6.2 Review of Anatomy and Physiology of the Respiratory System
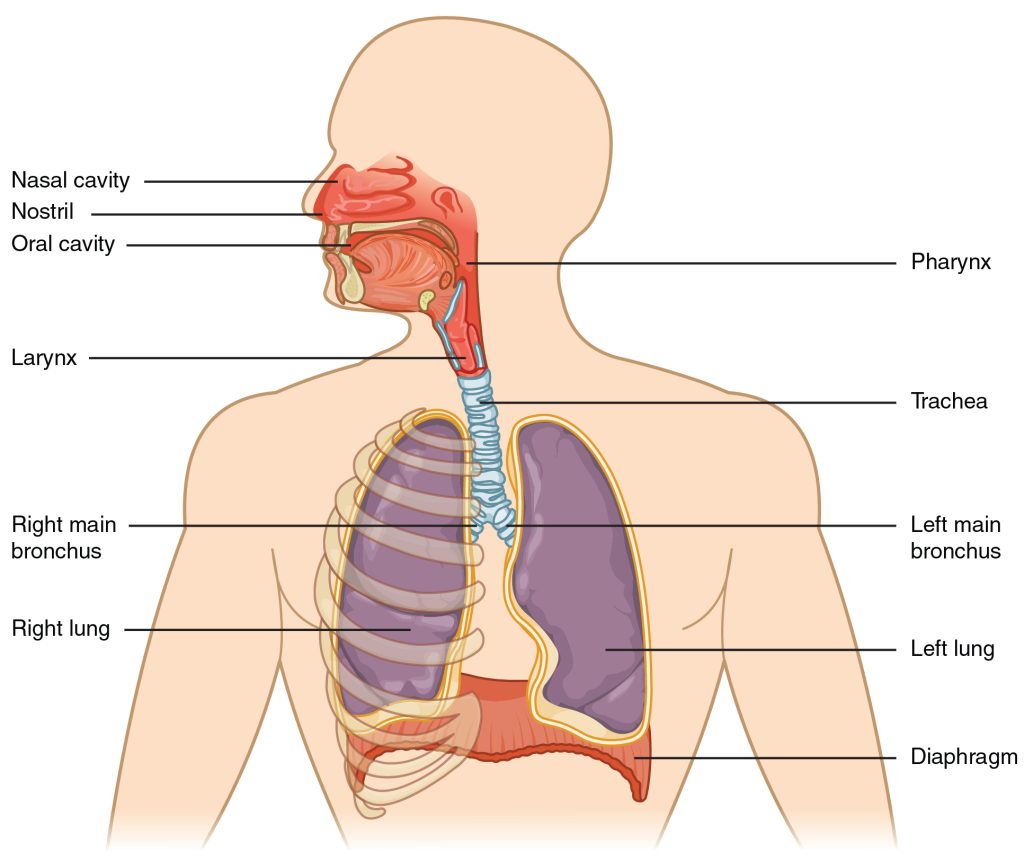
This section will review the anatomy and physiology of the respiratory system. Common disorders affecting these anatomic structures are also introduced. See Figure 6.1[1] for an illustration of the major structures of the respiratory system.
Nose, Nasal Cavity, and Sinuses
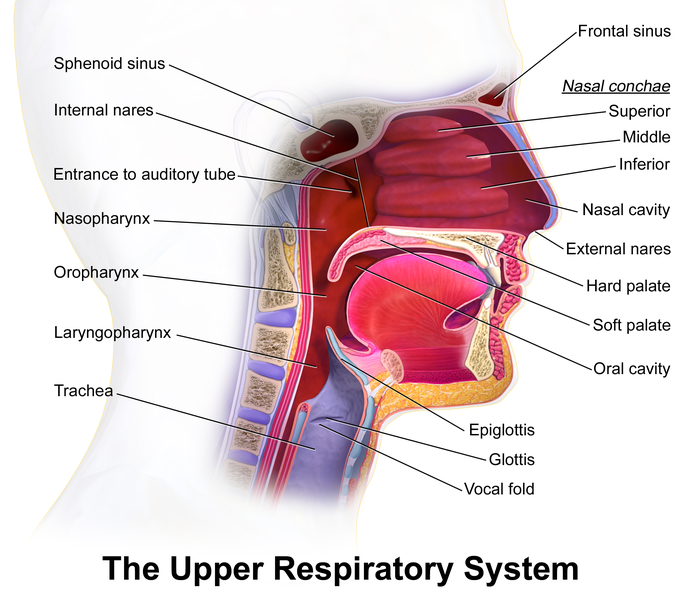
The upper respiratory system refers to the nose, nasal cavities, sinuses, pharynx, and larynx. See Figure 6.2[2] for an illustration of anatomic structures of the upper respiratory system. An upper respiratory infection (URI) refers to a viral infection of one or more of these structures.
The entrance and exit for the respiratory system are through the nose. The nostrils are the opening to the nose, also referred to as nares. The nares and nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. Rhinorrhagia refers to bleeding from the nose, also called epistaxis. Rhinitis refers to inflammation of the nasal mucosa.
The nares open into the nasal cavity, which is separated into left and right sections by the nasal septum. The floor of the nasal cavity is composed of the hard palate and the soft palate. The nasal cavities are lined with mucous membranes that produce mucus, a substance created for lubrication and protection. Rhinorrhea, commonly referred to as a “runny nose,” is a medical term for excess mucus production by the nasal cavities.
