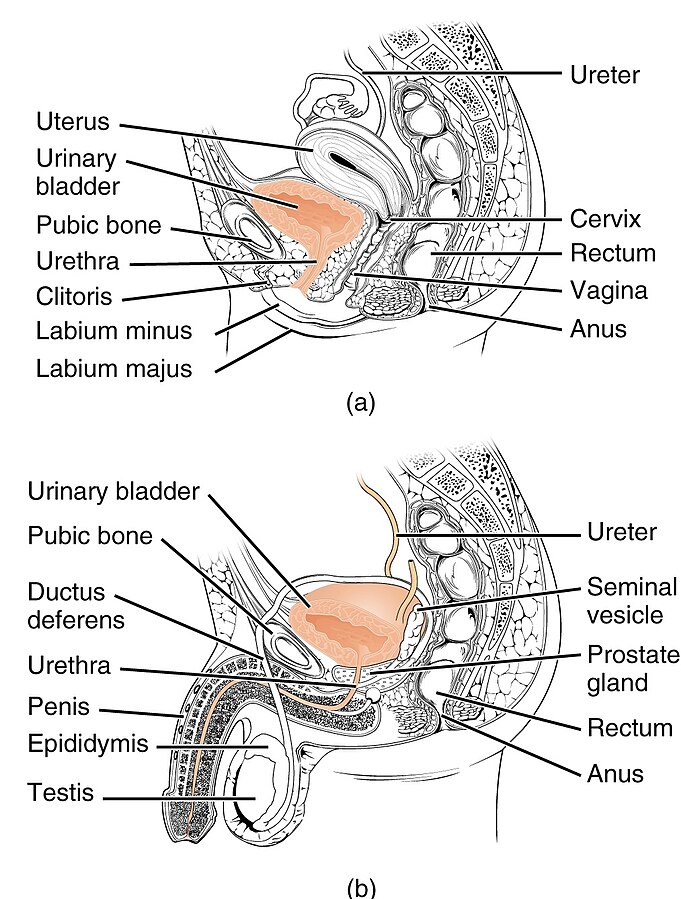
The bladder collects urine from both ureters. View Figure 8.6[7] to see a cross-section of the bladder. The bladder lies anterior to the uterus in females, posterior to the pubic bone, and anterior to the rectum. During late pregnancy, its capacity is reduced due to compression by the enlarging uterus, resulting in increased frequency of urination. In males, the anatomy is similar, minus the uterus, with the addition of the prostate inferior to the bladder. The bladder is partially retroperitoneal (outside the peritoneal cavity) with its peritoneal-covered “dome” projecting into the abdomen when the bladder becomes distended (stretched out) with urine.
Urethra
The urethra transports urine from the bladder to the outside of the body during urination. The urethra is the only urologic organ that is significantly different between males and females; all other urine transport structures are identical. In females, the urethra is shorter and closer to the rectum, which causes increased risk for urinary tract infections. See Figure 8.7[8] for a comparison of the female and male urethra.
Physiology
Filtration, Reabsorption, and Secretion
The kidneys filter all the blood in your body every 30 minutes and create urine. They remove waste products and excess fluid and also regulate electrolytes and hormones that control blood pressure, stimulate production of red blood cells, and activate vitamin D to keep bones healthy.[9]
Blood enters the kidneys via the renal arteries and is filtered by nephrons, where many functions take place. Three principal functions of the nephron are filtration, reabsorption, and secretion. Secondary functions of the nephron include controlling blood pressure (via the production of renin), producing red blood cells (via the hormone erythropoietin), and vitamin D activation so calcium can be absorbed via the gastrointestinal tract.[10]
To produce urine, nephrons and collecting ducts carry out three basic functions: glomerular filtration, tubular reabsorption, and tubular secretion. The initial filtering of the blood takes place in the glomerulus, a cluster of capillaries surrounded by the glomerular capsule within the nephron. The renal tubule receives this filtered fluid, called glomerular filtrate, and electrolytes and water are reabsorbed in different parts of the renal tubule and returned to circulation. The final end product of the filtered fluid is urine.[11] These processes are discussed in more detail in the following subsections.
Filtration
The first step in urine production is glomerular filtration. In this process, water and most of the solutes in the blood pass through the wall of glomerular capillaries into the glomerular capsule and then into the renal tubule. This process filters the blood and creates a filtrate that does not contain blood cells or large proteins, referred to as glomerular filtrate.
