3.5 Anemia
Anemia is a condition characterized by a reduction in either the number of red blood cells, the amount of hemoglobin, or the hematocrit (percentage of red blood cells in the total blood volume). There are several types of anemia with different causes and treatments. Anemia itself is not a specific disease, but an abnormal condition that causes a decreased amount of oxygen delivered to body tissues, resulting in a variety of potential symptoms.[1]
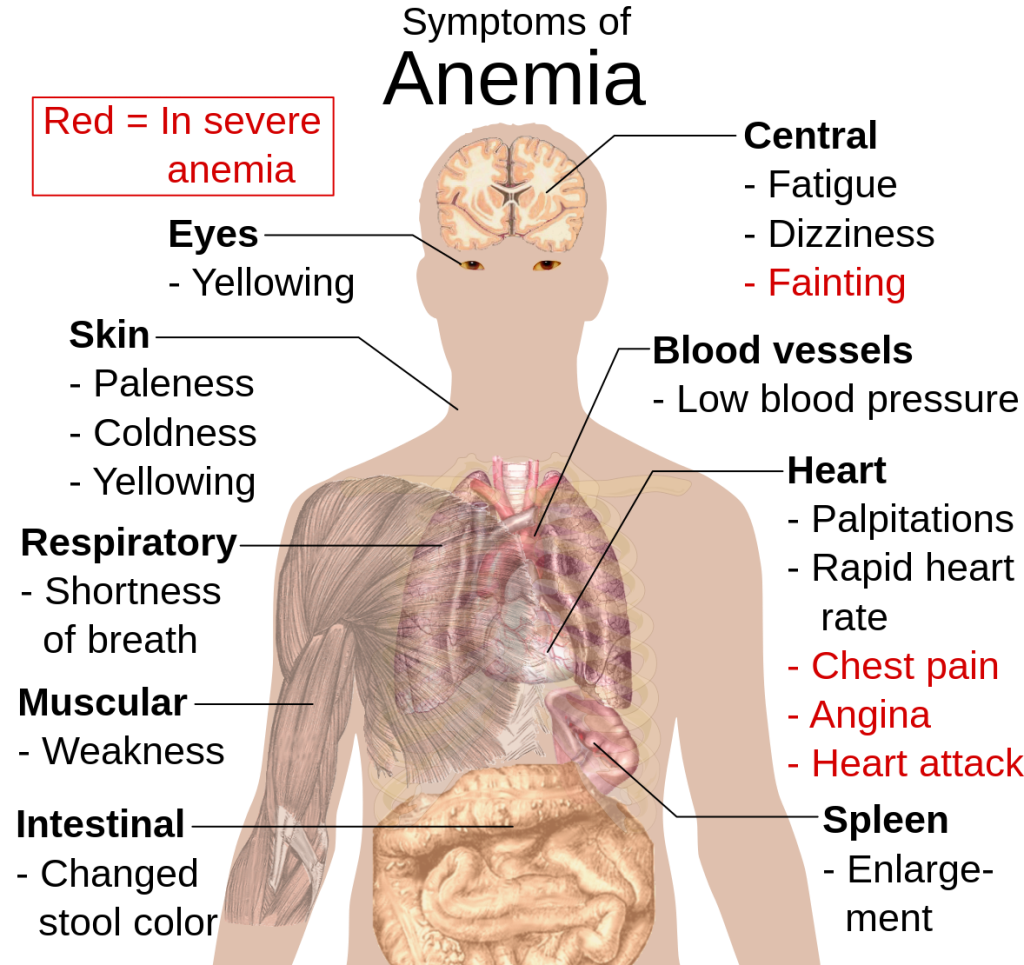
Common symptoms of anemia include fatigue, weakness, pale skin, unexplained shortness of breath, and heart palpitations.[2] Severe symptoms can include fainting, angina (chest pain), and myocardial infarction (heart attack). See Figure 3.7[3] for an illustration of the symptoms of anemia.
There are several common reasons for anemia in adults, including gastrointestinal (GI) bleeding caused by various gastrointestinal disorders such as peptic ulcers, inflammatory bowel disease, or colorectal cancer; chronic kidney disease; and excessive menstrual bleeding in females.[4]
Blood Transfusions
In severe cases of symptomatic, severe anemia (i.e., dyspnea or chest pain) or hemoglobin levels less than 7 g/dL, transfusions of red blood cells are typically prescribed to rapidly increase hemoglobin levels.