Adjacent to the nasal cavity are the sinuses that serve to warm and humidify incoming air. There are four sinuses named for their adjacent bones: frontal sinus, maxillary sinus, sphenoidal sinus, and ethmoidal sinus. Air moves from the nasal cavities and sinuses into the pharynx. Sinusitis refers to inflammation of the sinus cavities.[3]
Pharynx
The pharynx, commonly known as the throat, is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx. See Figure 6.3[4] for an illustration of the regions of the pharynx.[5]
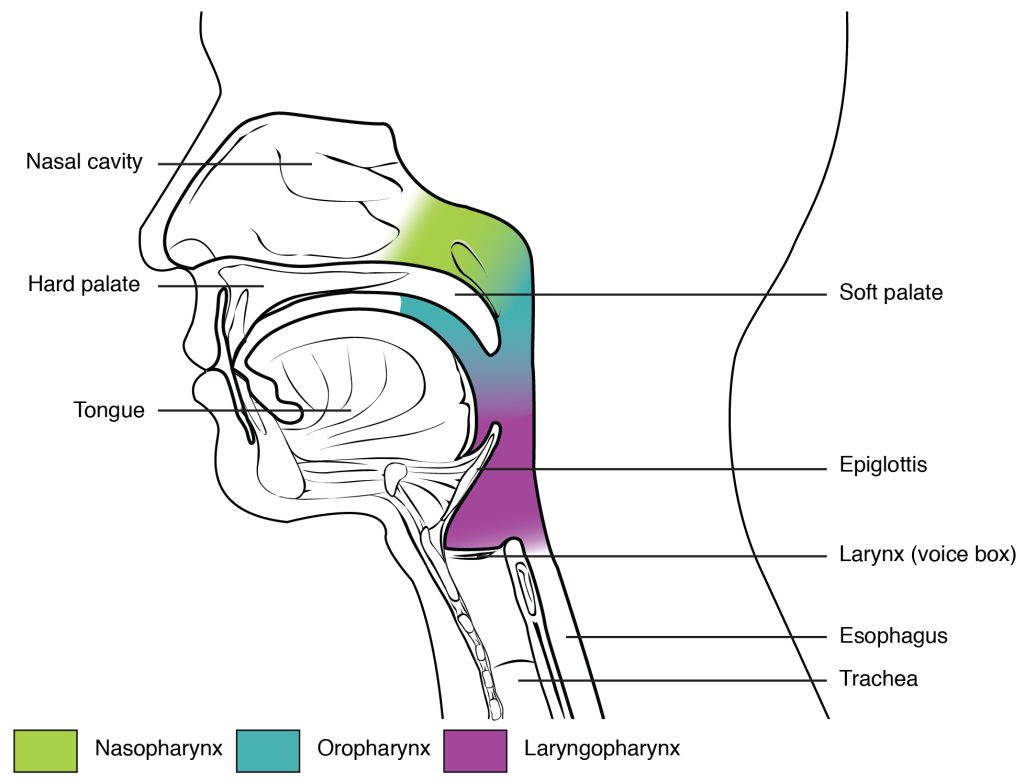
At the top of the nasopharynx is the pharyngeal tonsil, also called adenoid. The function of the pharyngeal tonsil is to trap and destroy invading pathogens that enter the airway during inhalation. Pharyngitis is inflammation of the pharynx, and tonsillitis is inflammation of the tonsils.[6]
The soft palate and a bulbous structure called the uvula swing upward during swallowing to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. Eustachian tubes connect the middle ear cavities with the nasopharynx. This connection is why upper respiratory infections often lead to ear infections.[7]
The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two distinct sets of tonsils called the palatine tonsils and lingual tonsils that also trap and destroy pathogens entering the body through the oral or nasal cavities. Adenoids are lymphatic tissue between the back of the nasal cavity and the pharynx. Adenoiditis refers to inflammation of the adenoids, a common medical condition in young children that can hinder speaking and breathing.[8]
The laryngopharynx is just below the oropharynx. It is part of the pharynx (throat) located behind the larynx. The laryngopharynx separates into the trachea (the tube going into the larynx) and the esophagus (the tube going into the stomach). The epiglottis prevents food and fluid from entering the trachea while swallowing.[9]
Larynx
The structure of the larynx is formed by several pieces of cartilage, as shown in Figure 6.4.[10] Three large cartilage pieces form the major structure of the larynx called the thyroid cartilage (the larger piece of cartilage on the anterior side), epiglottis (at the top of the larynx), and cricoid cartilage (just inferior to the thyroid cartilage). Laryngitis refers to inflammation of the larynx, specifically the vocal cords, typically resulting in huskiness or loss of one’s voice and a cough.[11]
