11.14 Hernia
A hernia is when internal organs or tissues bulge through an inappropriate opening. Common types of hernias are inguinal hernias, hiatal hernias, and ventral hernias[1],[2],[3],[4],[5]:
- Inguinal hernias occur in the inguinal canal. The inguinal canal is a passageway that contains the spermatic cord and blood vessels in men and the round ligaments in women. See Figure 11.36[6] for an image of the small bowel herniating through the inguinal canal of a male.
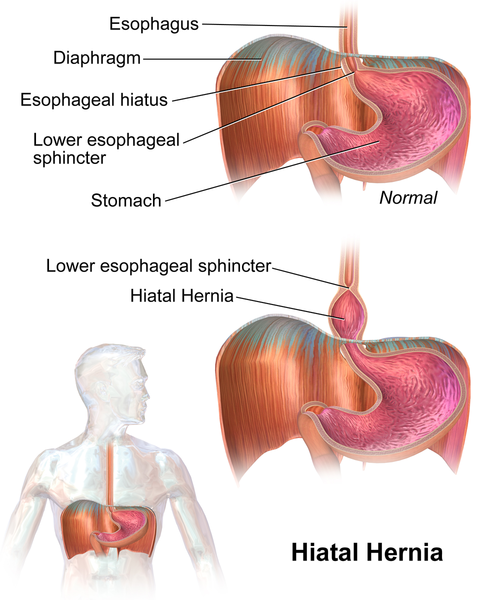
- Hiatal hernias are when part of the stomach bulges through the diaphragmatic opening. This opening of the diaphragm is also known as the esophageal hiatus as the esophagus passes through this opening on its way to the stomach. See Figure 11.37[7] for an illustration of a hiatal hernia.
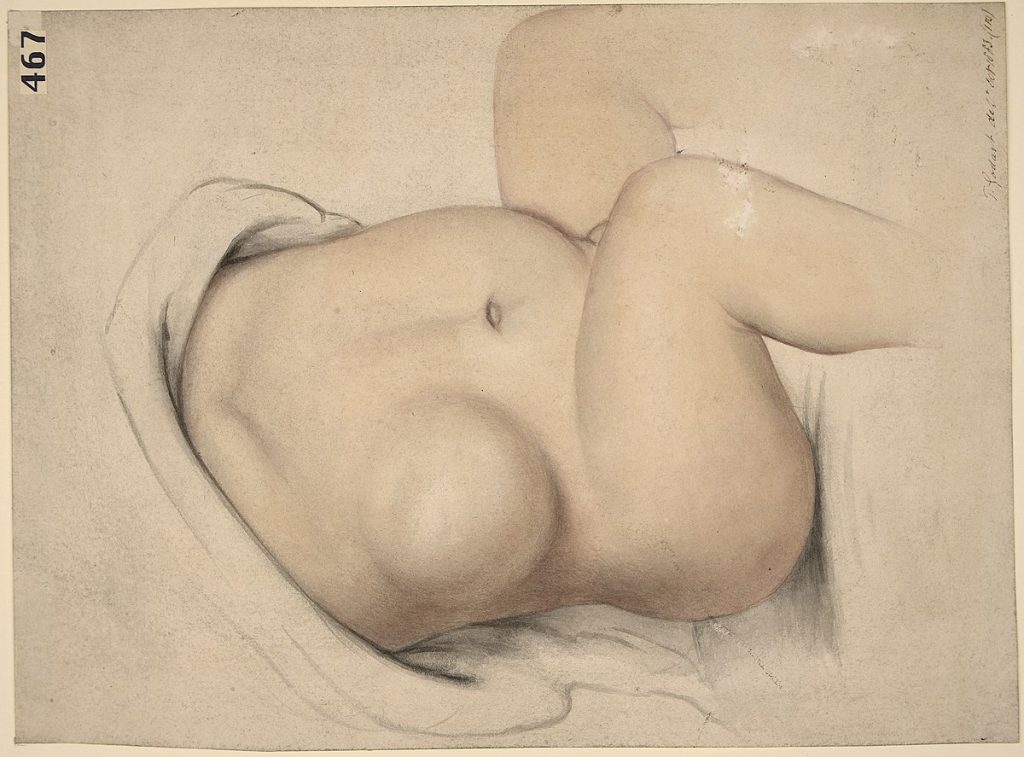
- Ventral hernias are hernias that occur in the wall of the abdomen and are neither inguinal nor hiatal in origin. See Figure 11.38[8] for an illustration of a ventral hernia in a child.