Registered nurses administer blood products according to hospital policies and protocols and assess the client for transfusion reactions and potential complications. Nurses also evaluate the effectiveness of blood transfusions by monitoring the client’s hemoglobin level. For each unit of RBCs transfused, the client’s hemoglobin level can be anticipated to increase by 1g/dL.
Nurses who administer blood products must complete specific training for safe transfusion practices and demonstrate competency in the transfusion administration process. The nurse is responsible for knowing which blood components are appropriate for specific client situations and serving as the last link in the chain of safety events. Agency policy and procedures must be strictly followed to prevent client harm. The nurse must verify that the client has signed informed consent for the procedure in their medical record.
Nurses must be aware of the client’s beliefs (and in the case of minors, their parents’ religious beliefs). Some religions, such as Jehovah’s Witnesses, oppose blood transfusions. They may be excommunicated from their church and the facility can be sued, even if the transfusion is implemented to save their life. This is another reason why it is critical to obtain written informed consent prior to initiating blood or blood product administration. It is essential to follow agency policies and procedures if a client (or the parent of a minor) refuses blood therapy.
Prior to blood product administration, the nurse confirms that a blood sample has been collected from the client and transported to the laboratory within the past 72 hours for typing and compatibility screening. This is the first step in maintaining client safety and preventing errors. Diligent client identification and blood product compatibility verification are vital for safe blood product administration. A two-person verification process is used for blood product transfusions. The first individual is the qualified transfusionist who will administer the blood or blood product to the client. The second individual conducting the identification verification process is qualified to participate in the verification process, as determined by the hospital. See Table 3.5a for an overview of nursing responsibilities related to administration of blood transfusions based on using the nursing process.
Table 3.5a. Nursing Responsibilities Related to Blood Product Administration[5]
| Assessment | Rationale |
|---|---|
| Verify written informed consent has been received for the procedure. Check the form to ensure it is properly completed and signed and assess client understanding of the procedure. | Infusion of blood is an invasive procedure with inherent risks and requires specific informed consent. Client understanding of the procedure and its rationale must be assessed by the nurse prior to its initiation. |
| Verify provider order for the blood product to be administered. Note any pre- or post-transfusion medications that have been prescribed. | A provider order is necessary before transfusing any blood product. Verifying the order and associated medications ensures they are appropriately administered. |
| Obtain client allergies, previous transfusion history, and transfusion reactions. | Gathering this data helps prevent transfusion reactions. If the client has had previous transfusion reactions, measures can be taken to help prevent another one from occurring. |
| Assess the recent laboratory values and results related to the blood product being transfused. | Ensure the type and screen has been completed. Assessment of other laboratory values provides a baseline comparison when evaluating the client’s response to the transfusion or in the event of a complication. |
| Analyze recent vital signs and notify the provider of any concerns. For example, if the client has a fever, clarify the order with the provider before obtaining the blood product from the blood bank. | If the client has any vital signs that are out of range and require clarification from the provider, this clarification should be addressed before obtaining the blood product because it typically must be initiated within 20-30 minutes of retrieval and cannot be returned. |
| Perform a respiratory assessment, skin assessment, and pain assessment. | Establish a baseline to use to trend future assessments and recognize changes in the event a transfusion reaction occurs. |
| Planning | |
| Review the indication for the transfusion with clinical supportive data. | The RN develops a plan of care and formulates expected outcomes of the procedure based on the indication for the transfusion. |
| Review expected outcomes for the client receiving a blood product transfusion. Expected outcomes of the transfusion are based on the indications for the transfusion. | Examples of expected outcomes for a PRBC transfusion include improved activity tolerance and improved hemoglobin and hematocrit to target range. |
| Determine if pre- or post-medication is needed for this specific client. | Diphenhydramine and acetaminophen are commonly prescribed for clients with a previous history of reactions. Anticipate that a client with a history of heart failure who will be receiving multiple units of blood may require furosemide to prevent fluid overload. |
| Implementation | |
| Verify venous access with 20G to 24G short peripheral catheters based on vein size and client preference, or 18G to 20G if rapid transfusion is required. Verify the integrity and patency of IV catheters. The distal lumen of a central venous access device may also be used to administer blood. | Correct catheter use ensures appropriate size, gauge, and viable intravenous access for the blood product.