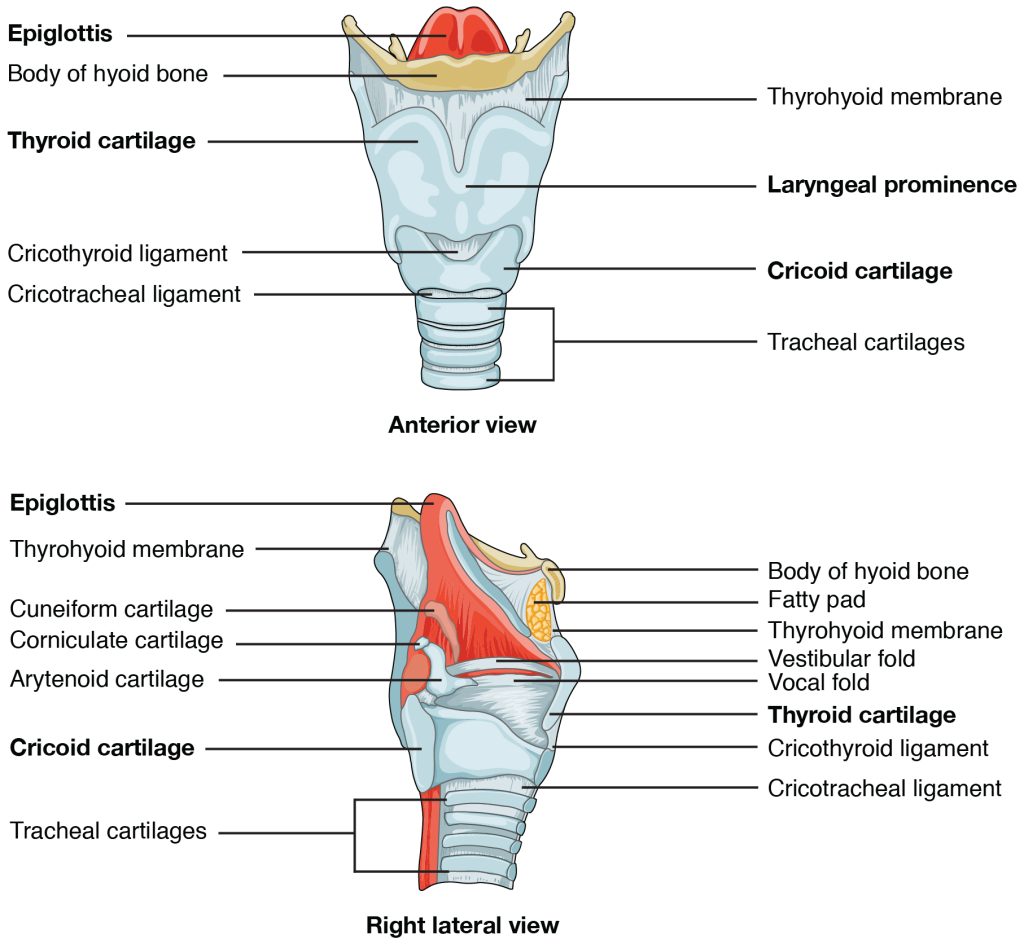
The epiglottis is a flap of tissue that covers the trachea during swallowing to prevent aspiration, the inhalation of food or fluids into the trachea and lower respiratory tract. The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea.[12]
Vocal cords are white, membranous folds attached by muscle to the cartilages of the larynx on their outer edges. The inner edges of the vocal cords are free, allowing oscillation as air passes through to produce sound for speaking.[13]
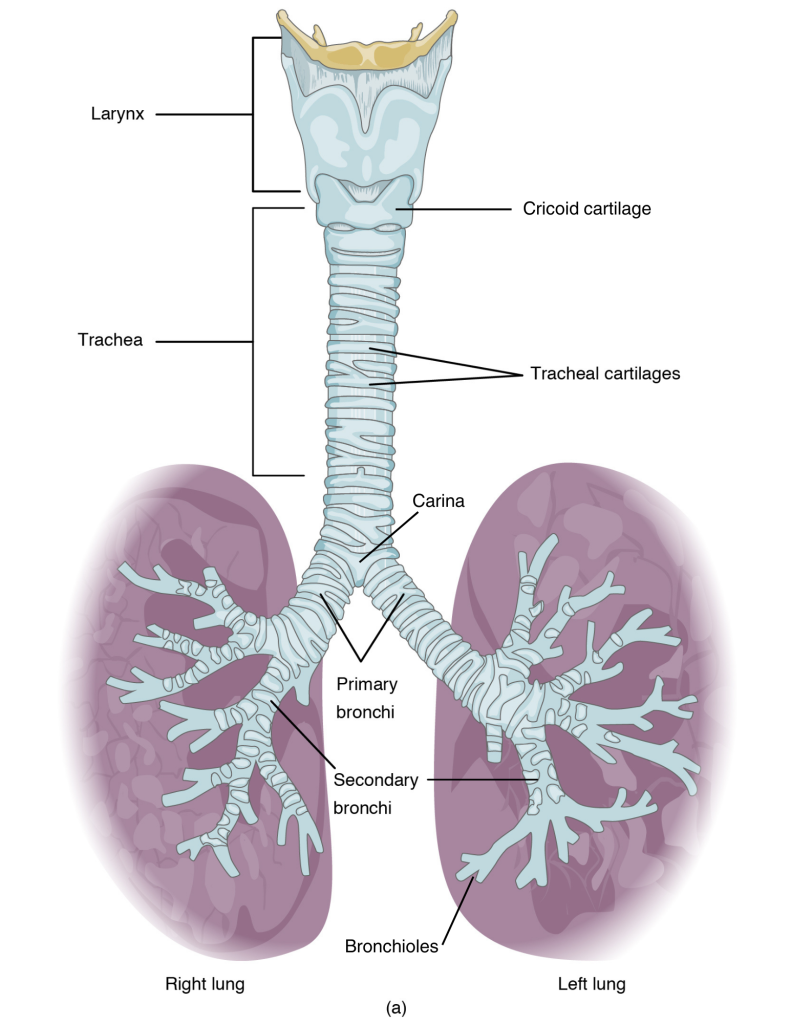
The lower respiratory tract consists of the trachea, bronchi, alveoli, and lungs.[14]
Trachea
The trachea is formed by stacked, C-shaped pieces of cartilage that are connected by dense connective tissue. See Figure 6.5[15] for an illustration of the trachea. The trachea stretches and expands slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. The trachea is lined with cilia and mucus-secreting cells to trap debris and move it towards the pharynx to be swallowed or spit out.[16]
If the upper respiratory tract becomes blocked with mucus, inflammation, or a foreign object, no air can pass to the lungs, causing a life-threatening emergency requiring a tracheostomy. A tracheostomy is an incision created in the trachea to create an artificial opening to allow breathing when an obstruction is present.[17]
Bronchi and Bronchioles
Bronchi are the main air passageways of the lungs. The trachea branches into the right and left primary bronchi at the carina. The carina is a raised structure that contains specialized nervous system tissue that induces violent coughing if a foreign body, such as food, is present. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. The bronchi of each lung continue to branch up to 26 times creating the bronchial tree, which looks similar to the branching of an actual tree. The main function of the bronchi is to provide a passageway for air to move into and out of each lung.[18]
