5.7 Coronary Artery Disease
Overview
Coronary artery disease (CAD) is caused by plaque buildup that causes the inside of the coronary arteries to narrow over time, which can partially or totally block the blood flow to the muscle tissue of the heart. As previously discussed in this chapter, the process of plaque buildup is referred to as atherosclerosis.
Risk Factors
There are a variety of risk factors for CAD, referred to as modifiable and nonmodifiable risk factors. Modifiable risk factors include high blood pressure; high cholesterol; smoking; obesity; physical inactivity; and diets high in saturated fats, trans fats, sodium, and refined sugars. Chronic stress and excessive alcohol consumption can also play a role in the development of coronary artery disease.[1],[2] Nurses play an important role in educating clients about modifiable risk factors for CAD and healthy lifestyle choices that can reduce these risks.
There are also numerous nonmodifiable risk factors for coronary artery disease. The risk of coronary artery disease increases with age; men over the age of 45 and women over the age of 55 are at higher risk. Family history and genetics are also nonmodifiable risk factors, especially if a client has a first-degree relative who has been diagnosed with coronary artery disease or had a myocardial infarction (i.e., heart attack), especially at a young age. Specific ethnic groups, such as African Americans are also at higher risk for the development of cardiovascular disease.[3],[4]
Angina
As blood flow becomes partially blocked in coronary arteries due to atherosclerosis, individuals often experience chest pain called angina. Angina is caused by lack of oxygenated blood flow to heart muscle tissue, referred to as ischemia. See Figure 5.28[5] for an image of a client experiencing angina.[6] Because angina is caused by blockage of oxygenated blood flow to the heart tissue, it is often brought on by physical activity and an increased demand for oxygenated blood. Physical activity stimulates the heart to beat faster with stronger contractions to distribute oxygenated blood flow to muscle tissue throughout the body. However, if coronary arteries are partially blocked, the heart tissue itself may not receive enough oxygenated blood flow as this workload increases, resulting in angina.

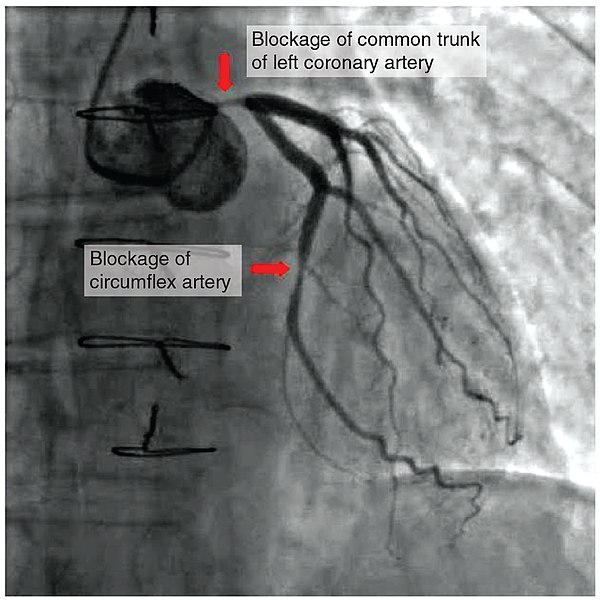
Angina is classified as stable or unstable. View Table 5.7 to compare the characteristics of stable versus unstable angina. Stable angina is caused by narrowing of the coronary arteries, resulting in partial blockage of blood flow. It is chronic, predictable, and relieved with rest or nitroglycerin. Clients may live with stable angina for several years and managed with medication. However, unstable angina is caused by worsening or a sudden blockage of blood flow to the heart that falls under the umbrella term of acute coronary syndrome (ACS). ACS refers to conditions that cause a sudden decrease in oxygenated blood flow to the cardiac muscle, ranging from unstable angina to myocardial infarction. As previously discussed, unstable angina is characterized by chest pain that does not resolve completely with rest or nitroglycerin. Myocardial infarction (MI), commonly referred to as a “heart attack,” occurs when there is a sudden blockage within the coronary arteries. Figure 5.29[7] shows a blockage in the coronary arteries of a client during a coronary angiogram that can result in a myocardial infarction without intervention.