A second venous access site may be required for administration of other fluids, medications, or other substances while blood is transfusing because they cannot be administered using the same line. |
| Use Y-infusion tubing sets specific to blood product administration and 0.9% normal saline IV fluid. | Only IV normal saline is compatible with simultaneous blood product administration. Lactated ringers, dextrose, hyperalimentation (artificial nutrients supplied intravenously), and other intravenous solutions with medications are not compatible with blood products. |
| Obtain blood or blood product from facility blood bank (follow agency policy). | Blood should not remain in the client care area for more than 30 minutes before the transfusion begins, so the nurse must be prepared to begin the transfusion shortly after the blood is delivered. |
| Perform the following checks with a second nurse or agency-defined trained health professional: compare the blood unit to the order, verify the client’s identity, verify the client’s blood type and Rh factor against the type of blood that will be infused, check the expiration of the blood component, and compare the client’s number against the blood product number. The nurses should also visually inspect the blood for any unusual color, precipitate, clumping, and any other unusual signs. | Checks by two nurses prevent transfusion reactions through proper client identification, verification of the prescription, and blood product compatibility. Note: The Joint Commission classifies a blood incompatibility error as a sentinel event (i.e., an event that is an unexpected occurrence resulting in death or serious physical or psychological injury, or the risk thereof).[6] |
| Obtain and document pre-transfusion vital signs and a baseline physical assessment. If the client is febrile (i.e., above 37.8° C or 100.4° F), notify the provider before starting the transfusion. | Baseline data and hemodynamic status must be established immediately before the transfusion begins so that manifestations of a transfusion reaction can be quickly recognized. For example, if a client develops fluid overload, a baseline assessment, including lung sounds, can be used for comparison with new findings. |
| An RN initiates the blood transfusion and remains with and monitors the client for a transfusion reaction for at least 15 minutes as the transfusion begins at a slow rate of 2 mL/min (i.e., 120 mL/hour). Ask the client to report unusual sensations (i.e., chills, hives, itching, shortness of breath, and chest pain). Note: All blood products must be completely administered in less than four hours. Administration sets are changed based on agency policy, commonly at the completion of every unit or every four hours. | Most transfusion reactions occur within the first 15 minutes of starting the transfusion. Blood products should not hang for more than four hours, and administration sets should be changed at the completion of each unit or every four hours to reduce bacterial contamination. |
| After 15 minutes, obtain another set of vitals. The RN determines an appropriate rate of transfusion based on agency policy and client considerations. | Most transfusion reactions occur within the first 15 minutes of starting the transfusion. The rate of infusion can be adjusted after the initial 15 minutes based on client tolerance. For example, a client with an active hemorrhage requires a fast rate whereas an elderly, symptomatic anemic client with a history of heart failure requires a slower rate. |
| If signs of a transfusion reaction occur, stop the transfusion and perform appropriate steps based on the agency’s transfusion reaction policy and protocol. Assess the client and obtain vital signs. Start normal saline with new primed tubing attached directly to the venous access device and notify the health care provider immediately. Do not infuse saline through the existing tubing because it will cause the blood in the tubing to enter the client. Do not discard the blood product or tubing; prepare it for lab analysis according to agency policy. | These steps prevent increased risks to the client. New tubing ensures that none of the blood product will further infuse into the client. Agency policy typically requires additional steps such as labs drawn, urine collection, and forms to be filled out and sent to lab. |
| Frequently monitor and assess the IV site and surrounding area. | Early detection of IV site complications improves client outcomes. |
| Evaluation | |
| After the procedure, evaluate and document client response and tolerance of the infusion, comparing current status to baseline data, such as physical assessment, vital signs, and lab results. Assess IV site to ensure integrity and patency after the infusion. | Evaluation determines if the goals of the transfusion therapy were achieved or if late onset transfusion complications are developing. Note: Some laboratory results may not reflect anticipated targets for several hours after the transfusion is completed. |
Nurses must be knowledgeable of potential complications that can occur during blood transfusions. The majority of transfusion reactions occur because of clinical error.