Bronchioles are the smallest branches of the bronchi that lead to the alveolar sacs. The muscular walls of these tiny bronchioles do not contain cartilage like those of the bronchi, so the muscular wall can change the size of the bronchioles to increase or decrease airflow to the alveoli. Bronchospasm is a symptom of many respiratory conditions that refers to a sudden constriction of the muscles in the walls of the bronchioles. Bronchitis refers to inflammation of the bronchi.[19]
The trachea, bronchi, and bronchioles are lined with mucous membranes that create mucus secretions that can be expelled through the mouth, also referred to as sputum.[20]
Alveoli
Alveoli are small, grape-like sacs where gas exchange occurs. See Figure 6.6[21] for an illustration of one alveolus surrounded by capillaries. The blue capillaries refer to deoxygenated blood transported to the lungs from the pulmonary artery, and the red capillaries refer to oxygenated blood that is being transported back to the heart via the pulmonary vein. Note in this case that a vein is carrying oxygenated blood. Veins always carry blood back to the heart, but most of the time, it is deoxygenated. However, in this case, the pulmonary vein is transporting blood that is oxygenated back to the heart because it is being transported from the lungs.[22]
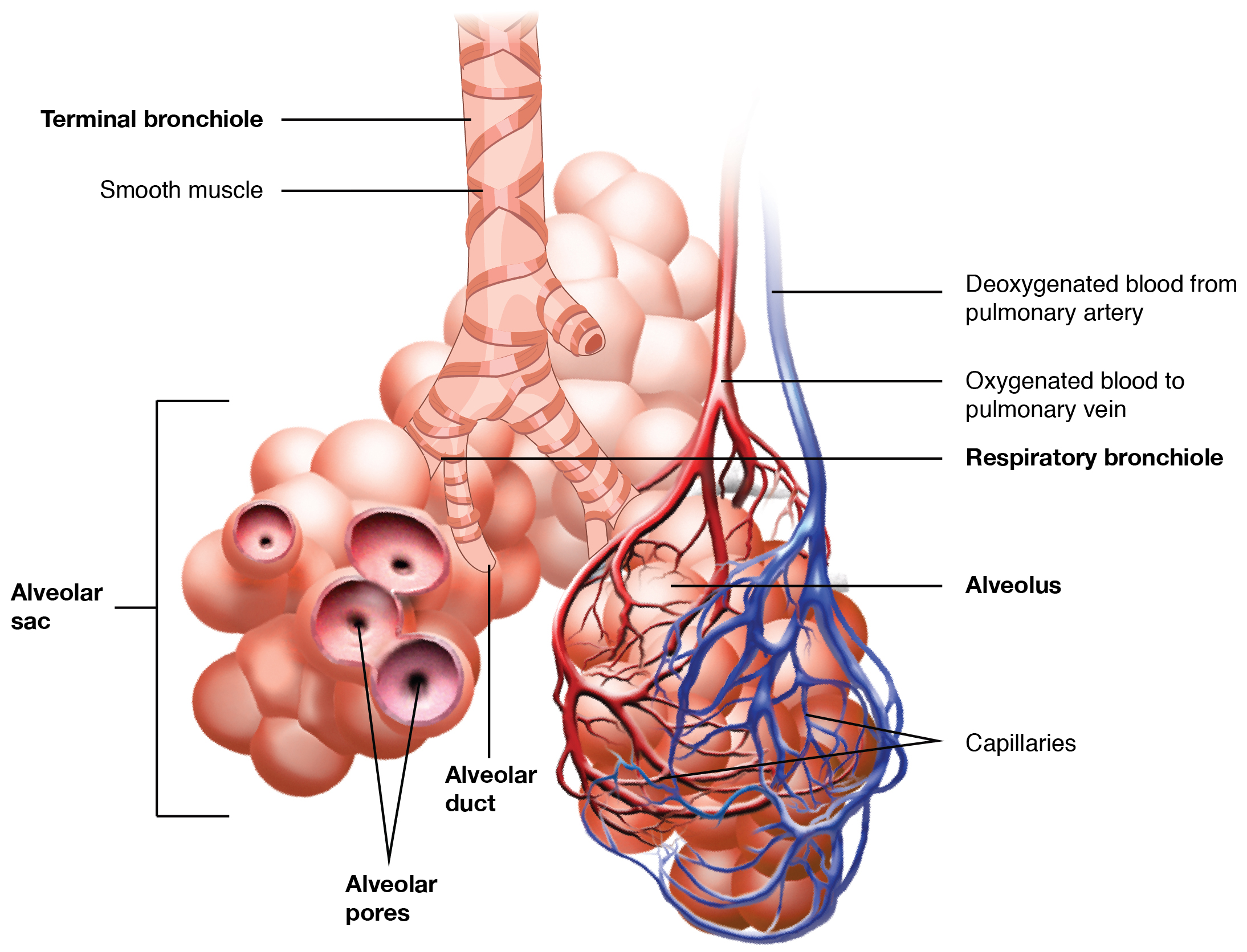
Alveoli have elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli secrete surfactant, a slippery substance that keeps the lungs from collapsing. Atelectasis is a medical term that refers to the collapse of alveoli and/or small passageways of the lungs that can result in a partially or completely collapsed lung.[23]
Lungs
The lungs are connected to the trachea by the main (primary) bronchi that branches into the right and left bronchi. See Figure 6.7[24] for an illustration of the lungs. On the inferior surface, the lungs are bordered by the diaphragm. The cardiac notch, a medial indentation found only on the left lung, allows space for the heart. The apex of the lung is the superior region, whereas the base is the distal region near the diaphragm.[25]
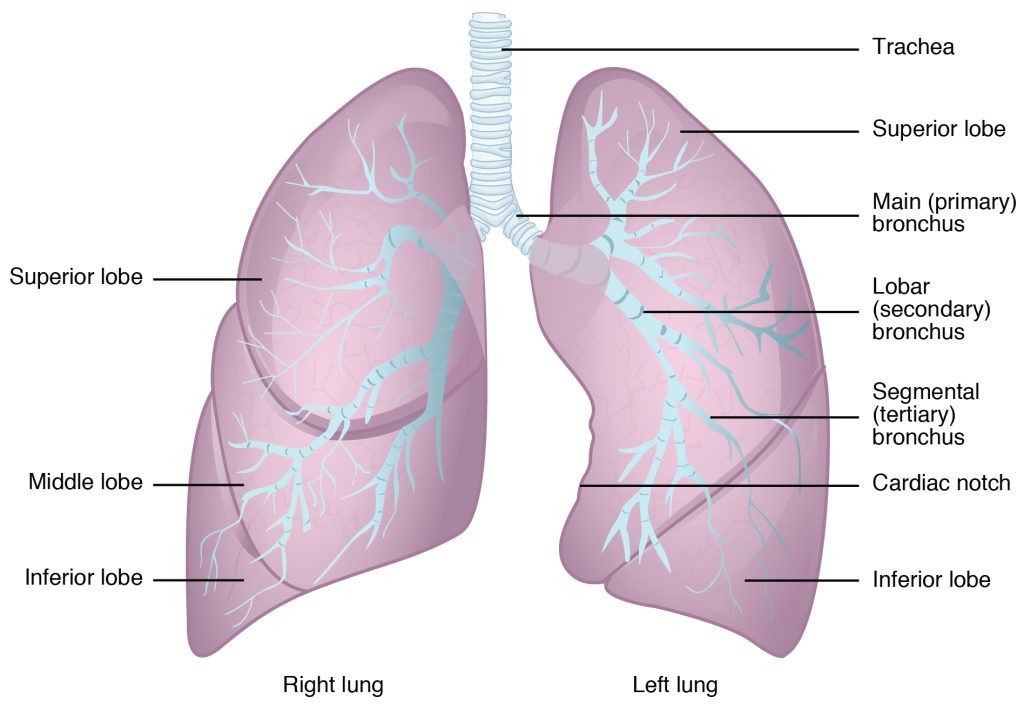