Table 5.7. Characteristics of Stable and Acute Coronary Syndrome[8],[9]
| Characteristic | Stable Angina | ACS |
|---|---|---|
| Trigger | Typically triggered by exercise or emotional stress. | May occur at rest or with minimal exertion, sometimes with no apparent trigger. |
| Predictability | Generally predictable based on an individual’s specific activities. For example, an individual may be aware that climbing stairs will cause angina. | Unpredictable in terms of when it occurs and its severity. It may occur suddenly without warning. |
| Duration of Symptoms | Short duration that typically resolves within five minutes of rest or administration of nitroglycerin. | Longer duration than five minutes. Rest and/or nitroglycerin may improve but not completely resolve the pain. |
| Frequency | Predictable frequency. | Episodes of angina become more frequent over time. |
| Severity | Often described as pressure, heaviness, tightness, or squeezing over a broad area of the chest. | Often associated with shortness of breath and may also include symptoms of nausea, vomiting, diaphoresis, dizziness, and palpitations. Women may only experience fatigue and indigestion-type symptoms. |
| Progression | Rarely progresses to a myocardial infarction. | A serious warning sign of an impending myocardial infarction. |
| Management | Managed with lifestyle modifications and medications. | Requires immediate medical attention to prevent a myocardial infarction. |
When a myocardial infarction occurs, there are three types of potential damage to the cardiac muscle tissue: ischemia, injury, and infarction. When ischemia occurs, the viability of the tissue may be preserved if oxygen is promptly restored, and the heart muscle can recover without permanent damage. On an ECG, ischemia to cardiac muscle tissue is indicated by ST segment depression.
Next to the area of ischemia may be tissues that were injured. These tissues can be viable as long as oxygen is delivered to the tissue by pathways that circumvent the blockage. For example, providing supplemental oxygen during an MI may help save injured areas from necrosis (death). Areas of injury to cardiac muscle tissues may be indicated on an ECG by ST segment elevation. See Figure 5.30[10] for an illustration of ST elevations indicated by red arrows on an ECG strip.

The most significant area of damage during an MI is an area of infarct. Infarcted tissue has been deprived of oxygen for so long that the damage is irreversible, and the tissue has died. Troponin is a protein found in heart muscle cells that is released into the bloodstream when tissues have died and is used to help diagnose myocardial infarction. Cardiac muscle tissue that has died due to an infarct also causes a Q wave change on an ECG.[11] See Figure 5.31[12] for an illustration of a myocardial infarction.
Additional information regarding medical treatment for MI is provided in the following box.
Medical Treatment for MI
Nurses must recognize signs of unstable angina and implement appropriate action, such as notifying the provider and/or obtaining emergency assistance. Common interventions include the following[13],[14],[15]:
- Obtain stat ECG.
- Administer oxygen if SpO2 is less than 92% or per agency protocol, which helps ensure that the heart tissue receives adequate oxygen.
- Administer nitroglycerin to dilate the blood vessels and improve blood flow to the heart.
- Administer aspirin to reduce the opportunity for clot formation.
- Analgesics (such as morphine) may be prescribed to help reduce discomfort and cardiac workload, but morphine is no longer considered first-line treatment because of higher risk of death and adverse clinical outcomes.
- Mild anxiolytics may be prescribed for very anxious clients.
- Antiplatelet medications (such as clopidogrel) may be prescribed to reduce platelet aggregation and clot formation.
- Beta-blockers may be prescribed to reduce myocardial oxygen consumption by lowering heart rate, blood pressure, and myocardial contractility.
- Revascularization procedures, such as cardiac catheterization, stenting, or coronary artery bypass grafting surgery, may be required if vessel occlusion is significant.
Read additional information about MI treatment in the National Library of Medicine’s StatPearl Myocardial Infarction.
View a supplementary YouTube video[16] about acute coronary syndrome: How to Treat a Heart Attack
Assessment
Nurses assess subjective and objective data on physical examination and by reviewing laboratory and diagnostic test results.
Angina is the most common symptom of CAD. However, for many people, the first sign of CAD is a myocardial infarction (MI). Symptoms of an MI include the following[17]:
- Angina (Often described as heaviness, pressure, squeezing, or the feeling of something sitting on the chest)
- Shortness of breath
- Diaphoresis (Often described as “cold sweat”)
- Weakness
- Lightheadedness
- Nausea (Often described as “indigestion” or “feeling sick to your stomach”)
- Pain or discomfort in the jaw, arms, or shoulder
Over time, CAD can weaken the heart muscle. This may lead to heart failure, a serious condition where the heart can’t pump blood the way it should.[18]
Diagnostic Testing
Health care providers order various tests to assess the presence and severity of blockages within the coronary arteries. Depending on the severity of symptoms, providers may also order a coronary catheterization, considered the “gold standard” for the diagnosis of CAD. Common diagnostic tests related to CAD include the following.[19],[20],[21],[22]
- Troponin: A blood test used to help diagnose myocardial infarction that measures protein released into the bloodstream when heart tissue is damaged. Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
- Electrocardiogram (ECG or EKG): Measures the electrical activity, rate, and rhythm of the heart.
