7.6 Thyroid Disorders
The thyroid gland is a butterfly-shaped organ located in the front of the neck and plays a vital role in regulating various metabolic processes in the body by producing and releasing thyroid hormones. When the thyroid gland does not function correctly, it can lead to a range of thyroid disorders, with the most common being hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid). These disorders can result in a variety of symptoms and health complications, affecting energy levels, weight, vital signs, and overall well-being.[1]
Hypothyroidism
Hypothyroidism is a medical condition characterized by an underactive thyroid gland that causes reduced production of thyroid hormones. When the thyroid gland fails to produce sufficient levels of thyroxine (T4) and triiodothyronine (T3), the body’s metabolic rate decreases. Goiter, a swelling or nodularity of the thyroid, is a sign of both hypothyroidism and hyperthyroidism. See Figure 7.15[2] for an image of a goiter.

A Closer Look…Myxedema Coma
Myxedema coma is a severe form of hypothyroidism. It is a rare condition that requires immediate medical attention. Myxedema means “swelling of the skin and underlying tissues.” With extremely low levels of thyroid hormones, multisystem organ failure can develop. Hypothermia is a hallmark sign of myxedema coma. Other classic signs and symptoms of myxedema coma include severe bradycardia, hypotension, and impaired cardiac contractility that can result in cardiac failure. Breathing can become shallow, resulting in hypoxia and hypercapnia. Impaired cognitive function with decreased levels of consciousness and extreme confusion can progress to complete lack of responsiveness or coma. To prevent myxedema coma, it is crucial for individuals diagnosed with hypothyroidism to adhere to their prescribed treatment regimen by taking thyroid hormone replacement medication as directed and attending regular follow-up appointments with their health care provider to monitor their condition with lab work.[3],[4]
Pathophysiology
Hypothyroidism can be caused by a variety of factors, including autoimmune disease, thyroid surgery, radiation therapy, medications, iodine deficiency, or congenital thyroid disease. The most common cause of hypothyroidism is an autoimmune disease called Hashimoto’s thyroiditis, a condition in which the immune system mistakenly attacks the thyroid gland, resulting in inflammation and damage.[5]
Assessment of Hypothyroidism
Common signs and symptoms of untreated or inadequately controlled hypothyroidism can be viewed in the following Table 7.6a.
Table 7.6a. Common Manifestations of Hypothyroidism[6]
| Body System | Common Manifestations |
|---|---|
| General | Fatigue and weakness, cold intolerance, weight gain, hoarseness associated with goiter, or myxedema (generalized edema) |
| Cardiovascular | Bradycardia and hypotension |
| Respiratory | Slow, shallow breathing |
| Gastrointestinal | Constipation, abdominal bloating and pain, or anorexia |
| Musculoskeletal | Muscle weakness and aches, joint pain and stiffness, or muscle cramps |
| Neurological | Cognitive impairment (i.e., memory problems, poor concentration), depression, slow mental processing, or paresthesia (tingling or numbness in extremities) |
| Integumentary | Dry, pale, cool, itchy skin; dry, coarse, brittle hair or hair loss; or thinning, brittle, ridged nails |
| Reproductive | Menstrual irregularities (heavier or more frequent periods), infertility (in some cases), or low libido (decreased sexual desire) |
Diagnostic Testing
Diagnostic testing for hypothyroidism assesses the underactivity of the thyroid gland. It typically involves measuring the blood levels of thyroid hormones, especially T3 (triiodothyronine), T4 (thyroxine), and TSH (thyroid-stimulating hormone)[7],[8]:
- Thyroid-Stimulating Hormone (TSH): TSH is produced by the pituitary gland. Recall that TSH is part of a negative feedback loop for regulating thyroid hormones by the hypothalamus and pituitary. In hypothyroidism, where the thyroid gland is underactive and not producing enough thyroid hormones, the pituitary gland increases its production of TSH to stimulate the thyroid gland to produce more thyroid hormones. Therefore, in hypothyroidism, the TSH level is typically elevated.[9]
- Thyroxine (T4): T4 is produced and secreted by the thyroid gland. T4 is a prohormone and is relatively inactive on its own. However, it serves as a precursor to the more active thyroid hormone triiodothyronine (T3). Low T4 levels indicate hypothyroidism.[10]
- Triiodothyronine (T3): T3 is the active form of thyroid hormone. It directly impacts the body’s metabolic rate by affecting the function of cells throughout the body. T3 helps regulate how the body uses energy, including the consumption of oxygen and the burning of calories. This, in turn, impacts body temperature, heart rate, and the rate of chemical reactions in the body.[11]
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing diagnoses for clients with hypothyroidism guide nursing care and address the specific needs of these individuals.