All types of hernias can be present at birth (i.e., congenital) or acquired over time, but they are most likely to be acquired. Risk factors for hernias depend on the specific type of hernia. See Table 11. 14 for a comparison of risk factors for inguinal, hiatal, and ventral hernias.[9],[10],[11],[12],[13]
Table 11.14. Hernia Risk Factors
| Inguinal Hernia | Ventral Hernia | Hiatal Hernia |
|---|---|---|
| Family history | Previous surgical procedures (leads to an incisional hernia or a hernia at the site of an incision) | Previous surgery |
| History of connective tissue disorders such as Ehlers-Danlos or Marfan syndrome | Trauma to abdominal wall | Trauma to abdominal wall |
| Increased intra-abdominal pressure (obesity, coughing, lifting of heavy objects, staining with bowel movements) | Stress to abdominal wall (obesity or frequent weight loss and gain) | Increased intra-abdominal pressure (obesity, pregnancy, straining with bowel movements, COPD) |
| Not linked to age, but much more common in males | Not linked to age | Older age |
| No genetic link | No genetic link | Genetic link |
Hernias can be further described as reducible or incarcerated. A reducible hernia means that the hernia and its contents can be pushed back into their normal anatomical space. An incarcerated hernia means that the hernia cannot be reduced. This can lead to a strangulated hernia, or when the hernia undergoes a reduction in oxygen supply due to reduced blood flow. This is considered a medical emergency that requires urgent surgical intervention.[14],[15],[16],[17],[18]
View a supplementary YouTube video[19] on hernias and hernia repair: Repairing a hernia with surgery.
Pathophysiology
Hernias usually occur when there is a combination of increased pressure, as well as an area of weakened tissue or musculature. The increase in pressure causes the organ or tissue to push through the weakened area.[20],[21],[22],[23],[24]
An inguinal hernia occurs when there is a weakened area in the oblique or transversalis muscles and abdominal organs protrude through the opening. These clients are also more likely to have increased levels of Type III collagen as opposed to Type I collagen, which is stronger. There is also a link between a patent processus vaginalis and the formation of an inguinal hernia. The processus vaginalis forms in fetal development. In males, it aids in the descent of the testicles through the inguinal canal. In females, it plays a role in the development of the round ligament. When this process does not occur in a normal fashion and the processus vaginalis does not close appropriately, the client is at greater risk for an inguinal hernia.[25],[26],[27],[28],[29]
In clients with a ventral hernia, recurrent stress to the abdominal wall leads to the development of small tears in the abdominal tissue. With time, the abdominal tissue has reduced strength and increased intra-abdominal pressure, which can lead to abdominal organs protruding through the weakened area.[30]
With a hiatal hernia, the stomach is pushed through the esophageal hiatus into the chest by one of the causative factors mentioned above. This compromises the integrity of the lower esophageal sphincter and is a leading cause of gastroesophageal reflux disease.[31]
Assessment
Physical Exam
Presenting signs and symptoms of a hernia will depend on the specific type and location of the hernia. Common signs and symptoms of inguinal and ventral hernias are as follows[32],[33]:
- Visible bulge in the area of the hernia
- Pain in the location of the hernia
- Increase in pain or size of bulge with activity, changes in position, or increases in intra-abdominal pressure
In addition to assessing for the aforementioned signs and symptoms, a physical exam can also aid in the diagnosis of inguinal and ventral hernias. With an inguinal hernia, the client is asked to stand so the health care provider can visualize the inguinal area for the presence of a bulge. The client will then be instructed to cough or bear down while the provider palpates the inguinal area. If there is a bulge that moves in and out with the increase in intra-abdominal pressure, an inguinal hernia is likely present. A ventral hernia can usually also be seen upon visualization of the abdomen. However, this should be done with the client in various positions as the appearance of the hernia can change based on the position of the client. Additionally, if the client is obese, a physical exam may have limited success in the diagnosis of a ventral hernia.[34],[35]
Common signs and symptoms of hiatal hernias are as follows[36]:
- Heartburn or other GERD symptoms
- Chronic coughing or asthma
- Regurgitation of stomach contents
- Difficulty or painful swallowing
If a hernia of any type becomes strangulated, the client may exhibit the following signs and symptoms[37]:
- Signs of a bowel obstruction such as nausea, vomiting, and absence of feces and flatus
- Severe pain
- Signs of sepsis (decreased blood pressure and elevated heart rate)
- Reddened or dusky skin over the hernia site (inguinal and ventral hernias only)
Common Laboratory and Diagnostic Tests