- Echocardiogram: Uses ultrasound (special sound wave) to create images of the heart.
- Exercise Stress Test: Evaluates the heart rate and rhythm while walking on a treadmill to determine how well the heart is working when it has to pump more blood.
- Cardiac Catheterization and Coronary Angiogram: Examines the inside of the coronary arteries for blockage by inserting a thin, flexible tube through an artery in the groin, arm, or neck to reach the heart. During the coronary angiogram, dye is administered to view the coronary arteries. Review additional information about cardiac catheterizations under the “Diagnostic Testing” subsection in the “General Cardiovascular System Assessment” section.
- Coronary Artery Calcium Scan: Examines coronary arteries for calcium buildup and plaque through computed tomography (CT).
- Cardiac Magnetic Resonance Imaging (MRI): Uses a magnetic field and radiofrequency waves to create detailed pictures of the heart and arteries.
- Coronary Computed Tomography (CCTA): Uses X-rays to take images of the heart and blood vessels. A computer combines the images to create a three-dimensional (3D) image of the heart.
Nursing Diagnoses
Nursing priorities for clients with CAD involve addressing inadequate oxygenation and managing pain, fatigue, activity intolerance, impaired cardiac output, and anxiety. Nursing diagnoses for clients with CAD are formulated based on the client’s assessment data, medical history, and specific needs. These nursing diagnoses guide the development of individualized care plans and interventions. Recall that symptoms of CAD are related to decreased oxygenated blood flow in the coronary arteries and can range from stable, chronic angina to acute coronary syndrome (ACS).[23]
Common nursing diagnoses for stable CAD include the following[24]:
- Acute Pain
- Risk for Decreased Cardiac Tissue Perfusion
- Risk for Decreased Cardiac Output
- Readiness for Enhanced Health Self-Management
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to CAD are as follows:
- The client will maintain adequate cardiac tissue perfusion as evidenced by the following vital sign ranges: SBP between 90 mm Hg – 120 mm Hg, HR 60-99 bpm, and O2 saturation greater than 92%.
- The client will report relief of angina within 5-10 minutes of rest and/or administration of nitroglycerin.
- The client will verbalize a decreased level of anxiety and demonstrate the use of relaxation techniques (e.g., deep breathing exercises) to effectively manage anxiety.
- The client will be able to participate in activities of daily living (ADLs) and physical activity.
Interventions
Medical Interventions
Medical interventions for CAD are aimed at managing symptoms, slowing disease progression, and improving quality of life. These interventions are typically prescribed by health care providers based on the severity of CAD, the client’s risk factors, and individualized needs and goals. Common medical interventions used to address CAD include medication therapy and lifestyle modifications. For severe CAD, surgical treatment may be performed.[25],[26]
Medication Therapy
Several classes of medications are used to treat CAD:
- Antiplatelet Medications: Help reduce the buildup of thrombotic plaque in the coronary arteries. Common medications include aspirin and clopidogrel.
- Cholesterol-Lowering Medications: Reduce the risk of atherosclerosis and plaque buildup. Common medications include statins like atorvastatin and simvastatin to lower LDL blood levels.
- Antihypertensive Medications: Control blood pressure and reduce strain on the heart. Common medications include beta-blockers, ACE inhibitors, and calcium channel blockers.
- Nitroglycerin: Relaxes and dilates coronary blood vessels to increase blood flow to cardiac muscle tissue and resolve angina.
- Antianginal Medications: Reduce the frequency and severity of angina. Examples include isosorbide, beta-blockers, and calcium channel blockers.
- Antiarrhythmic Medications: Used to manage abnormal rhythms. Because abnormal heart rhythms are associated with CAD, medications like beta-blockers or calcium channel blockers may be prescribed.
- Thrombolytic Therapy: Used to dissolve blood clots that are blocking coronary arteries during an acute myocardial infarction.
Read more information about these medication classes in “Cardiovascular & Renal System Medications” in Open RN Nursing Pharmacology, 2e.
View supplementary YouTube videos[27],[28],[29],[30] on common cardiac medications:
- Calcium channel blockers: CCBs for Hypertension (high blood pressure) or Arrhythmias (irregular heartbeat)
- ACE inhibitors: How do ACE inhibitors work?