The volume of filtrate formed by both kidneys per minute is called the glomerular filtration rate (GFR). GFR is used to assess how well the kidneys are functioning. The heart pumps about five liters of blood per minute when a person is resting, and approximately 20 percent of this (i.e., one liter) enters the kidneys to be filtered per minute. On average, this results in the production of about 115 mL/min of filtrate produced by the nephrons. However, 99 percent of this filtrate is returned to the circulation by reabsorption so that only about 1–2 liters of urine are produced per day.
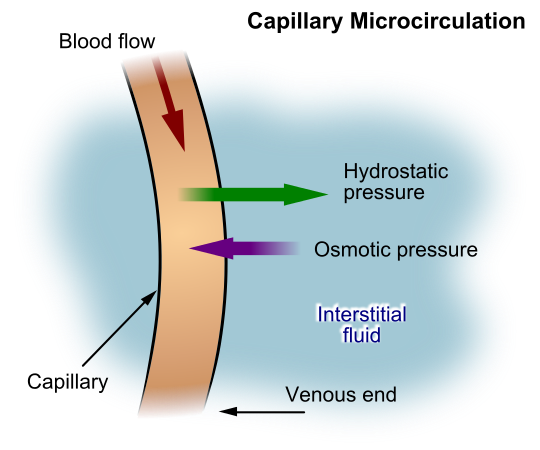
GFR is influenced by hydrostatic pressure, osmotic pressure, and oncotic pressures. Hydrostatic pressure refers to the pressure produced by a fluid against a surface. Glomerular filtration occurs as hydrostatic pressure forces fluid and solutes through the semipermeable barrier of the glomerular capillary membrane. The movement of solutes out of the blood is limited by their size. Glomerular filtration occurs when glomerular capillary hydrostatic pressure exceeds the luminal hydrostatic pressure of glomerular capsule.
Another force, called osmotic pressure, also controls the movement of water. Osmosis refers to the movement of water across a semipermeable membrane that is impermeable to a solute. As long as the concentration of water differs on both sides, water will move in the direction of lower pressure until the osmotic pressure on both sides of the membrane is equal. For this reason, a proper concentration of solutes in the blood is important in maintaining osmotic pressure in the glomerulus, as well as systemically.
A third force, called oncotic pressure, is created by the protein content of the blood that helps hold water inside of capillaries. There are urinary system disorders in which too much protein passes through during filtration into the glomerular filtrate. This excess protein in the filtrate leads to a deficiency of circulating proteins in the blood. In turn, the presence of excess protein in the urine allows it to retain more water in the filtrate and results in an increase in urine volume. Because there is less circulating protein in the blood (principally albumin), the osmotic pressure of the blood also falls. Less osmotic pressure tips the balance towards hydrostatic pressure, which causes water to be pushed out of the capillaries. The net effect is that water is lost from the circulation into interstitial tissues and cells. This “plumps up” the tissues and cells, a condition called edema.
See Figure 8.8[12] for an illustration of hydrostatic pressure and osmotic pressure in a capillary.
Tubular Reabsorption and Secretion
After glomerular filtration, the filtrate continues to undergo modification through secretion and reabsorption in the renal tubules before urine is produced and collected in the collecting ducts. During this process, some substances are reabsorbed, whereas others are secreted. In fact, 99 percent of the water and most of the solutes that were filtered out during glomerular filtration are reabsorbed in the tubules. A blood vessel runs alongside the tubule. As the filtered fluid moves along the tubule, a blood vessel reabsorbs almost all of the water, along with minerals and nutrients the body needs, and returns them to the body via the renal vein. The remaining fluid and wastes in the tubule become urine.
See Figure 8.9[13] for an illustration of tubular reabsorption and secretion. The glomerulus (1) filters small solutes from the blood. The proximal tubule (2) reabsorbs 60-70% of the sodium and water back into the bloodstream. From the proximal tubule, the filtrate flows into the descending loop of Henle (3) and then into the ascending loop of Henle (4). Another 20-25% of sodium is reabsorbed in the ascending loop of Henle. Filtrate then enters the distal tubule (5), where sodium is actively filtered in exchange for potassium or hydrogen ions to maintain blood pH and electrolyte balance, a process regulated by the hormone aldosterone. The collecting duct (6) is the final pathway where antidiuretic hormone (ADH) acts to further reabsorb water and solutes back into the bloodstream, thereby preventing it from being eliminated in urine.
