3.8 Sickle Cell Disease
Sickle cell disease (SCD) is the most common disorder affecting hemoglobin in the United States, affecting about 100,000 Americans.[1] It is a genetic hemoglobin disorder, resulting in chronic anemia, chronic pain, organ damage, and early death. Clients with SCD form sickle-shaped red blood cells instead of the usual biconcave disc-shaped cells. When triggered by a causative event, the RBCs become rigid and clump together. As a result, blood vessels become occluded, and there is decreased perfusion to tissues and organs.[2],[3] See Figure 3.8[4] for an illustration of the sickled cells that results in decreased perfusion during SCD.
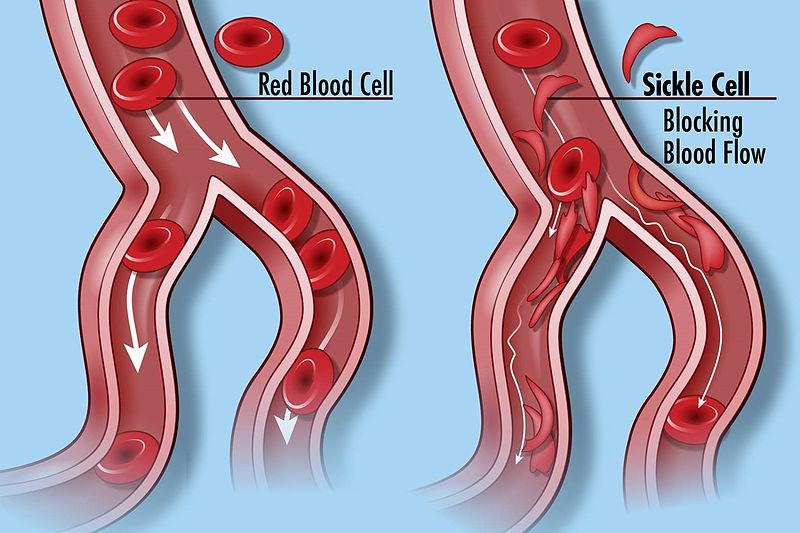
The pathophysiology of SCD occurs due to a genetic mutation of the hemoglobin gene, resulting in an abnormal hemoglobin called hemoglobin S (HbS). Sickle cell disease is an autosomal recessive genetic disorder where under certain conditions, the hemoglobin molecules form a long, rigid chain. The chains cause the red blood cells to change shape from a normal biconcave disc to a rigid sickle shape.[5],[6]
Individuals of African descent are at increased risk for SCD, with about 1 in 13 African Americans carrying the gene for HbS. If someone has the sickle cell trait, they are a carrier of the hemoglobin S gene, which means they can pass it on when they have a child. If two parents who are both carriers of the sickle cell trait have offspring, each child has a 25% chance of developing sickle cell disease.[7]
Advancement in new gene therapy has shown promise in clinical trials for developing a cure for SCD. This new technology entails removing the client’s stem cells from their bone marrow and adding a therapeutic gene to those cells, which leads to the production of anti-sickling cells.[8]
Pathophysiology
Many conditions can trigger the sickling of red blood cells in an individual with SCD, including dehydration, low oxygen levels, infection or inflammation, pregnancy, acidosis, temperature changes, stress, and high altitudes.[9],[10] Nurses help teach clients how to avoid these triggers.
During a vaso-occlusive crisis, the red blood cells become rigid and sickled and block small blood vessels, causing reduced perfusion of tissues. Because of the reduced blood flow causing decreased oxygenation of tissues and organs, vaso-occlusive events cause severe pain and can result in organ damage.
When individuals experience multiple vaso-occlusive events, significant and progressive damage occurs to organs and tissues, such as the kidneys, liver, spleen, heart, and lungs. Damage to the brain can occur without outward symptoms, called a silent stroke. Reduced perfusion in the legs can cause ulcers to form that may not heal and last for long periods of time. Joints can become damaged due to lack of perfusion, resulting in decreased mobility.[11]
Damage to the spleen reduces its ability to filter and remove damaged cells and bacteria from the bloodstream, causing clients to have an increased susceptibility to infections.[12],[13],[14]
Sickled red blood cells have a shorter life span than that of healthy red blood cells. As a result, there is a premature breakdown of red blood cells in the spleen, which can cause hemolytic anemia. Additionally, the breakdown of red blood cells causes the release of bilirubin. If the liver has experienced damage, jaundice may occur if it is not able to adequately metabolize the bilirubin. Bilirubin can also form gallstones that get stuck in the gallbladder.[15]
SCD is a painful, life-limiting disorder. Self-management education, psychosocial care, and genetic counseling are vital to help clients manage the disease and achieve the highest level of wellness possible.