Delegation Tips
Each state’s Nurse Practice Act specifies if the skill of blood product transfusion can be delegated to a licensed vocational/practical nurse (LVN/PN) and if unlicensed assistive personnel (UAP) may collect vital signs after the first 15 minutes of the transfusion and the client’s stability has been confirmed. During the delegation process, the registered nurse (RN) should specify the frequency in which the client should be monitored and vital signs collected, as well as the parameters for vital signs and symptoms that should be immediately reported. Examples of parameters include an increased temperature, decreased pulse oximetry reading, shortness of breath, chest pain, hives, or chills. The RN retains responsibility and accountability for monitoring the client’s status during the transfusion.
Transfusion Reactions
Transfusion reactions are adverse events that are directly related to the transfusion of blood products and may range from mild to severe with life-threatening effects. The onset of transfusion reactions may occur during the transfusion (known as acute transfusion reactions) or in days or weeks following the transfusion (known as delayed transfusion reactions). Reactions may be an immune-related reaction or non-immunological condition. Immune-related reactions are often due to a mismatch or incompatibility of the transfused blood product and the recipient’s blood type or Rh factor. Non-immunologic reactions are typically caused by the physical effects of the blood component or the transmission of a disease.
It can be difficult to ascertain if a reaction will occur and what kind of reaction is occurring because some reactions can present with non-specific, overlapping manifestations. The most common manifestations of transfusion reactions include fever, urticaria, chills, and itching. Some mild symptoms may resolve without treatment, but some are severe, presenting with high fevers, respiratory distress, hypotension, and hemoglobinuria.[7]
The most common types of transfusion reactions include acute hemolytic, febrile non-hemolytic, delayed hemolytic, anaphylactic, simple allergic, transfusion-associated circulatory overload (TACO), transfusion-related acute lung injury (TRALI), and septic (bacterial contamination).[8] If a client experiences a blood transfusion reaction, always follow agency policy to manage mild to severe blood reactions. See Table 3.5b for additional information about different types of transfusion reactions, their causes, onset, manifestations, prevention, and related nursing interventions.[9]
Table 3.5b. Transfusion Reactions and Related Nursing Interventions[10]
| Transfusion Reaction | Cause | Onset | Manifestations | Prevention | Nursing Interventions |
|---|---|---|---|---|---|
| Mild to Moderate Allergic Reaction | Hypersensitivity to a foreign protein in the donor product. | During the transfusion and up to 24 hours post-transfusion. | Pruritus, erythema, local hives, urticaria, and bronchospasm. | If known history of a previous allergic reaction, may require administration of an antihistamine prior to infusion. | Stop transfusion and notify the provider. Administer antihistamine if prescribed and carefully monitor for new or progression of symptoms. Analyze vital signs every 15 minutes. |
| Anaphylactic | Recipient allergy to donor antigen (most often IgA). | Occurs within 5-15 minutes of initiation of transfusion. | Similar to mild/moderate allergic reaction, but more severe with nausea/vomiting, shortness of breath, cough, wheezing, hypotension, and loss of consciousness. May lead to cardiac arrest. | If known history of previous allergic reaction, transfuse with leukocyte – depleted RBCs. | Stop transfusion and notify the provider. Maintain IV access. Administer epinephrine, antihistamines, and corticosteroids as prescribed. Monitor vital signs frequently until stable. |
| Febrile Non-Hemolytic | Caused by cytokines released from blood donor’s leukocytes or platelets. Most common transfusion reaction that typically occurs in immunocompromised clients. | Occurs 30 minutes after initiation of transfusion to six hours post-transfusion. | Increased fever greater than 1-degree Celsius above baseline with associated flushing, chills, muscle pain, and headache. Tachycardia, tachypnea, and hypotension may also occur. | If known history of a previous febrile non-hemolytic reaction, use a leukocyte-reduced blood product. | Stop transfusion and notify the provider. If prescribed, administer antipyretics. Monitor temperature every four hours and as needed. |