- Nitrates: A Patient Guide: Nitroglycerin Jennifer Riccobono 252 subscribers Subscribe
Lifestyle Modifications
Several evidence-based lifestyle modifications are recommended by health care providers, including the following[31]:
- Healthy Weight: Carrying extra weight can put extra stress on the heart and blood vessels. Clients are encouraged to follow a healthy diet and incorporate regular physical activity to maintain a healthy weight.
- Heart Healthy Diet: A heart-healthy diet low in saturated fats, trans fats, cholesterol, and sodium is encouraged. Emphasis is placed on consuming fruits, vegetables, whole grains, and lean proteins while also considering cultural and religious diet preferences.
- Moderate Alcohol Consumption: Alcohol consumption can elevate blood pressure and should be consumed in moderation. Men should have no more than two drinks per day, and women no more than one drink per day.
- Regular Physical Activity: Physical activity is recommended to maintain a healthy weight and lower blood pressure, blood cholesterol, and blood sugar levels. For adults, the Surgeon General recommends 2 hours and 30 minutes of moderate-intensity exercise, like brisk walking or bicycling, every week. Children and adolescents should get 1 hour of physical activity every day.[32]
- Smoking Cessation: Smoking is a significant risk factor for CAD. If clients smoke, they are encouraged to consider quitting at every health care visit through counseling and nicotine replacement therapy.
- Mental Health: Various studies have shown the impact of trauma, depression, anxiety, and stress on the body, including stress on the heart. Clients are encouraged to talk to their health care providers about their mental health.
Surgical Interventions
In severe cases of CAD, these surgical procedures may be performed by cardiologists:
- Cardiac Catheterization With Angioplasty: A catheter is inserted into a narrowed coronary artery during cardiac catheterization. During the procedure, a balloon at the end of the catheter is inflated to widen the artery and improve blood flow. A small mesh device, known as a stent, may also be inserted to help keep the coronary artery open after the procedure is completed. Review information about cardiac catheterization under the “Diagnostic Testing” subsection in the “General Cardiovascular System Assessment” section.
- Coronary Artery Bypass Grafting (CABG): Blocked coronary arteries are bypassed using grafts (i.e., veins or arteries obtained from elsewhere in the body) to create new pathways for blood to flow to the heart muscle.
Cardiac Rehabilitation
Cardiac rehabilitation is a supervised program that includes physical activity, education about healthy lifestyle choices, and counseling to find ways to relieve stress and improve mental health. It is typically prescribed for clients who have had cardiac surgery, a myocardial infarction, or have been diagnosed with heart failure. Cardiac rehabilitation can help prevent another, perhaps more serious, heart attack and helps clients build heart-healthy habits.[33]
Read more information about How Cardiac Rehabilitation Can Help Heal Your Heart by the CDC.
Nursing Interventions
Nursing interventions for CAD focus on medication management, health teaching, safety promotion, and psychosocial support to facilitate overall cardiovascular health.
Medication Management
Prescribed medications are safely administered, and monitoring is provided for therapeutic effect and potential side effects. Teaching is provided about the role of medications, potential side effects, and when to notify the provider.
Health Teaching
Health teaching is provided about CAD, its risk factors, and the role of prescribed treatments and medications.
Guidance is provided for tracking blood pressure and monitoring cholesterol levels with lab work. Lifestyle modifications, as outlined under the “Medical Interventions” subsection, are taught and reinforced. Client understanding is evaluated, and follow-up teaching and/or cardiac rehabilitation is recommended as indicated.
Safety Promotion
Clients experiencing angina are taught how to properly use and store nitroglycerin.
Nitroglycerin Safety
Client teaching for nitroglycerin is crucial as it helps individuals understand how to use this medication safely and effectively.
- Instruct the client on the correct method of administration based on the prescribed form (sublingual tablets, transdermal patch, or spray).
- If using sublingual tablets, advise client to be in a seated position and then place the tablet under the tongue and allow it to dissolve.
- Clearly explain the prescribed dosage and the frequency with which nitroglycerin should be taken. Clients should be instructed to self-administer one tablet every five minutes for a total of three doses.
- Pain relief should start within one to two minutes of administration.
- Nitroglycerin tablets should be stored in their original container and protected from light.
- Inform clients about potential side effects of nitroglycerin, such as hypotension, headache, dizziness, or flushing. These effects are usually temporary but should be reported to the health care provider if persistent.
