11.5 Appendicitis
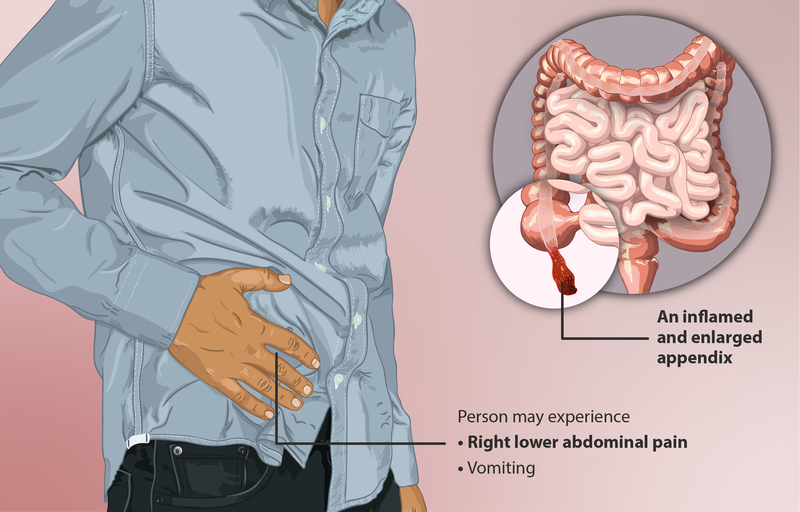
Appendicitis is an inflammation of the appendix, a hollow appendage that extends off of the cecum of the large intestine in the right lower quadrant of the abdomen. The true purpose of the appendix is unknown. Some believe the appendix is an organ with no true function, while others believe it serves a purpose in the immune system by harboring good bacteria. Appendicitis can occur at any age, but it is more commonly seen in those between 5 and 45 years of age. Males experience appendicitis slightly more frequently than females.[1] See Figure 11.24[2] for an image of an inflamed appendix.
Pathophysiology
Appendicitis occurs when something obstructs the opening of the appendix, such as a fecalith (mass of hardened feces), tumors, or even parasitic infections. Once the appendix becomes obstructed, pressure increases inside the appendix and occludes small blood vessels. The appendix also fills with mucus, leading to further distention and reduced blood flow to the appendix, ultimately causing necrosis. Bacterial overgrowth also occurs at this time.[3],[4]
Due to the large amount of inflammation, the appendix is at risk for rupture or abscess formation if not treated promptly. The risk of rupture drastically increases within 24-36 hours of symptom onset, so urgent medical care is essential. If the appendix does perforate, peritonitis may occur. Peritonitis is the inflammation of the peritoneum, the lining of the abdominal cavity.[5],[6]
Assessment
Physical Exam
The most common presenting symptom of appendicitis is abdominal pain. Initially, the pain is generalized, but eventually it shifts to the lower right quadrant of the abdomen. Rebound tenderness (pain that is more severe when releasing pressure on a tender area during palpation than when actively pressing on it) is also common. The client may also present with loss of appetite, nausea/vomiting, diarrhea, and fever.[7]
Common Laboratory and Diagnostic Tests
Lab Tests
Lab tests that are commonly ordered to diagnose appendicitis are a complete blood count (CBC) and C-reactive protein[8]:
- Complete blood count (CBC) assesses for an elevated white blood cell count. Typically, white blood cells will be elevated in those with appendicitis. However, one third of clients can have appendicitis with a normal white blood cell count. Severely elevated white blood cell counts are linked to complications of appendicitis such as perforation and gangrene formation.
- C-reactive protein (CRP) measures levels of inflammation. In cases of appendicitis, elevated levels of C-reactive protein may occur.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Diagnostic Testing
A diagnosis of appendicitis can be confirmed with various imaging techniques such CT scan, ultrasound, or MRI[9]:
- Abdominal CT scan is the preferred imaging modality for diagnosing appendicitis due to its specificity and accuracy.
- Ultrasound is not as specific or accurate as a CT scan, but it may be used in instances where radiation should be avoided, such as with children or pregnant women.
- MRI may be used for pregnant clients or for those who have had an inconclusive ultrasound or CT scan. MRIs are very accurate but expensive.
Nursing Diagnoses
Nursing priorities for clients with appendicitis include managing pain, preventing complications from occurring, and preparing the client for surgery.
Nursing diagnoses for clients with appendicitis are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client-specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Possible nursing diagnoses for clients with appendicitis are as follows[10],[11]:
- Acute Pain
- Risk for Infection
- Deficient Fluid Volume
- Anxiety
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes for some of the above nursing diagnoses are listed below:
- The client will rate their pain three or less (on a pain scale of zero to ten) within four hours.