Assessment
Physical Examination
Table 3.8 provides a summary of common clinical manifestations of SCD by body system.
Table 3.8. Common Clinical Manifestations of SCD by Body System[16],[17]
| Body System | Common Clinical Manifestations/Physical Assessment Findings |
|---|---|
| Central Nervous | Severe pain is a hallmark feature of sickle cell disease (SCD) because of lack of perfusion to body tissues and organs. Pain can be acute or chronic in nature. Pain is often severe and debilitating, requiring prompt and effective pain management. Decreased perfusion of the brain from repeated vaso-occlusive episodes can cause seizures or a stroke. |
| Cardiovascular | Cardiovascular symptoms include tachycardia, general fatigue, and weakness. Potential complications include heart failure and arrhythmias. |
| Respiratory | Respiratory symptoms include shortness of breath. Pulmonary complications include pulmonary hypertension and acute chest syndrome, a common cause of hospital admission and death associated with a respiratory infection. |
| Skin | Skin may appear pale or cyanotic due to decreased perfusion and/or decreased gas exchange resulting from the lack of hemoglobin. Skin may appear jaundiced due to RBC destruction, resulting in increased bilirubin levels. Clients may develop ulcers on the lower legs due to decreased perfusion. Wounds may have poor wound healing. |
| Abdominal | Diffuse and steady abdominal pain can occur during vaso-occlusive crises. Hepatomegaly (enlarged liver) and splenomegaly (enlarged spleen) may be present. Gallstones may occur. |
| Renal & Urinary | Kidney damage from poor perfusion and impaired gas exchange can lead to chronic kidney disease, resulting in decreased or no urine output. |
| Musculoskeletal | Joints may be damaged during vaso-occlusive crises, causing pain and decreased mobility, referred to as osteonecrosis (bone death). |
| Psychosocial | Anxiety, depression, and stress may occur related to chronic illness and pain. |
Diagnostic Testing
Laboratory tests commonly performed to identify sickle cell disease (SCD) include hemoglobin electrophoresis, complete blood cell count, reticulocyte count, peripheral blood smear, and bilirubin levels. These tests are ordered to help identify the presence of hemoglobin S and sickled red blood cells, immature blood cells, and lysing red blood cells.
Hemoglobin electrophoresis is a blood test that allows for the detection of abnormal types of hemoglobin. In this test, an electric current is applied to a sample of blood. This application of an electric current allows for the separation of normal and abnormal hemoglobin types. Normal types of hemoglobin are Hemoglobin A (the most common type in adults) and Hemoglobin F (the type of hemoglobin found in infants). Hemoglobin S, an abnormal hemoglobin, is the predominant type of hemoglobin present in those with sickle cell disease. High levels of Hemoglobin S are diagnostic for sickle cell disease.[18]
A complete blood count (CBC) can also be helpful in diagnosing SCD. In SCD, the red blood cells have a shorter life span of only about 10-20 days, versus a typical life span of 120 days. Therefore, a CBC for clients with SCD will show decreased numbers of red blood cells (RBC), hemoglobin, and hematocrit. Due to the anemia that results from SCD, there is also a high reticulocyte count due to compensation for the increased rate of RBC destruction. Reticulocytes are immature RBCs. Additionally, due to the rapid destruction and breakdown of RBCs, clients with SCD can also have elevated bilirubin levels. Bilirubin is released during the breakdown of RBCs. If the liver cannot keep up with the rate of RBC destruction, bilirubin levels build up and cause jaundice.[19],[20] Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
A peripheral blood smear can also be used to diagnose SCD. As mentioned in the “Diagnostic Testing” subsection in the “General Hematological System Assessment” section of this chapter, a thin layer of cells is examined under a microscope during a peripheral blood smear. In someone with SCD, the RBC will appear sickle-like in shape, especially when oxygen-deprived. Although this is a simple and inexpensive test, its accuracy is based on the expertise of the pathologist viewing the cells.[21]
Other diagnostic tests may be ordered to identify complications related to decreased perfusion that occurs during vaso-occlusive crises. For example, pulmonary function tests and electrocardiograms may be evaluated to identify respiratory and cardiac complications.[22],[23],[24]
Nursing Diagnoses
Nursing priorities for clients with sickle cell anemia include promoting adequate oxygenation and pain relief, decreasing incidences of vaso-occlusive crises, preventing complications, and helping the client self-manage the disease and effectively cope with it.