Common nursing diagnoses include the following:
- Fatigue
- Imbalanced Nutrition
- Impaired Thermoregulation
- Constipation
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
- The client will verbalize an understanding of energy conservation techniques.
- The client will achieve and maintain a stable, healthy body weight within the recommended range.
- The client will verbalize an understanding of strategies to prevent constipation, such as increased fiber and physical activity.
Interventions for Hypothyroidism
Medical Interventions
Medical interventions for hypothyroidism focus on hormone replacement therapy, hormone level monitoring, and dietary modifications. Adherence to prescribed medical therapy and appropriate monitoring are critical for managing this chronic disease.
Medication Therapy
Levothyroxine is a synthetic T4 hormone and is the classic treatment for hypothyroidism. It is usually taken orally as a daily medication. The goal of treatment is to achieve and maintain a stable TSH level within the normal range, indicating adequate thyroid hormone replacement.
Review additional information about thyroid replacement medications in the “Thyroid Medications” section of the “Endocrine” chapter of Open RN Nursing Pharmacology, 2e.
TSH Monitoring
After beginning thyroid hormone replacement therapy, TSH levels must be routinely monitored to assess thyroid function and ensure thyroid hormones are within the target range. Adjustments to a client’s medication dosage may be necessary based on the test results and the client’s clinical response to the medication.
Dietary Modifications
Maintaining a well-balanced diet that includes iodine (a crucial component of thyroid hormones) is important. Clients may benefit from dietary modifications to prevent constipation, such as increased fluids, fiber, and physical activity. It may also be helpful to avoid excessive consumption of foods that can interfere with thyroid function such as cruciferous vegetables, soy products, peaches, and strawberries.[12]
Nursing Interventions
Nursing interventions for hypothyroidism focus on medication management and symptom management to promote client comfort.
Medication Management
Nurses teach the importance of taking thyroid medication at the same time each day, preferably on an empty stomach, to maximize absorption. They explain that levothyroxine is prescribed at a low dose and then titrated to achieve therapeutic blood levels of TSH, requiring repeated blood draws. Nurses teach clients to avoid taking thyroid medication with certain foods, beverages, and supplements that can interfere with absorption (e.g., calcium supplements, iron, and soy) and emphasize the importance of not changing the brand of thyroid medication without consulting their health care provider.
Nurses are aware that clients with hypothyroidism must use sedatives and opioids with caution because of the increased effects of sedation and respiratory depression effects of these medications.
Symptom Management
Nurses teach clients how to manage symptoms, such as fatigue, weight gain, and cold intolerance, until thyroid hormone levels are normalized. They encourage the client to maintain a nutritious diet and engage in regular physical activity, but also teach energy conservation techniques to combat fatigue. Nurses discuss the client’s comfort level with temperature regulation, especially regarding cold intolerance, and encourage the use of appropriate clothing and heating devices to stay warm. Review energy management strategies in the “Nursing Interventions” subsection of “Iron-Deficiency Anemia” in the “Hematological Alterations” chapter.
Hyperthyroidism
Hyperthyroidism is characterized by the excess secretion of thyroxine (T4) and triiodothyronine (T3) from the thyroid gland. Hyperthyroidism can be a chronic or temporary condition, depending upon the underlying cause.
Pathophysiology
Common causes of hyperthyroidism include Graves’ disease (an autoimmune disorder), toxic nodular goiter, and thyroiditis. Graves' disease is typically a long-lasting or permanent condition resulting from autoimmune destruction of the thyroid gland, whereas other forms of hyperthyroidism, such as thyroiditis, can be temporary and resolve on their own.
Recall the negative feedback loop used to regulate the secretion of thyroid hormones. In hyperthyroidism there is a failure of negative feedback control mechanisms. The thyroid gland becomes overactive, producing excessive levels of thyroid hormones regardless of the body’s actual need.
Thyroid storm is a severe state of hyperthyroidism that is a life-threatening medical condition. It occurs when hyperthyroidism is untreated, poorly controlled, or when the client is under severe physical or emotional stress, or if antithyroid medication is abruptly stopped. It can also occur during surgery when the thyroid is manipulated. Thyroid storm is most commonly associated with Graves’ disease, which causes the thyroid gland to produce excessive amounts of thyroid hormones.[13] Review additional information about thyroid storm in the following box.