Although the presence of an inguinal or ventral hernia can often be detected via physical exam, imaging is often used to help confirm a diagnosis. Common imaging modalities used are ultrasound, CT scan, and MRI. An ultrasound is the least invasive modality, but not as sensitive and specific as an MRI. However, MRIs are expensive to perform, so a CT scan may be a better option in cases of unclear ultrasound results.[38],[39]
In those with a suspected hiatal hernia, there are a number of potential diagnostic tests. A barium swallow can show the presence of a hiatal hernia, as well as its size and specific location. A barium swallow can also show areas of narrowing that may have occurred due to chronic GERD. An EGD may be performed to diagnose a hiatal hernia. Esophageal manometry, a test that measures esophageal motility, can also be used to diagnose hiatal hernia, as well as rule out other conditions with similar symptoms. Lastly, although a CT scan is not a first-line tool to diagnose a hiatal hernia, it may be used if additional information is needed regarding the location and type of hiatal hernia.[40]
Lab tests are not used in the diagnosis of hernias, but they will be used when strangulation of a hernia is suspected. In the case of strangulation, a complete blood count may show elevated white blood cells, and lactic acid levels may be elevated if the client is septic.[41]
Nursing Diagnosis
Nursing priorities for those suffering from a hernia include managing symptoms, preventing complications, and client education.
Nursing diagnoses for clients with a hernia are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Common nursing diagnoses for those with a hernia are as follows[42],[43]:
- Acute Pain
- Risk for Injury
- Risk for Infection
- Readiness for Enhanced Knowledge
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes include the following:
- The client will rate their pain at 3 or less on a scale of 0 to 10.
- The client will remain free from signs and symptoms of a strangulated hernia (nausea, vomiting, absence of feces and flatus).
- The client will verbalize three methods to reduce their risk of contracting a surgical site infection after the teaching session.
- The client will describe common causes and treatment of hernias after the teaching session.
Interventions
Medical Interventions
Specific medical interventions depend on the type and severity of the hernia present. The medical treatment approach for each hernia type covered in this textbook will be described below.
Hiatal Hernias
In those with hiatal hernias, symptoms of GERD may be managed with proton pump inhibitors and lifestyle modifications such as losing weight, elevating the head of the bed, and avoiding eating before bed. If PPIs are able to manage symptoms in those with a hiatal hernia, surgical management may not be needed.[44]
Surgical management should be considered when the client’s symptoms are not managed with PPIs, when severe damage to the esophagus has occurred due to GERD, or when the hernia is large in size. Although there are a variety of options for surgical repair, a common procedure is the Nissen fundoplication. See the “Gastroesophageal Reflux Disease” section for more information on this procedure. Surgical management may be required for complications such as a gastric volvulus. A gastric volvulus is a type of obstruction in which the stomach twists upon itself.[45],[46]
Inguinal Hernias
If the inguinal hernia is asymptomatic, the provider typically recommends watchful waiting. Watchful waiting consists of monitoring the hernia for worsening symptoms. Surgical management is advised for symptomatic cases. Open and laparoscopic surgical methods have similar percentages for hernia recurrence. Although some approaches only repair the damaged tissue that allowed the hernia to occur, other approaches place a surgical mesh at the hernia site to support healing and prevent hernia recurrence.[47]
Ventral Hernias
As with inguinal hernias, those with asymptomatic ventral hernias may also undergo watchful waiting. Ventral hernias that present with incarceration but without strangulation should have the hernia repaired surgically, but it is not emergent. Clients who have a strangulated ventral hernia require emergency surgery. Ventral hernias can be repaired in an open or laparoscopic manner or even with the assistance of robotic technology. Those who undergo laparoscopic repair tend to have fewer complications and a shorter hospital stay than those who undergo an open procedure. As with inguinal hernia repair, there are a variety of surgical techniques that can be used, and the approach varies from repairing the damaged tissue to implanting a surgical mesh.[48]
Nursing Interventions
When providing nursing care for a client with a hernia, nursing interventions can be divided into nursing assessments, nursing actions, and client teaching.[49],[50]
Nursing Assessments
- Assess for increased tenderness, decreased appetite, and altered bowel movements, as this could indicate intestinal blockage due to incarceration or strangulation.