Nursing diagnoses for clients with sickle cell disease (SCD) are formulated based on the client’s assessment data, medical history, and specific needs. These nursing diagnoses guide the development of individualized care plans and interventions to address the unique challenges and complications of SCD.
Nursing diagnoses related to SCD include the following[25]:
- Acute Pain
- Chronic Pain
- Ineffective Peripheral Tissue Perfusion
- Risk for Infection
- Risk for Impaired Skin Integrity
- Decreased Activity Intolerance
- Readiness for Enhanced Knowledge
- Risk for Impaired Resilience
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating specific expected outcome statements for nursing diagnoses identified for the client. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to SCD are as follows:
- The client will report pain is controlled at an acceptable level to them (i.e., typically rated as 3 or less on a pain intensity rating scale of 0 to 10).
- The client will demonstrate adequate tissue perfusion as evidenced by vital signs within normal limits, palpable peripheral pulses, adequate urine output, capillary refill less than three seconds, and nail beds and lips of natural/pink color.
- The client will remain free from infection.
- The client will verbalize early symptoms of vaso-occlusive crisis and when to notify the health care provider.
Interventions
Interventions implemented for clients with SCD include medical interventions and nursing interventions.
Medical Interventions
Medical interventions for sickle cell disease aim to manage symptoms, prevent complications, and improve the overall quality of life for individuals living with the condition. Common medical interventions for sickle cell disease and sickle cell crisis include the following:
- Pain Management: Prompt and effective pain management is essential during vaso-occlusive crises. Pain relievers, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), may be effective for mild pain; severe pain during vaso-occlusive crises requires opioids. Morphine and dilaudid are typically administered on a routine schedule or using patient-controlled analgesia (PCA) pumps.
Read more about pain relievers and managing pain in the “Analgesics and Musculoskeletal System” chapter in Open RN Nursing Pharmacology, 2e.
- Hydration: Oral and intravenous (IV) fluids are prescribed during vaso-occlusive crises to rehydrate and improve perfusion, especially to the kidneys.
- Hydroxyurea Therapy: Hydroxyurea is a medication commonly prescribed for clients with SCD that stimulates the production of fetal hemoglobin (HbF) and reduces sickling of hemoglobin (HbS). However, hydroxyurea causes bone marrow suppression, so clients are at risk for abnormally low RBC, WBC, and platelets that can result in anemia, infection, or bleeding.[26] Hydroxyurea is also teratogenic, so it cannot be taken during pregnancy, and women taking it must be counseled to use effective contraceptives to prevent pregnancy.
- Blood Transfusions: Red blood cell transfusions may be prescribed to help increase the number of normal red blood cells and enhance their oxygen-carrying capacity, while also reducing the percentage of sickled cells. However, this is only a temporary fix and repeated transfusions put clients at risk for iron overload.
- Bone Marrow Transplant (Hematopoietic Stem Cell Transplantation): Bone marrow transplant is a potentially curative treatment for sickle cell disease. It involves administering chemotherapy to destroy and remove the client’s bone marrow cells and then replacing them with healthy stem cells from a compatible donor free of sickling. This transplantation can result in the client’s production of healthy red blood cells.[27]
- Antibiotics and Vaccinations: Prophylactic antibiotics and vaccinations are prescribed to prevent infections that can trigger sickling crises.
- Supportive Care: Supportive care involves addressing other aspects of sickle cell disease, such as preventing complications like leg ulcers and providing psychosocial support to address emotional and mental health needs.[28],[29]
Nursing Interventions
Nurses commonly perform these priority nursing interventions when caring for clients with SCD[30],[31],[32],[33]:
- Ensuring adequate oxygenation and providing supplemental oxygen therapy as indicated.
- Addressing acute and chronic pain through the administration of appropriate analgesics and nonpharmacological pain relief strategies.
- Preventing dehydration to help prevent vaso-occlusive crises and other complications.
- Implementing infection control measures to minimize the risk of infections, which can trigger sickle cell crises.