Each lung is composed of smaller units called lobes. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung is smaller and only contains two lobes, superior and inferior, as it shares space with the heart. Each lobe receives its own large bronchus that has multiple branches. A lobectomy refers to surgical removal of a lobe of the lung.[26]
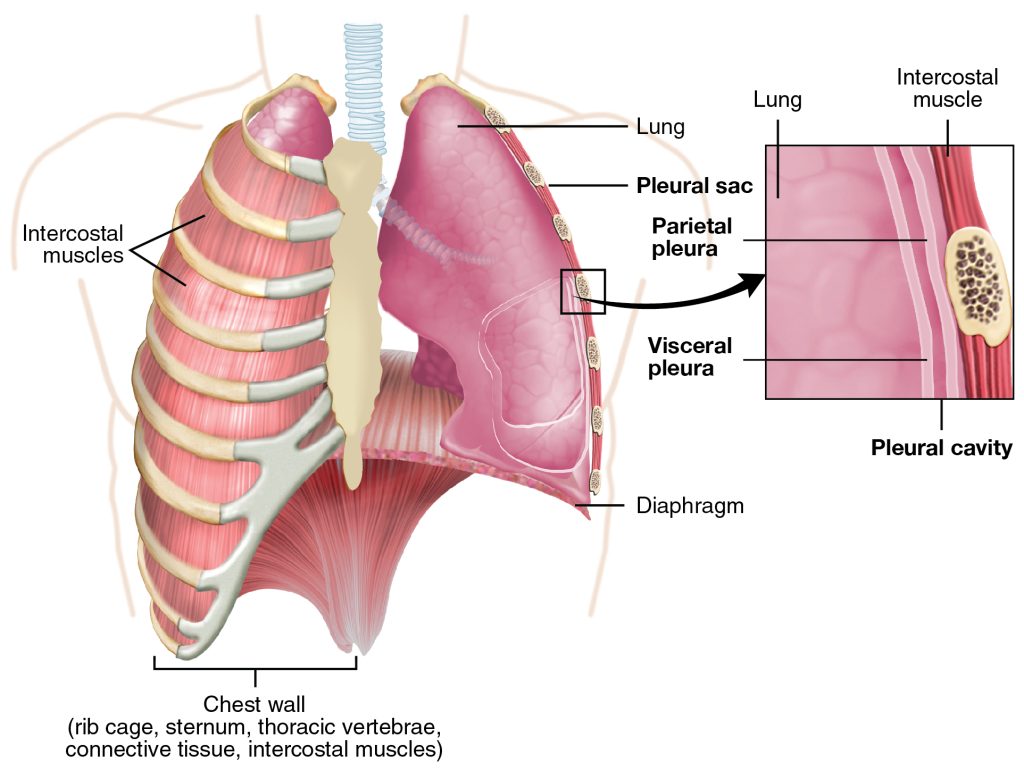
There are two pleural membranes in the lungs. The visceral pleura is a thin membrane on the outer surface of the lungs. The parietal pleura lines the inside of the thoracic cavity. Between these two membranes is the pleural cavity that contains pleural fluid to reduce friction and also sticks to the lungs to help keep them inflated. See Figure 6.8[27] for an illustration of the pleural membranes and the pleural cavity. Pleural effusion refers to excessive fluid between the pleural membranes that is commonly caused by disease or trauma.[28]
The main function of the respiratory system is gas exchange, meaning providing the body with a constant supply of oxygen to the body and removing carbon dioxide. To achieve gas exchange, the structures of the respiratory system create the mechanical movement of air into and out of the lungs called ventilation.[29]
Ventilation and the Mechanics of Breathing
The lungs bring oxygen to the cells of our body through inhalation and exhalation. Inhalation, also called inspiration, is the act of breathing air inward. During inhalation, the diaphragm contracts and flattens, creating a larger lung cavity, which decreases the pressure inside the lungs. At the same time, the intercostal muscles (the muscles between the ribs) pull downward, also causing the thoracic cavity to expand. The thoracic cavity is the space inside the chest that contains the heart, lungs, and other organs. As the thoracic cavity expands, a negative pressure (i.e., vacuum) is created inside the chest cavity, causing air to rush into the lungs (because air always moves from high pressure to low pressure).[30]
During exhalation, also called expiration or the act of breathing out, the diaphragm relaxes and the thoracic cavity springs back to its original position. This causes the volume of the thoracic cavity to decrease and pressure to increase, causing air to leave the lungs.