- The client will remain free from signs and symptoms of infection during their hospitalization stay.
- The client will exhibit blood pressures and heart rates within normal limits for age, moist mucous membranes, and urine output appropriate for their age during their hospitalization stay.
- The client will describe three ways to manage preoperative anxiety by the end of the teaching session.
Interventions
Medical Interventions
There is no conservative treatment for appendicitis because of the risk for rupture; it must be treated surgically with an appendectomy (surgical removal of the appendix). In uncomplicated cases, surgery is performed laparoscopically. However, in situations where complications are present, an open appendectomy may be warranted.[12]
The client will receive an NPO order to prepare for surgery and reduce the risk for aspiration. Intravenous fluids are administered to prevent or correct dehydration. Antibiotics are commonly administered preoperatively to prevent infection. For clients with complications, such as abscess formation, antibiotics will be continued postoperatively. Lastly, if perforation has occurred or an abscess has formed, a percutaneous drain may be placed to allow for continual drainage.[13]
Nursing Interventions
When caring for a client with appendicitis and/or after an appendectomy, nursing interventions can be divided into categories of nursing assessments, nursing actions, and client teaching.[14],[15]
Nursing Assessments
- Assess pain on a 0-10 scale. Note and document location and characteristics of pain.
- Monitor for changes in vitals, as well as changes in the location or characteristics of pain that could signal complications such as abscess formation, rupture, or peritonitis.
- After surgery, assess for the return of bowel sounds before the client starts oral intake. Once bowel sounds have returned, clients should start with eating clear liquids and then gradually progress to a normal diet.
- Assess the surgical site for healing and signs of infection.
Nursing Actions
- Prior to surgery, complete the preoperative checklist. As with all urgent surgical procedures, nurses provide emotional support as needed to decrease client anxiety. For more information on preoperative checklists and preparing a client for surgery, review the “Preoperative Care” section in the “Perioperative Care” chapter.
- Administer prescribed pain medications. Ice may be used to manage pain, but heat should be avoided as it places the client at risk for rupture.
- Administer IV fluids as ordered. Monitor blood pressure, pulse, urine output, skin turgor, and mucous membranes to evaluate hydration status.
- Administer antibiotics per provider order.
- After surgery, encourage postoperative ambulation to prevent complications such as deep vein thrombosis or pneumonia. Ambulation will also encourage the return of peristalsis.
Client Teaching
- Encourage clients to increase fluid intake to prevent constipation from pain medications, immobility, and abdominal surgery. Enemas and laxatives should be avoided because they increase intra-abdominal pressure and the risk for rupture.
- Teach clients to monitor their incision/dressing and notify the provider of any signs of infection (redness, warmth, drainage, increasing pain, or fever). The client should also be taught how to self-manage wound care as indicated.
- Teach coughing and deep breathing strategies, as well as how to use an incentive spirometer, to prevent respiratory complications. If excessive pain occurs with coughing, the client should be taught to splint the incision with a pillow. Review information on coughing and deep breathing and incentive spirometers in the “General Respiratory System Assessments and Interventions” section of the “Respiratory Alterations” chapter of this text.
- Reinforce prescribed activity restrictions, such as avoiding heavy lifting, as ordered postoperatively.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
View a supplementary video on appendicitis: Appendectomy.[16]
![]() RN Recap: Appendicitis
RN Recap: Appendicitis
View a brief YouTube video overview of appendicitis[17].
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- “Depiction_of_a_person_suffering_from_Appendicitis.png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Belleza, M. (2023). Appendicitis. https://nurseslabs.com/appendicitis/ ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Belleza, M. (2023). Appendicitis. https://nurseslabs.com/appendicitis/ ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Belleza, M. (2023). Appendicitis. https://nurseslabs.com/appendicitis/ ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Lotfollahzadeh, S., Lopez, R. A., & Deppen, J. G. (2024). Appendicitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK493193/ ↵
- Belleza, M. (2023). Appendicitis. https://nurseslabs.com/appendicitis/ ↵
- Vera, M. (2023). 4 appendectomy (appendicitis) nursing care plans. https://nurseslabs.com/appendectomy-nursing-care-plans/ ↵
- Nucleus Medical Media. (2015) Appendectomy [Video]. All rights reserved. https://mdmercy.com/mercy-services/conditions/appendicitis ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 11 - Appendicitis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/nCxIgXEhBZ4?si=3knP_12cxZ4g2GMz ↵
Mass of hardened feces.
Inflammation of the peritoneum.
Pain when hand is withdrawn during palpation.
Surgical removal of the appendix.