A Closer Look at a Thyroid Storm[14],[15]
Thyroid storm is a severe manifestation of hyperthyroidism in which excessive release of thyroid hormones causes a range of life-threatening symptoms.
Manifestations of thyroid storm are as follows:
- Fever: Clients with thyroid storm often have hyperthermia, an extremely high body temperature.
- Tachycardia: The heart rate becomes excessively fast, which can strain the cardiovascular system.
- Hypertension: Blood pressure may rise to dangerous levels, putting significant stress on the heart and blood vessels.
Thyroid storm is a medical emergency that requires immediate hospitalization and intensive medical management. Treatment typically includes medications to control the production and effects of thyroid hormones, as well as supportive care to manage symptoms and complications. Prompt recognition and treatment of thyroid storm are crucial to improving the chances of a successful outcome for individuals experiencing thyroid storm.
Assessment of Hyperthyroidism
Common signs and symptoms of hyperthyroidism are summarized in Table 7.6b.
Table 7.6b. Common Manifestations of Hyperthyroidism[16]
| Body System | Clinical Manifestations and Findings |
|---|---|
| Cardiovascular | Tachycardia, palpitations, hypertension, chest pain or angina, and arrhythmias |
| Nervous | Nervousness and anxiety, restlessness and irritability, tremors, heat intolerance, excessive sweating, insomnia and sleep disturbances, and difficulty concentrating or memory problems |
| Gastrointestinal | Increased appetite and weight loss, frequent bowel movements and diarrhea, nausea and vomiting, and hepatomegaly |
| Musculoskeletal | Muscle weakness, fatigue, and osteoporosis (bone density loss) |
| Endocrine | Goiter (enlargement of the thyroid gland) |
| Dermatological | Warm, moist skin; fine, soft hair and hair loss; and onycholysis (separation of fingernails from the nail bed) |
| Reproductive | Menstrual irregularities and amenorrhea (absence of menstrual periods) in some female clients |
| Ocular | Eye-related symptoms such as double vision, photophobia, and exophthalmos (bulging eyes) (See Figure 7.16[17] for an image of exophthalmos.) |
| Respiratory | Shortness of breath and tachypnea (due to increased oxygen demand) |
| Psychological | Emotional lability (rapid shifts in mood) |

Figure 7.16 Exophthalmos
Diagnostic Testing
Diagnostic testing for hyperthyroidism includes measuring blood levels of T3 (triiodothyronine) and T4 (thyroxine). Excessive T3 and T4 levels cause the symptoms and metabolic changes seen in hyperthyroidism. In response, the TSH (thyroid-stimulating hormone) level is typically decreased as the pituitary decreases stimulation of the thyroid to regulate T3 and T4 levels. Review information about these diagnostic tests under the “Diagnostic Testing” subsection for “Hypothyroidism.”
Nursing Diagnoses
Nursing diagnoses for clients with hyperthyroidism can help guide nursing care and address the specific needs of these individuals.
Common nursing diagnoses include the following:
- Ineffective Thermoregulation
- Anxiety
- Imbalanced Nutrition
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
- The client will demonstrate effective self-regulation of body temperature.
- The client will engage in relaxation techniques and stress-reduction activities.
- The client will achieve and maintain a stable weight.
Interventions for Hyperthyroidism
Medical Interventions
Medical interventions for hyperthyroidism aim to control the overproduction of thyroid hormones and manage the associated symptoms. Medication therapy, radioactive iodine, thyroidectomy, and radiofrequency ablation are common treatments for hyperthyroidism. The choice of treatment depends on the underlying cause of hyperthyroidism, the severity of the condition, and the client’s individual health factors.
Medication Therapy
Common medications used to treat hyperthyroidism and/or associated symptoms include antithyroid medications and beta-blockers.
- Antithyroid Medications: These medications work by blocking the production of thyroid hormones in the thyroid gland. They are often used to temporarily control hyperthyroidism, especially in Graves’ disease. Examples include methimazole and propylthiouracil (PTU).[18]
- Beta-Blockers: Beta-blockers are prescribed to manage the symptoms of hyperthyroidism, such as rapid heartbeat, tremors, and anxiety. They do not affect thyroid hormone levels but help alleviate some of the uncomfortable symptoms. Examples include propranolol and atenolol.[19]
Review additional information about these medication classes in the “Thyroid Medications” section of the “Endocrine” chapter in Open RN Nursing Pharmacology, 2e.