- Providing health teaching on self-management, pain management strategies, recognition of signs of complications, and signs or symptoms for health care provider notification.
- Providing psychosocial support and assisting the client to cope with chronic disease.
Each of these priorities is further discussed in the following subsections.
Ensuring Adequate Oxygenation
Decreased oxygenation and perfusion of tissues can occur in clients with SCD due to the decreased oxygen-carrying capacity of the sickled red blood cells (RBCs) and vessel occlusion that can occur during sickling of RBCs. Clients with sickle cell anemia are also more susceptible to bacterial pneumonia, which can further compromise gas exchange. Recall that lack of oxygenation also triggers additional sickling, so enhancing oxygenation and perfusion are vital.
Nurses monitor clients’ respiratory status and enhance gas exchange and tissue perfusion by performing the following interventions[34],[35]:
- Monitor respiratory status, including respiratory rate, use of accessory muscles, and lung sounds. Monitor pulse oximetry levels, but keep in mind the readings may be inaccurate due to the effects of decreased levels of hemoglobin. ABGs may be required to accurately monitor dissolved oxygen levels in the blood.
- Monitor peripheral perfusion, including peripheral pulses, skin color, capillary refill, pain in the extremities, and development of leg ulcers due to lack of perfusion.
- Monitor perfusion of major organs, including assessing level of consciousness, chest pain/angina, palpitations, dysrhythmias, and decreased urine output.
- Monitor for activity intolerance as demonstrated by fatigue and/or tachycardia, orthostatic hypotension, dyspnea, and/or chest pain on exertion.
- Administer oxygen therapy as indicated.
- Administer blood transfusions, as prescribed, to improve the number of oxygen-carrying red blood cells and improve oxygenation of tissues and organs.
- Implement energy management interventions (as described in the “Anemia” section)
- Maintain room temperature and body warmth without overheating to enhance tissue perfusion. Avoid extreme temperatures and overheating because this can lead to dehydration that can trigger vaso-occlusive crises.
- Encourage physical activity within the client’s limitations to prevent thrombosis.
- Administer hydroxyurea as prescribed and monitor for side effects.
- Avoid air travel in unpressurized aircraft and low oxygen levels at high altitudes because hypoxia can trigger vaso-occlusive crises.
Managing Pain
Clients with SCD often experience acute pain due to the vaso-occlusive nature of sickling, where sickled red blood cells block small blood vessels, causing tissue ischemia and inflammation. Chronic pain may also occur as a result of tissue damage from repetitive vaso-occlusive crises. Pain can occur in any part of the body, including bones, joints, chest, and abdomen. Nurses perform the following interventions to manage acute and chronic pain[36],[37]:
- Promptly assess pain using a pain rating scale and effectively provide pain management based on the client’s preferences.
- Administer analgesics, as prescribed, and monitor their effectiveness. NSAIDs may provide appropriate relief for chronic pain, but opioids are typically required during vaso-occlusive crises.
- Plan activities during peak analgesic effect to maximize movement of joints and enhance mobility.
- Apply warm, moist compresses to affected joints and avoid use of ice or cold compresses. Warmth causes vasodilation and increases circulation to hypoxic areas, but cold causes vasoconstriction.
- Provide additional nonpharmacological comfort measures such as keeping the room warm and repositioning with support devices for painful areas. Other cognitive-behavioral techniques for pain management include incorporating meditation, guided imagery, distraction, breathing, yoga, biofeedback, and progressive relaxation techniques.
- Encourage range-of-motion exercises within client’s limitations.
Promoting Hydration
Dehydration can trigger vaso-occlusive crises. Nurses encourage adequate daily oral fluid intake to prevent dehydration and administer IV fluids as prescribed during vaso-occlusive crises to help maintain adequate perfusion of tissues and organs.
Preventing Infection
Clients with SCD are at increased risk for infection and infection puts clients at risk for vaso-occlusive crises. Nurses educate clients and their family members about infection prevention measures, including routine vaccinations, hand hygiene, and avoiding exposure to sick individuals. Clients are also encouraged to follow a well-balanced diet rich in nutrients to support the production of red and white blood cells, as well as overall health.
Providing Health Teaching and Health Promotion
Nurses provide comprehensive health teaching to clients and their family members about sickle cell disease, common triggers of vaso-occlusive crises, signs of complications, home self-management techniques, and the need for seeking medical attention. Clients are encouraged to have regular medical check-ups, receive routine vaccinations, and take prescribed medications to prevent vaso-occlusive crises and future complications.