- Assess the client’s pain on a scale of 0-10. Pain is common after surgical repair of hernias and should be treated adequately. Changes in pain preoperatively could also indicate a complication such as a strangulated hernia.
- Assess the client’s surgical site after hernia repair for edema, erythema, and bleeding.
Nursing Actions
- Administer pain medications per provider order to manage the client’s pain.
- Administer stool softeners to prevent straining during bowel movements per provider order.
- Apply ice to the surgical site to reduce swelling and help reduce pain.
- Offer a scrotal support for male clients undergoing surgical repair of an inguinal hernia, as this can reduce swelling and optimize comfort levels.
Client Teaching
- Reinforce education given by the provider on the methods of surgical repair of hernias and ensure the client’s questions are answered.
- Encourage hernia prevention/recurrence by teaching the importance of maintaining a healthy weight, preventing constipation by eating high-fiber foods, avoiding lifting heavy loads, following postoperative activity restrictions, and seeking treatment for persistent coughing.
- Educate the client about the need to increase fluids and protein in the diet to promote healing and good nutrition.
- Educate the client on any wound care needs they will have after discharge, as well as how to monitor the surgical site for signs of infection.
Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
![]() RN Recap: Hernia
RN Recap: Hernia
View a brief YouTube video overview of hernia[51]:
- Curran, A. (2022). Hernia nursing diagnosis and nursing care plan. https://nursestudy.net/hernia-nursing-diagnosis/?expand_article=1 ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- “Inguinalhernia.gif” by National Institutes of Health is in the Public Domain ↵
- “Hiatal_Hernia.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Ventral_hernia_Wellcome_L0061630.jpg” by unknown author for Welcomimages.org is licensed under CC BY 4.0 ↵
- Curran, A. (2022). Hernia nursing diagnosis and nursing care plan. https://nursestudy.net/hernia-nursing-diagnosis/?expand_article=1 ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- Curran, A. (2022). Hernia nursing diagnosis and nursing care plan. https://nursestudy.net/hernia-nursing-diagnosis/?expand_article=1 ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- Johns Hopkins Medicine. (2015, March 10). Repairing a hernia with surgery [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=pLw3AjZx3NQ ↵
- Curran, A. (2022). Hernia nursing diagnosis and nursing care plan. https://nursestudy.net/hernia-nursing-diagnosis/?expand_article=1 ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- Curran, A. (2022). Hernia nursing diagnosis and nursing care plan. https://nursestudy.net/hernia-nursing-diagnosis/?expand_article=1 ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927 ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Sfara, A., & Dumitrascu, D. L. (2019). The management of hiatal hernia: an update on diagnosis and treatment. Medicine and pharmacy reports, 92(4), 321–325. https://doi.org/10.15386/mpr-1323 ↵
- Pastorino, A., & Alshuqayfi, A. A. (2022). Strangulated Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555972/ ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Smith, R. E., Sharma, S., & Shahjehan, R. D. (2024). Hiatal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK562200/ ↵
- Sfara, A., & Dumitrascu, D. L. (2019). The management of hiatal hernia: an update on diagnosis and treatment. Medicine and pharmacy reports, 92(4), 321–325. https://doi.org/10.15386/mpr-1323 ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Smith, J., & Parmely, J. D. (2023). Ventral Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499927/ ↵
- Curran, A. (2022). Hernia nursing diagnosis and nursing care plan. https://nursestudy.net/hernia-nursing-diagnosis/?expand_article=1 ↵
- Hammoud, M., & Gerken, J. (2023). Inguinal Hernia. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513332/ ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 11 - Hernia [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/n8tV3p0vg8Y?si=0OgLM1pdF93gVTp5 ↵
When internal organs or tissues bulge through an inappropriate opening.
A hernia that occurs in the inguinal canal.
A passageway that contains the spermatic cord and blood vessels in men and the round ligaments in women.
A hernia in which part of the stomach bulges through the diaphragmatic opening.
Opening in the diaphragm where
the esophagus passes through on its way to the stomach.
A hernia that occurs in the wall of the abdomen and is neither inguinal nor hiatal in origin.
A hernia at the site of an incision.
The hernia and its contents can be pushed back into their normal anatomical space.
The hernia cannot be reduced.
When the hernia undergoes a reduction in oxygen supply due to reduced blood flow.
Forms in fetal development; in males it aids in the descent of the testicles through the inguinal canal, and in females it plays a role in the development of the round ligament.
A type of obstruction in which the stomach twists upon itself.