Radioactive Iodine (RAI) Therapy
Radioactive iodine (RAI) therapy is a common treatment for hyperthyroidism in conditions like Graves’ disease. It involves the oral ingestion of a radioactive form of iodine, which is selectively taken up by the overactive thyroid cells. The RAI gradually shrinks the thyroid and reduces hormone production. However, this treatment can result in hypothyroidism, which may require lifelong thyroid hormone replacement therapy.[20] Clients who undergo radioactive iodine therapy will give off radiation for some time after treatment. They are taught radiation precautions, including how to protect others through social distancing, and to avoid contact with anyone who is pregnant or trying to get pregnant.[21]
Thyroidectomy
In some cases, surgical removal of part or all of the thyroid gland may be necessary, particularly when other treatments are not suitable or effective. A total thyroidectomy removes the entire thyroid gland, while a subtotal thyroidectomy removes a portion of the thyroid gland. Clients who undergo thyroid surgery require lifelong thyroid hormone replacement because this surgery typically results in hypothyroidism.[22] Although a thyroidectomy is a common surgical procedure, there are a number of complications that can occur. See Table 7.6c for an overview of potential postoperative complications after a thyroidectomy.
Table 7.6c. Potential Complications After a Thyroidectomy[23]
| Potential Complication | Cause | Signs and Symptoms | Treatment/Nursing Interventions |
|---|---|---|---|
| Airway compromise | Can occur due to hemorrhage, swelling, or tetany (involuntary contraction or spasm of muscles, associated with low calcium levels)
|
Difficulty breathing, neck swelling, stridor, low oxygen levels, difficulty swallowing, or drooling | Client may have to return to operating room in case of hemorrhage
Ensure tracheostomy tray is nearby Monitor surgical dressing for excessive bleeding (note that blood may pool to back of dressing) Keep neck in neutral position to prevent stress on suture line Monitor respiratory status Provide humidified air if possible to reduce tissue swelling |
| Hypoparathyroidism | Can occur due to unintended removal of or trauma to parathyroid glands during surgery | Low serum calcium levels, numbness, tingling, muscle cramping, Chvostek’s and Trousseau’s signs, changes in EKG readings, or seizures | Supplement with calcium and vitamin D
Monitor for signs and symptoms of low calcium Monitor levels of serum calcium Educate on food sources that are high in calcium and vitamin D |
| Laryngeal nerve injury | Superior and recurrent laryngeal nerves run through the thyroid and are at risk for injury during thyroid removal | Hoarse sounding voice, changes in the pitch of voice, or aspiration. May be transitory or permanent | Assess voice before and after surgery
Encourage resting of the voice Provide alternative means to communicate if necessary Monitor for signs of aspiration |
Radiofrequency Ablation
Radiofrequency ablation (RFA) is a minimally invasive procedure that uses radiofrequency energy to heat and destroy thyroid nodules or hyperactive tissue. This technique is typically employed for clients with toxic thyroid nodules or small areas of overactivity.[24]
Nursing Interventions
Nursing interventions for hyperthyroidism focus on medication management, nutritional support and hydration, and symptom management to promote client comfort.
Medication Compliance
Nurses administer antithyroid medications as prescribed and provide health teaching about the medication and potential side effects. Education is also provided regarding the importance of regular follow-up appointments and blood tests to monitor thyroid hormone levels.
Nutritional Support and Hydration
Nurses encourage a high-calorie diet to support the increased metabolic rate associated with hyperthyroidism. The client’s weight and nutritional status are monitored. Adequate fluid intake is also promoted because hyperthyroidism can lead to increased thirst and sweating.
Symptom Management
Clients with exophthalmos are typically prescribed eye drops to alleviate discomfort. Additional eye care may be required.
If the client is experiencing symptoms of anxiety and agitation as a result of elevated T3 and T4 levels, nurses encourage rest and a calm environment.
Evaluation
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the client’s expected outcomes to determine if they were met by the time frames indicated. For thyroid disorders, evaluation focuses on the normalization of thyroid panel results and the resolution of associated symptoms. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a client’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with others on the interprofessional team.