Providing Psychosocial Support
Nurses address the emotional and psychosocial needs of clients with SCD and their family members. Nurses encourage positive coping strategies and make referrals to support groups in the community to help individuals cope with the challenges of living with a chronic condition.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Sickle Cell Disease
RN Recap: Sickle Cell Disease
View a brief YouTube video overview of sickle cell disease[38]:
- Ashorobi, D., Naha, K., & Bhatt, R. (2023). Hematopoietic Stem Cell Transplantation in Sickle Cell Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538515/ ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- “Sickle_Cell_Disease_%2827249799083%29.jpg” by National Human Genome Research Institute (NHGRI) from Bethesda, MD, USA is licensed under CC BY 2.0 ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023, July 6). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- National Heart, Lung, and Blood Institute. (2024). What is sickle cell disease? National Institutes of Health. https://www.nhlbi.nih.gov/health/sickle-cell-disease ↵
- Ashorobi, D., Naha, K., & Bhatt, R. (2023). Hematopoietic Stem Cell Transplantation in Sickle Cell Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538515/ ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023, July 6). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- National Heart, Lung, and Blood Institute. (2024). What is sickle cell disease? National Institutes of Health. https://www.nhlbi.nih.gov/health/sickle-cell-disease ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- National Heart, Lung, and Blood Institute. (2024). What is sickle cell disease? National Institutes of Health. https://www.nhlbi.nih.gov/health/sickle-cell-disease ↵
- National Heart, Lung, and Blood Institute. (2024). What is sickle cell disease? National Institutes of Health. https://www.nhlbi.nih.gov/health/sickle-cell-disease ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- Medline Plus. (2023). Hemoglobin electrophoresis. https://medlineplus.gov/lab-tests/hemoglobin-electrophoresis/ ↵
- Cleveland Clinic. (2022). Reticulocyte count. https://my.clevelandclinic.org/health/diagnostics/22787-reticulocyte-count ↵
- Johns Hopkins Medicine. (n.d.). Sickle cell disease. https://www.hopkinsmedicine.org/health/conditions-and-diseases/sickle-cell-disease ↵
- Arishi, W. A., Alhadrami, H. A., & Zourob, M. (2021). Techniques for the detection of sickle cell disease: A review. Micromachines, 12(5), 519. https://doi.org/10.3390/mi12050519 ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- MedlinePlus. (2016). Blood count tests. National Library of Medicine. https://medlineplus.gov/bloodcounttests.html ↵
- Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladewig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Hydroxyurea. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK548724/ ↵
- Ashorobi, D., Naha, K., & Bhatt, R. (2023). Hematopoietic Stem Cell Transplantation in Sickle Cell Disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538515/ ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- American Society of Hematology. (n.d.). Sickle cell disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease ↵
- Centers for Disease Control and Prevention. (2023, July 6). What is sickle cell trait? U.S. Department of Health & Human Services. https://www.cdc.gov/sickle-cell/sickle-cell-trait/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/sicklecell/traits.html ↵
- Martin, P. (2023). 7 anemia nursing care plans. NursesLabs. https://nurseslabs.com/anemia-nursing-care-plans/#h-nursing-diagnosis. ↵
- Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladewig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Martin, P. (2023). 7 anemia nursing care plans. NursesLabs. https://nurseslabs.com/anemia-nursing-care-plans/#h-nursing-diagnosis. ↵
- Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladewig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Martin, P. (2023). 7 anemia nursing care plans. NursesLabs. https://nurseslabs.com/anemia-nursing-care-plans/#h-nursing-diagnosis. ↵
- Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladewig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Open RN Project. (2024, March 24). Health Alterations - Chapter 3 Hematological - Sickle cell disease [Video]. YouTube. CC BY 4.0 https://www.youtube.com/watch?v=vR5rDPn1m6E ↵
A genetic disorder characterized by abnormal hemoglobin molecules in red blood cells, leading to the formation of sickle-shaped cells instead of the usual biconcave disc-shaped cells.
Enlarged liver.
Bone death.
A blood test that allows for the detection of abnormal types of hemoglobin and often used when diagnosing sickle cell disease.
A test that can be used to diagnose SCD where a thin layer of cells is examined under a microscope to determine the shape of red blood cells.