Urination
To urinate means passing urine out of the bladder, also referred as void or micturate. A healthy adult with normal functioning kidneys produces an average of 800-2,000 mL of urine per day, depending on their fluid intake and other physiological processes. The adult bladder typically holds about 360-480 mL of urine.
Urination is regulated by the internal and external urinary sphincters, circular muscles constricting an orifice. As the bladder fills and reaches about 150 mL (5 ounces), it sends signals to the brain to create an urge to urinate. The internal and external urinary sphincters work together to close off the urethra to keep urine in the bladder. The external urinary sphincter is under voluntary control and remains closed until the brain sends a signal it is time to urinate. As the bladder fills, subsequent urges become harder to ignore. If voluntary voiding does not occur and the bladder overfills, voluntary control fails, resulting in urinary incontinence.
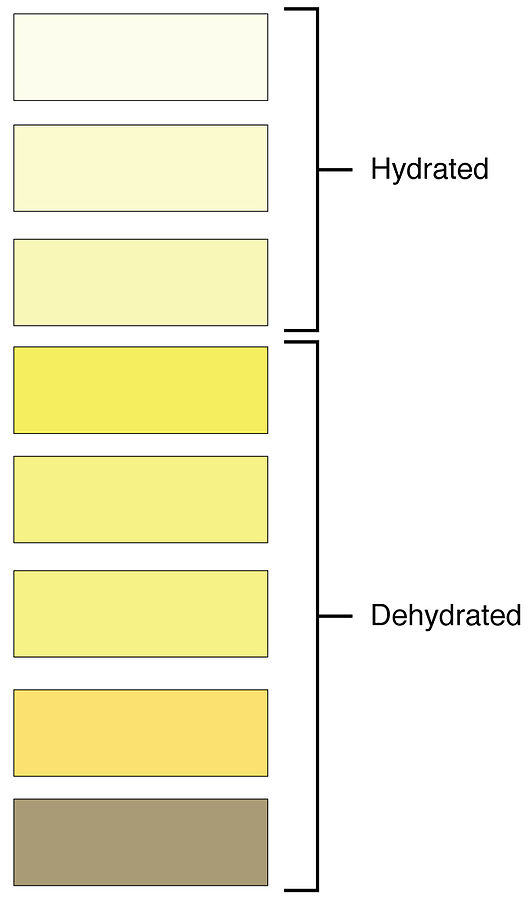
Frequency of urination depends on how quickly the kidneys produce urine and how much urine a person’s bladder can comfortably hold. Normal urine is typically clear or pale to light yellow in color and not foul-smelling. However, some foods or medications may change the smell or color of urine.[14]
In infants, the reflex to urinate is active, but as toddlers mature, they learn how to override the reflex and control the external sphincter, thus delaying voiding until it is appropriate to do so (commonly referred to as “potty training”).
Urine
Urine volume varies considerably by individual, based on several factors such as fluid intake, perspiration, and disorders affecting the urinary system. The normal range of urine output for adults is one to two liters per day. The kidneys must produce a minimum urine volume of about 500 mL/day to adequately rid the body of wastes. Urine output below this level can be caused by severe dehydration or kidney disease.
Urine color and odor are affected by many conditions and even the food a person has eaten. For example, a urinary tract infection or kidney stone may cause bleeding, resulting in pink or even bright red urine. Dehydration produces darker, concentrated urine. See Figure 8.10[15] for an illustration of the color of urine based on the client’s hydration status. Additionally, about one in five people detect a distinctive odor in their urine after consuming asparagus; other foods such as onions, garlic, and fish can impart their own aromas. These food-caused odors are harmless.
Urea
Urea nitrogen is a waste product made when the liver breaks down protein into amino acids, and then deamination converts the amino acids into ammonia, urea, or uric acid. Urea is transported in the blood, filtered out by the kidneys, and eliminated from the body in urine. Urine primarily contains urea with small amounts of ammonia and uric acid. When damage occurs to the nephrons, urea is not filtered out as efficiently, and a buildup of urea in the blood can occur. For this reason, a diagnostic test called blood urea nitrogen (BUN) provides important information about kidney function.
Most of the ammonia produced from the breakdown of protein in the body is converted into urea by the liver, so the odor of ammonia is rarely detected in fresh urine.