Clients and their family members are taught to recognize symptoms of an unstable angina and/or myocardial infarction and when to call 911.
Psychosocial Support
Nurses address the emotional and psychological impact of CAD by providing emotional support and making referrals to mental health professionals as indicated. Clients are also encouraged to participate in support groups and cardiac rehabilitation programs to maintain heart-healthy lifestyles.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Coronary Artery Disease
RN Recap: Coronary Artery Disease
View a brief YouTube video overview of CAD[34]:
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. https://www.uptodate.com/ ↵
- Mechanic, O.J., Gavin, M., Grossman, S.A., & Ziegler, K. (2023). Acute Myocardial Infarction (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568759/ ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. UpToDate. https://www.uptodate.com/ ↵
- Mechanic, O.J., Gavin, M., Grossman, S.A., & Ziegler, K. (2023). Acute Myocardial Infarction (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568759/ ↵
- “51096039583” by Marco Verch Professional Photographer’s photostream is licensed under CC BY 2.0 ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. UpToDate. https://www.uptodate.com/ ↵
- “2016 Occluded Coronay Arteries.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Goyal, A., & Zeltser, R. (2022). Unstable Angina. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK442000/ ↵
- Gillen, C., & Goyal, A. (2022). Stable Angina. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK559016/ ↵
- “ST Elevations” by Meredith Pomietlo is licensed under CC BY 4.0 ↵
- Mechanic, O.J., Gavin, M., Grossman, S.A., et al. (2023). Acute Myocardial Infarction (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568759/ ↵
- “Heart_attack-NIH.gif” by NIH: National Heart, Lung and Blood Institute is in the Public Domain. ↵
- Goyal, A., & Zeltser, R. (2022). Unstable Angina. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK442000/ ↵
- Gillen, C., & Goyal, A. (2022). Stable Angina. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK559016/ ↵
- Ojha, N., & Dhamoon, A.S. (2023). Myocardial Infarction. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537076/ ↵
- 7activestudio. (2017, January 15). How to treat a heart attack [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QllguanpKic ↵
- Centers for Disease Control and Prevention. (2023). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Centers for Disease Control and Prevention. (2023). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. UpToDate. https://www.uptodate.com/ ↵
- Centers for Disease Control and Prevention. (2023). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- American Heart Association. (2025). Cardiac computed tomography angiography (CCTA). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/cardiac-computed-tomography ↵
- American Heart Association. (2025). Cardiac magnetic resonance imaging (MRI). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/magnetic-resonance-imaging-mri ↵
- Mechanic, O.J., Gavin, M., Grossman, S.A., & Ziegler, K. (2023). Acute Myocardial Infarction (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568759/ ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. UpToDate. https://www.uptodate.com/ ↵
- Mechanic, O.J., Gavin, M., Grossman, S.A., & Ziegler, K. (2023). Acute Myocardial Infarction (Nursing). StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568759/ ↵
- 7activestudio. (2017, January 15). How to treat a heart Attack [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QllguanpKic ↵
- Drugs in Motion. (2018, December 10). CCBs for hypertension (high blood pressure) or arrhythmias (irregular heartbeat) [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QeVIGjJbE6g ↵
- British Heart Foundation. (2018, October 2). How do ACE inhibitors work? [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=xIlaQuRaZmk ↵
- Riccobono, J. (2012, September 11). A patient guide: Nitroglycerin [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=pII49Kn14Q8 ↵
- Centers for Disease Control and Prevention. (2025). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Centers for Disease Control and Prevention. (2025). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Centers for Disease Control and Prevention. (2025). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Open RN Project. (2024, April 4). Health Alterations - Chapter 5 Cardiovascular - Coronary artery disease [Video]. YouTube. CC BY-NC 4.0 https://www.youtube.com/watch?v=5KaFXLcRKNQ ↵
Plaque buildup that causes the inside of the coronary arteries to narrow over time, which can partially or totally block the blood flow to the muscle tissue of the heart.
Chest pain.
Condition in which oxygenated blood flow to tissue is reduced.
Conditions that cause a sudden decrease in oxygenated blood flow to the cardiac muscle, ranging from from unstable angina to myocardial infarction.
Commonly referred to as a “heart attack,” occurs when there is a sudden blockage within the coronary arteries.
Tissues lcoated next to ischemic area that can remain viable as long as oxygen is delivered to the tissue by pathways that circumvent the blockage.
The most significant area of damage during an MI.
A protein found in heart muscle cells that is released into the bloodstream when tissues have died and is used to help diagnose myocardial infarction