| Acute Hemolytic | ABO and Rh incompatibility results in destruction of RBCs. | Occurs within 15 minutes of initiation of transfusion. | Flank pain, chest pain, increased heart rate, chills, increased temperature, low back pain, headache, dyspnea, bronchospasm, anxiety, hypotension, or pain along the accessed vein. | Considered a hospital-acquired condition preventable by diligent client identification and blood product compatibility verification. | Stop transfusion, remove blood tubing, and maintain access with 0.9% normal saline. Notify the provider and monitor vitals every 15 minutes. Obtain blood and urine samples and send to the lab with unused portion of blood product. |
| Septic | Contamination of blood product with bacterial microorganisms. | During transfusion and possibly up to two hours post-transfusion. | High fever, skin flushing, hypotension, back pain, abdominal cramping, nausea, and vomiting and diarrhea. | Complete transfusion within four hours to avoid bacterial growth. Proper care of blood product is required from donation through administration. | Stop the transfusion, remove blood product and tubing, and maintain IV access with 0.9% normal saline. Notify the provider. Monitor vital signs. Obtain blood cultures as prescribed. Administer fluids, obtain gram stain, and provide broad-spectrum antimicrobials as prescribed. |
| Transfusion-Associated Circulatory Overload (TACO) | Occurs when the volume of the transfusing blood component causes volume overload (hypervolemia) from an overly rapid administration rate or amount. | Can occur anytime during the transfusion or within one to two hours post-transfusion. | Crackles in lung bases, dyspnea, cough, tachypnea, tachycardia, hypertension, jugular vein distension, and headache. | Follow prescribed rate of infusion, typically 2 – 4 mL/kg/hr. Use caution with older adults and with those who have cardiac and renal disorders. | Reduce rate or stop transfusion as prescribed by provider. Monitor and manage client manifestations. Elevate head of bed and administer diuretic as prescribed. |
| Transfusion – Related Acute Lung Injury (TRALI)[11] | Acute lung injury caused by antibodies in the donor blood products that react with antigens in the recipient. Recipient chemical mediators are released and lead to pulmonary edema. | Within 6 hours to 72 hours of transfusion of blood products that are rich in plasma. | Cyanosis, dyspnea, fever, hypoxemia, hypotension, and pulmonary edema that is not cardiac-related (i.e., due to fluid overload). | Assess for contributing factors that predispose the client to this condition, including infection, inflammation, or recent surgery. | Stop the transfusion immediately and notify the provider. Administer treatment to support blood pressure as prescribed. Administer supplemental oxygen as prescribed. Prepare for endotracheal intubation and mechanical ventilation. Notify the blood bank so they can screen for certain donor antibodies. |
View this supplementary YouTube video[12] on blood transfusion reaction types:
Read additional information about blood product transfusions in the “Administer Blood Products” chapter of Open RN Nursing Advanced Skills.
- American Society of Hematology. (n.d.). Anemia. https://www.hematology.org/education/patients/anemia ↵
- American Society of Hematology. (n.d.). Anemia. https://www.hematology.org/education/patients/anemia ↵
- “Symptoms_of_anemia.svg.png” by Mikael Häggström is licensed in the Public Domain ↵
- American Society of Hematology. (n.d.). Anemia. https://www.hematology.org/education/patients/anemia ↵
- Blood and blood product transfusion. (2022). Lippincott procedures. http://procedures.lww.com ↵
- World Health Organization. (2022). Blood products. https://www.who.int/health-topics/blood-products#tab=tab_ ↵
- Lotterman, S., & Sharma, S. (2023). Blood Transfusion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499824/ ↵
- Lotterman, S., & Sharma, S. (2023). Blood Transfusion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499824/ ↵
- Lotterman, S., & Sharma, S. (2023). Blood Transfusion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499824/ ↵
- Lotterman, S., & Sharma, S. (2023). Blood Transfusion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499824/ ↵
- Lotterman, S., & Sharma, S. (2023). Blood Transfusion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499824/ ↵
- RegisteredNurseRN. (2018, March 20). Blood transfusion procedure nursing | Reaction types, complications (hemolytic/ febrile) NCLEX [Video]. YouTube. Used with permission. https://youtu.be/v4PHCwvkH24 ↵
A clinical sign characterized by a reduction in either the number of red blood cells, the amount of hemoglobin, or the hematocrit (percentage of red blood cells in the total blood volume).
Adverse events that are directly related to the transfusion of blood products and may range from mild to severe with life-threatening effects