Diuretics
A diuretic is a substance that increases urine production. Three common beverages contain diuretic compounds: coffee, tea, and alcohol. The caffeine in coffee and tea works by promoting vasodilation in the nephron, which increases GFR. Alcohol increases GFR by inhibiting ADH release from the posterior pituitary, resulting in less water recovery by the collecting duct. Medications called diuretics are prescribed to reduce blood volume and, thereby, reduce edema.
Acid-Base Imbalances Resulting From Nephron Damage
Several diseases and disorders can damage the kidneys and the nephrons. When nephrons are damaged, their ability to filter, reabsorb, and secrete substances is affected.
The kidneys and the lungs work together to balance acids and bases in the body. If an acid-base imbalance occurs due a respiratory disorder, the kidneys compensate by adjusting bicarbonate level of the blood (HCO3). HCO3 is a base that makes the blood more alkaline. As the kidneys sense an alteration in pH, they begin to retain or excrete HCO3, depending on what is needed. If the pH becomes acidic, the kidneys retain HCO3 to increase the amount of bases present in the blood to increase the pH. Conversely, if the pH becomes alkalotic, the kidneys excrete more HCO3, causing the pH to decrease.[16]
Metabolic Acidosis
Under normal conditions, the kidneys work to excrete acids through urine and neutralize excess acids by increasing bicarbonate (HCO3) reabsorption from the urine to maintain a normal pH. When the kidneys are not able to perform this buffering function to the level required to excrete and neutralize the excess acid, metabolic acidosis results. Metabolic acidosis is diagnosed by arterial blood gas (ABG) results indicating a pH level below 7.35 and an HCO3 level below 22.[17]
A common cause of metabolic acidosis is diabetic ketoacidosis, where acids called ketones build up in the blood. Another common cause of metabolic acidosis is lactic acidosis, which can be caused by impaired tissue oxygenation. Metabolic acidosis can also be caused from renal disease that causes decreased acid elimination.[18]
Nurses may first suspect that a client has metabolic acidosis due to rapid breathing that occurs as the lungs try to remove excess carbon dioxide in an attempt to resolve the acidosis. Other symptoms of metabolic acidosis include confusion, decreased level of consciousness, hypotension, and electrolyte disturbances that can progress to circulatory collapse and death if not treated promptly. It is important to promptly notify the provider of suspected metabolic acidosis so that an ABG can be drawn, and treatment prescribed based on the cause.[19]
Metabolic Alkalosis
Metabolic alkalosis occurs when there is too much bicarbonate (HCO3) or an excessive loss of acid (H+ ions). Metabolic alkalosis is defined by ABG results indicating a pH above 7.45 and an HCO3 level above 26. One cause of metabolic alkalosis is excessive urine loss (due to diuretics or excessive mineralocorticoids) due to loss of hydrogen ions in the urine.[20] Prolonged vomiting and extensive nasogastric tube suctioning may also result in conditions of metabolic alkalosis.
A nurse may first suspect that a client has metabolic alkalosis due to a decreased respiratory rate (as the lungs try to retain additional CO2 to increase the acidity of the blood and resolve the alkalosis). The client may also be confused due to the altered pH level. The nurse should report signs of suspected metabolic alkalosis because uncorrected metabolic alkalosis can result in hypotension and cardiac dysfunction. Treatment is prescribed based on the ABG results and the suspected cause.[21]
Review information about acid-base imbalance in the “Acid-Base Balance” section of the “Fluids & Electrolytes” chapter of Open RN Nursing Fundamentals, 2e.
Other Terms Related to Urine and Urination
Terms commonly used to document conditions related to the urinary system are as follows:
- Anuria: Absence of urine output, typically found during kidney failure, defined as less than 50 mL of urine over a 24-hour period.
- Diuresis: Increased production of urine.
- Dysuria: Painful or difficult urination.
- Enuresis: Involuntary urination, especially by children.
- Frequency: The need to urinate several times during the day or night in normal or less-than-normal volumes. It may be accompanied by a feeling of urgency.[22]
- Hematuria: Blood in the urine, either visualized or found during microscopic analysis.
- Incontinence: Loss of bladder control.
- Oliguria: Decreased urine output; defined as less than 500 mL of urine in adults in a 24-hour period.
- Nocturia: The need to get up at night on a regular basis to urinate. Nocturia often causes sleep deprivation that affects a person’s quality of life.[23]
- Polyuria: Greater than 2.5 liters of urine output over 24 hours; also referred to as diuresis.[24] New polyuria should be reported to the health care provider because it can be a sign of many medical conditions.