Lung sounds are caused by the movement of air from the trachea to the bronchioles to the alveoli and can be impacted by the presence of sputum, bronchoconstriction, or fluid in the alveoli. These sounds are referred to as rhonchi (coarse crackles), rales (fine crackles), wheezes, stridor, and pleural rub[31]:
- Rhonchi, also referred to as coarse crackles, are low-pitched, continuous sounds heard on expiration that are a sign of turbulent airflow through mucus in the large airways.
- Rales, also called fine crackles, are popping or crackling sounds heard on inspiration. They are associated with medical conditions that cause fluid accumulation within the alveolar and interstitial spaces, such as heart failure or pneumonia. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling noises produced when air is forced through airways narrowed by bronchoconstriction or mucosal edema. For example, clients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with obstruction of the trachea/upper airway.
- Pleural rub sounds like the rubbing together of leather and can be heard on inspiration and expiration. It is caused by inflammation of the pleura membranes that results in friction as the surfaces rub against each other.
Listen to lungs sounds in the “Respiratory Assessment” section of the “Respiratory Assessment” chapter of Open RN Nursing Skills, 2e.
Forced breathing is a type of breathing that can occur during exercise, singing, or playing a musical instrument. During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract. Muscles of the neck contract and lift the thoracic wall, increasing lung volume, and accessory muscles of the abdomen contract, forcing abdominal organs upward against the diaphragm. This helps to push the diaphragm farther into the thorax, pushing out more air. In addition, accessory muscles help to compress the rib cage, which also reduces the volume of the thoracic cavity. These additional muscle contractions during inspiration also occur during labored breathing, a symptom of many respiratory disorders.[32]
Control of Breathing
Respiratory rate is the number of breaths taken per minute. The normal respiratory rate for adults is 12-20 breaths per minute. A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute. By the time a child is about eleven years old, the normal rate is closer to 14 to 22.