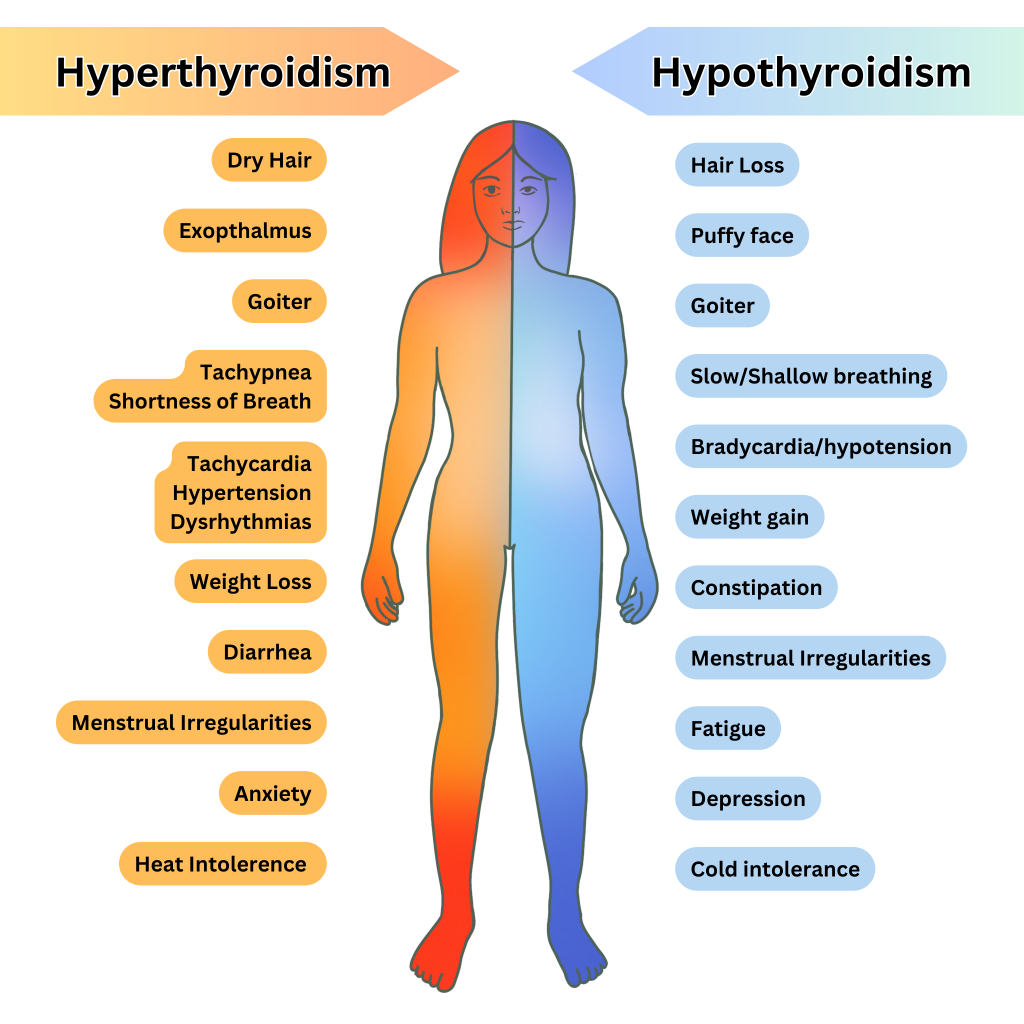
Comparison of Hypothyroidism and Hyperthyroidism
The clinical manifestations of hypothyroidism and hyperthyroidism can be easily remembered by recalling the opposite effects of “not enough” thyroid hormones versus “too much” thyroid hormones on various body systems. See Figure 7.17 [25] for an illustration comparing the manifestations of hypothyroidism and hyperthyroidism.
View a supplementary YouTube video[26] from Nurse Mike on hypothyroidism/hyperthyroidism: Hyperthyroidism vs. Hypothyroid RN LPN NCLEX.