- Pruritus: Itchy skin; a common symptom of kidney failure.
- Pyuria: White blood cells in a urine sample indicating infection. In severe infections, pus may be visible in the urine.[25] See Figure 8.11[26] for an image of pyuria.
- Urgency: A sensation of an urgent need to void.[27] Urgency can cause urge incontinence if the client is not able to reach the bathroom quickly.

- National Institute of Diabetes and Digestive and Kidney Diseases. (2020). The urinary tract & how it works. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works ↵
- “Urinary_System_(Male).png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “2608_Kidney_Position_in_Abdomen.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “2610_The_Kidney.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “2612_Blood_Flow_in_the_Kidneys.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “2611_Blood_Flow_in_the_Nephron.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- "2605_The_Bladder.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “Female_and_Male_Urethra.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Centers for Disease Control and Prevention. (2022). Chronic kidney disease basics. https://www.cdc.gov/kidney-disease/about/ ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020). The urinary tract & how it works. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works ↵
- Colorado Community College System (CCCOnline). (n.d.). Anatomy & Physiology. https://pressbooks.ccconline.org/bio106/ ↵
- “Capillary_microcirculation.jpg” by Kes47 is in the Public Domain ↵
- “Figure 41 03 04.jpg” by CNX OpenStax is licensed under CC BY 4.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020). The urinary tract & how it works. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works ↵
- "2601_Urine_Color_Chart.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Nursing fundamentals 2E. Open RN | WisTech Open. https://wtcs.pressbooks.pub/nursingfundamentals/ ↵
- Maddukuri, G. (2021). Urinary frequency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/symptoms-of-genitourinary-disorders/urinary-frequency ↵
- Leslie, S. W., Sajjad, H., & Singh, S. (2024). Nocturia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK518987/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. (2021). Urination - excessive amount. https://medlineplus.gov/ency/article/003146.htm ↵
- Cherney, K. (2018). Everything you should know about pyuria. Healthline. https://www.healthline.com/health/pyuria ↵
- “Pyuria2011.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- Maddukuri, G. (2021). Urinary frequency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/symptoms-of-genitourinary-disorders/urinary-frequency ↵
- RegisteredNurseRN. (2017, May 4). Kidney and nephron anatomy structure function | Renal function system [Video]. YouTube. All rights reserved. Reused with permission. https://www.youtube.com/watch?v=0qZxw0Nd1lI ↵
- Bozeman Science. (2017, February 13). The urinary system [Video]. YouTube. All rights reserved. https://youtu.be/H2VkW9L5QSU ↵
System consists of the kidneys, ureters, bladder, and urethra.
An organ that filters waste from the blood and produces urine.
The functional unit of the kidney and filters the blood, removes wastes, and balances fluid and electrolyte levels.
A cluster of high-pressure capillaries.
The duct by which urine passes from the kidney to the bladder.
Hollow organ that acts as a reservoir for urine.
Stretched out.
Transports urine from the bladder to the outside of the body during urination.
The first step in urine production.
The volume of filtrate formed by both kidneys per minute.
The pressure produced by a fluid against a surface
The movement of water across a semipermeable membrane that is impermeable to a solute
Colloidal pressure created by the protein content of the blood; helps hold water inside of capillaries.
Excess fluid around the cells.
Passing urine, also referred as void or micturate.
Circular muscles constricting an orifice.
Occurs when the bladder overfills and voluntary control fails.
A waste product made when the liver breaks down protein into amino acids, and then deamination converts the amino acids into ammonia, urea, or uric acid.
Process by which amino acids are broken into ammonia, urea, or uric acid.
A substance that increases urine production.
A pH level below 7.35 and an HCO3 level below 22.
A pH above 7.45 and an HCO3 level above 26.
Absence of urine output, typically found during kidney failure, defined as less than 50 mL of urine over a 24-hour period.
Increased production of urine.
Painful or difficult urination.
Involuntary urination, especially by children.
The need to urinate several times during the day or night in normal or less-than-normal volumes.
Blood in urine.
Loss of bladder control.
Decreased urine output, defined as less than 500 mL of urine in adults in a 24-hour period.
The need to get up at night on a regular basis to urinate.
Excessive urination.
Itching.
White blood cells in a urine sample indicating infection. In severe infections, pus may be visible in the urine
A sensation of an urgent need to void.