Respiratory rate may increase or decrease during illness or disease. Medical terms related to breathing include tachypnea (rapid breathing), bradypnea (slow breathing), and apnea (episodes of the absence of breathing). Dyspnea is a common symptom of respiratory disorders and refers to shortness of breath or a feeling of breathlessness.[33]
The respiratory rate is controlled by the respiratory center located within the medulla oblongata and pons in the brain stem, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood. These changes are sensed by central chemoreceptors, which are located in the brain, and peripheral chemoreceptors, which are located in the aortic arch and carotid arteries.
The major factor that drives breathing is not hypoxemia (a decreased amount of dissolved oxygen in the blood), but rather the concentration of carbon dioxide. Carbon dioxide is a waste product of cellular respiration and is toxic at high levels in the blood. Elevated levels of carbon dioxide are called hypercapnia. As carbon dioxide levels increase, the central chemoreceptors stimulate the contraction of the diaphragm and intercostal muscles, increasing the rate and depth of respirations to help rid the body of carbon dioxide. Hyperventilation refers to rapid and deep breathing. It can occur for many reasons such as anxiety and pain, but it can also be a sign the body is trying to compensate for acidosis and increasing the pH level by eliminating excess carbon dioxide.
In contrast, low levels of carbon dioxide in the blood stimulate shallow, slow breathing to help the body retain carbon dioxide. Hypoventilation refers to slow and shallow breathing.[34] Hypoventilation can occur for several reasons, such as oversedation by opioids and exhaustion from hyperventilation. It can also be a sign the body is trying to compensate for alkalosis by retaining carbon dioxide and decreasing the pH level.
Gas Exchange
Ventilation (i.e., the mechanics of breathing) provides air to the alveoli for gas exchange. Respiration refers to the exchange of gases in the lungs between the alveoli and the pulmonary capillaries or in the tissues between the systemic capillaries and cells/tissues.
Gas exchange refers to the exchange of oxygen and carbon dioxide through capillary walls of the alveoli and the pulmonary capillaries, called external respiration. During external respiration, oxygen from the air we breathe diffuses into the blood. Carbon dioxide (waste) diffuses out of the blood and into the alveoli where it can be exhaled. Throughout the rest of the body, gas exchange also occurs between the systemic capillaries and body cells/tissues, called internal respiration. During internal respiration, oxygen diffuses out of the systemic capillaries and body cells/tissues, and carbon dioxide diffuses from the cells/tissues into the systemic capillaries where it is carried to the lungs. It is through this process that cells in the body are oxygenated and carbon dioxide, the waste product of cellular respiration, is removed from the body.[35]
Perfusion
In addition to adequate ventilation, the second important aspect of gas exchange is perfusion. Perfusion refers to the flow of blood. In the lungs, perfusion occurs in the pulmonary circulation as it moves from the heart into the lungs and then back to the heart for distribution to the body. The pulmonary arteries carry deoxygenated blood from the heart into the lungs, where they branch and eventually become the capillary network composed of pulmonary capillaries. These pulmonary capillaries create the respiratory membrane with the alveoli. As the blood is pumped through this capillary network, gas exchange occurs.[36]
Although a small amount of the oxygen is able to dissolve directly into the blood from the alveoli, most of the oxygen binds to hemoglobin within the red blood cells. The more oxygen the hemoglobin in the red blood cells carry, the brighter red the color of the blood. Oxygenated blood returns to the heart through the pulmonary veins to the left atrium and ventricle, where it is pumped out to the body via the aorta. The hemoglobin on the red blood cells transports the oxygen to the tissues throughout the body.[37]
Hypoxia and Hypoxemia
Diseases and disorders affecting the respiratory system can cause hypoxia, defined as reduced tissue oxygenation. Hypoxia can occur due to inadequate ventilation or impaired perfusion, also referred to as V-Q mismatch, where the ratio of air ventilating the lungs’ alveoli (V) to blood perfusing through the surrounding capillaries (Q) is not properly matched.
Pulmonary edema is an example of hypoxia caused by inadequate ventilation due to fluid accumulation in alveoli, often caused by heart failure or kidney failure. As a result of the fluid accumulation, oxygen cannot move across the alveolar membrane into the blood, and carbon dioxide cannot be removed from the blood. As a result, hypoxia and hypercapnia (high levels of carbon dioxide) may occur, requiring urgent medical interventions to sustain life by decreasing carbon dioxide levels and increasing oxygen levels.[38]
Another example of hypoxia caused by impaired perfusion is a pulmonary embolism. Let’s take a closer look at pulmonary embolism in the box below.
Pulmonary Embolism
A pulmonary embolism (PE) can occur when a clot from elsewhere in the body travels through venous circulation and gets lodged in the blood vessels of the lungs. This impedes blood flow, and impacted lung tissue dies. PEs are medical emergencies that require emergent treatment. Diagnosis of pulmonary embolism involves various tests:
- CT pulmonary angiography (CTPA): Visualizes blood flow in the pulmonary arteries.
- D-dimer test: Detects the presence of a substance that may indicate the presence of a blood clot.
- Ultrasound: Checks for DVT in the legs.
- Ventilation-perfusion (V/Q) scan: Detects blood flow and air movement in the lungs.