![]() RN Recap: Hypothyroidism and Hyperthyroidism
RN Recap: Hypothyroidism and Hyperthyroidism
View a brief YouTube video overview of hypothyroidism and hyperthyroidism[27]:
- Ross, D. S. (2022). Thyroid hormone synthesis and physiology. UpToDate. www.uptodate.com ↵
- "Goiter.JPG" by Dr. J.S. Bhandari, India is licensed under CC BY-SA 3.0 ↵
- Ross, D. S. (2023). Treatment of primary hypothyroidism in adults. UpToDate. www.uptodate.com ↵
- Surks, M. I. (2022). Clinical manifestations of hypothyroidism. UpToDate. www.uptodate.com ↵
- Surks, M. I. (2022). Clinical manifestations of hypothyroidism. UpToDate. www.uptodate.com ↵
- Surks, M. I. (2022). Clinical manifestations of hypothyroidism. UpToDate. www.uptodate.com ↵
- National Institute of Diabetes and Digestive and Kidney Disease. (2017). Thyroid tests. National Institutes of Health. https://www.niddk.nih.gov/health-information/diagnostic-tests/thyroid ↵
- MedlinePlus [Internet]. (2023). Thyroid tests. https://medlineplus.gov/tendinitis.html ↵
- Ross, D. S. (2022). Diagnosis and screening for hypothyroidism in nonpregnant adults. UpToDate. www.uptodate.com ↵
- Ross, D. S. (2022). Diagnosis and screening for hypothyroidism in nonpregnant adults. UpToDate. www.uptodate.com ↵
- Ross, D. S. (2022). Diagnosis and screening for hypothyroidism in nonpregnant adults. UpToDate. www.uptodate.com ↵
- Ross, D. S. (2022). Diagnosis and screening for hypothyroidism in nonpregnant adults. UpToDate. www.uptodate.com ↵
- Ross, D. S. (2022). Overview of the clinical manifestations of hyperthyroidism in adults. UpToDate. www.uptodate.com ↵
- Ross, D. S. (2022). Overview of the clinical manifestations of hyperthyroidism in adults. UpToDate.www.uptodate.com ↵
- Ross, D. S. (2023). Thyroid storm. UpToDate. www.uptodate.com ↵
- Ross, D. S. (2022). Overview of the clinical manifestations of hyperthyroidism in adults. UpToDate. www.uptodate.com ↵
- "Proptosis_and_lid_retraction_from_Graves%27_Disease.jpg" by Jonathan Trobe, M.D. - University of Michigan Kellogg Eye Center is licensed under CC BY 3.0 ↵
- Ross, D. S. (2023). Patient education: Antithyroid drugs (Beyond the basics). UpToDate. www.uptodate.com ↵
- Ross, D. S. (2023). Beta blockers in the treatment of hyperthyroidism. UpToDate. www.uptodate.com ↵
- Ross, D. S., & Sugg, S. L. (2023). Surgical management of hyperthyroidism. UpToDate. www.uptodate.com ↵
- American Cancer Society. (2023). Radiation therapy safety. https://www.cancer.org/cancer/managing-cancer/treatment-types/radiation/safety.html ↵
- Ross, D. S., & Sugg, S. L. (2023). Surgical management of hyperthyroidism. UpToDate. www.uptodate.com ↵
- Biello, A., Kinberg, E. C., Menon, G., et al. (2024). Thyroidectomy. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563279/ ↵
- Ross, D. S., & Sugg, S. L. (2023). Surgical management of hyperthyroidism. UpToDate. www.uptodate.com ↵
- "Hyperthyroidism and Hypothyroidism" by Meredith Pomietlo is licensed by CC BY-NC 4.0. ↵
- Simple Nursing. (2019, August 21). Hyperthyroidism vs. hypothyroid RN LPN NCLEX [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=YyHM9xQyyas ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 7 - Hypothyroidism & hyperthyroidism [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/s3H4sc-3OFQ?si=l7aClnLjARPP8tTz ↵
A medical condition characterized by an underactive thyroid gland that causes reduced production of thyroid hormones.
A swelling or nodularity of the thyroid.
A severe form of hypothyroidism which can manifest with hypothermia, bradycardia, hypotention, impaired cardiac contractility resulting in cardiac failure.
A condition in which the immune system mistakenly attacks the thyroid gland, resulting in inflammation and damage.
Hormone which stimulates the thyroid gland to produce more thyroid hormones.
A prohormone which serves as a precursor to thyroid hormone triiodothyronine (T3).
The active form of thyroid hormone which directly impacts the body's metabolic rate by affecting the function of cells throughout the body.
A long-lasting or permanent condition resulting from autoimmune destruction of the thyroid gland.
A severe state of hyperthyroidism that is a life-threatening medical condition.
Separation of fingernails from the nail bed.
Absence of menstrual periods.
Bulging eyes.
The oral ingestion of a radioactive form of iodine, which is selectively taken up by the overactive thyroid cells.
The surgical removal of the whole thyroid gland.
Surgical removal of part of the thyroid gland.
Involuntary contraction or spasm of muscles.
A minimally invasive procedure that uses radiofrequency energy to heat and destroy thyroid nodules or hyperactive tissue.