Signs and symptoms of PE include sudden shortness of breath, sudden anxiety or feeling of “impending doom,” chest pain, rapid heart rate, coughing up blood, sweating, feeling lightheaded or dizzy, or leg swelling or pain if a DVT is present. Read more about DVT in the “Cardiovascular Alterations” chapter. Complications of PE include death of lung tissue, increased pulmonary pressure in the arteries of the lungs, and cardiac arrest. Rapid intervention is required if PE is suspected. Treatment includes blood thinners to prevent additional clotting, thrombolytic therapy to dissolve clots, inferior vena cava (IVC) filter to prevent clots traveling to the lungs, oxygen therapy, and supportive measures such as pain management and breathing exercises.[39]
The term hypoxia and hypoxemia are not synonymous. Whereas hypoxia refers to reduced tissue oxygenation, hypoxemia is defined as a decrease in the partial pressure of oxygen in the blood (PaO2). Hypoxemia can be caused by impaired delivery of oxygen to the tissues or defective utilization of oxygen by tissues. Additionally, hypoxemia and hypoxia do not always coexist. For example, clients can develop hypoxemia without hypoxia if there is a compensatory increase in their hemoglobin levels and/or cardiac output (CO).[40]
- “2301_Major_Respiratory_Organs.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “Blausen_0872_UpperRespiratorySystem.png” by Blausen.com staff (2014). Medical gallery of Blausen Medical 2014 is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- "2305_Divisions_of_the_Pharynx.jpg" by OpenStax College is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- “2306_The_Larynx.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- “Trachea” by Meredith Pomietlo is a derivative of "File:2308a_The Trachea" by OpenStax Anatomy and Physiology and is licensed under CC BY 4.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- “2309_The_Respiratory_Zone” by OpenStax College is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- “2312_Gross_Anatomy_of_the_Lungs.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- "2313_The_Lung_Pleurea.jpg" by OpenStax College is licensed under CC BY 3.0. ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2023). Nursing skills 2e. Open RN. https://wtcs.pressbooks.pub/nursingskills/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Ernstmeyer, K., & Christman, E. (Eds.). (2024). Medical terminology 2e. Open RN | WisTech Open. https://wtcs.pressbooks.pub/medterm/ ↵
- Centers for Disease Control and Prevention. (2023). Venous thromboembolism. https://www.cdc.gov/blood-clots/about/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/dvt/facts.html ↵
- Sarkar, M., Niranjan, N., & Banyal, P. K. (2017). Mechanisms of hypoxemia. Lung India, 34(1), 47–60. https://doi.org/10.4103/0970-2113.197116 ↵
A viral infection occurring in one or more of the structures of the upper respiratory system.
Bleeding from the nose.
Rapid flow of blood from the nose, also known as rhinorrhagia.
Inflammation of the nasal mucosa.
Separates the left and right sections of the nasal cavity.
Excess mucus production by the nasal cavities.
Inflammation of the sinus passages.
Commonly known as the throat.
Inflammation of the pharynx.
Lymphatic tissue between the back of the nasal cavity and the pharynx.
Inflammation of the adenoids.
Formed by several pieces of cartilage, it contains the vocal cords that allow for speech.
Inflammation of the larynx, typically resulting in huskiness or loss of one's voice and a cough.
A flap of tissue that covers the trachea during swallowing to prevent aspiration.
The inhalation of food or fluids into the trachea and lower respiratory tract.
Formed by stacked C-shaped pieces of cartilage that are connected by dense connective tissue.
An incision created in the trachea to create an artificial opening to allow breathing when an obstruction is present.
Main air passageways of the lungs.
A raised structure that contains specialized nervous system tissue that induces violent coughing if a foreign body, such as food, is present.
The smallest branches of the bronchi that lead to the alveolar sacs.
A symptom of many respiratory conditions that refers to a sudden constriction of the muscles in the walls of the bronchioles.
Inflammation of the bronchi.
Mucus secretions that can be expelled through the mouth.
Small, grape-like sacs where gas exchange occurs.
A slippery substance that keeps the lungs from collapsing.
Collapse of lung tissue.
Organ of the respiratory system responsible for gas exchange.
Small units of the lung.
Surgical removal of a lobe of the lung.
Area between the two membranes of the lung.
Excessive fluid between the pleural membranes that is commonly caused by disease or trauma.
Main function of the respiratory system, providing a supply of oxygen to the body and removing carbon dioxide.
The mechanical movement of air into and out of the lungs.
The act of breathing in.
The space inside the chest that contains the heart, lungs, and other organs.
Expiration or the act of breathing out.
Also referred to as coarse crackles, are low-pitched, continuous sounds heard on expiration that are a sign of turbulent airflow through mucus in the large airways.
Also called fine crackles, are popping or crackling sounds heard on inspiration.
Whistling noises produced when air is forced through airways narrowed by bronchoconstriction or mucosal edema.
Heard only on inspiration, sound associated with obstruction of the trachea/upper airway.
The rubbing together of leather and can be heard on inspiration and expiration.
Additional muscle contractions during inspiration.
The number of breaths taken per minute.
Rapid respiratory rate.
Slow breathing.
Episodes of the absence of breathing.
Shortness of breath.
A decreased amount of dissolved oxygen in the blood.
Elevated levels of carbon dioxide.
Rapid and deep breathing.
Slow and shallow breathing.
The passage of blood through the blood vessels.
The flow of blood in the lungs.
Reduced tissue oxygenation.
Hypoxia occurring due to inadequate ventilation or impaired perfusion.
An example of hypoxia caused by inadequate ventilation due to fluid accumulation in alveoli.

