11.6 Cholecystitis
Cholecystitis is inflammation of the gallbladder due to impaired flow of bile due to blockage by gallstones or a poorly functioning gallbladder. Cholecystitis can be an acute or chronic condition. See Figure 11.25[1] for an image of a gallbladder containing gallstones that was surgically removed.

Cholecystitis can occur in men or women. Certain populations have a higher risk of gallbladder disease such as females or clients who are overweight, pregnant, in their 40s, or have experienced drastic weight loss. A family history of gallstone formation is also a risk factor.[2]
Pathophysiology
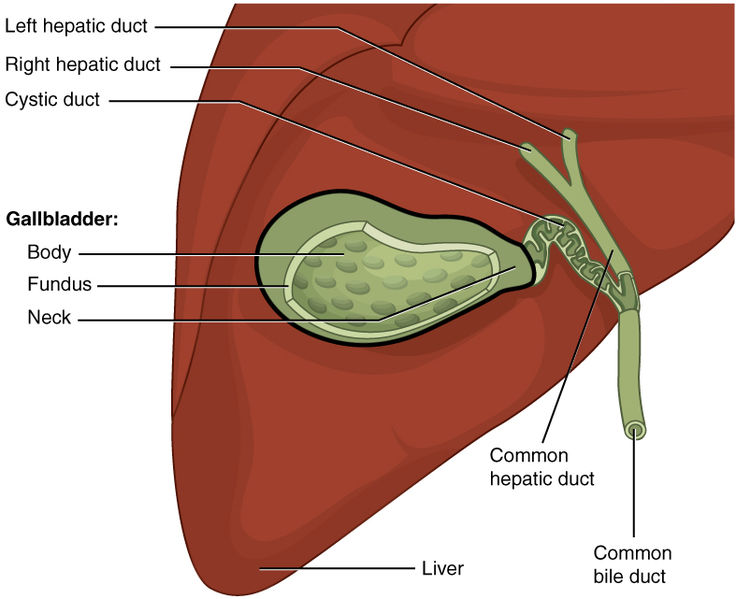
The purpose of the gallbladder is to store and concentrate bile, which is needed to break down fats. In normal digestion, the gallbladder releases bile through the cystic duct when fatty foods are eaten. The bile then travels to the duodenum to help break down fatty foods. This process becomes impaired with cholecystitis.
Cholecystitis can be further classified into two types: calculus and acalculous. Calculus cholecystitis means that a stone is present that is blocking the flow of bile. Although there are various potential locations of gallstones, the cystic duct is a common location. See Figure 11.26[3] for an image of the liver, gallbladder, and associated bile ducts. Gallstones can form from excess bilirubin, cholesterol, or calcium. Gallstones can also form when there is biliary stasis (lack of movement of bile), particularly when bile is very concentrated.[4]
In acalculous cholecystitis, there is no stone formation, but the gallbladder does not contract properly to release bile. Whether bile flow is impaired due to a stone or improper gallbladder contraction, the result is the same. Bile starts to build up, and the gallbladder becomes inflamed and edematous. If this is not treated appropriately and it progresses, the gallbladder can become gangrenous and even rupture.[5]
Assessment
Physical Exam
The most common presenting sign of cholecystitis is pain in the right upper quadrant of the abdomen. Murphy’s sign (pain in the right upper quadrant with palpation) is also a common finding. Some clients may also have pain in the back or shoulder. Other symptoms may include bloating, flatulence, nausea/vomiting, and intolerance to fatty and/or spicy foods.
Common Laboratory and Diagnostic Tests
Lab Tests
Lab tests commonly ordered by health care providers to diagnose cholecystitis are a complete blood count (CBC), a metabolic panel, and lipase levels[6]
- In chronic cholecystitis, a CBC may be normal. However, during acute cases there may be elevated white blood cells.
- A metabolic panel is performed to assess liver function and bilirubin levels. Both liver enzymes and bilirubin levels may be elevated with cholecystitis, particularly when a gallstone is blocking a bile duct.
- A lipase level may also be ordered to rule out pancreatitis. Gallstones can lead to pancreatitis when they become lodged near the pancreatic duct.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Diagnostic Testing
A diagnosis of cholecystitis can be confirmed with a CT scan, ultrasound, or hepatobiliary iminodiacetic acid scan[7]:
- A CT scan can show the presence of gallstones and cholecystitis.
- An ultrasound of the gallbladder can detect gallstones, as well as gallbladder thickening. Gallbladder thickening is commonly seen with cholecystitis.
- A hepatobiliary iminodiacetic acid (HIDA) scan can assess how well the gallbladder is functioning by tracing the flow of bile throughout the gastrointestinal tract using a radioactive tracer. A HIDA scan can also determine the ejection fraction (the amount of bile released with each contraction) of the gallbladder. An ejection fraction of 35% or less indicates acalculous cholecystitis.
Nursing Diagnoses
Nursing priorities for those suffering from cholecystitis include managing pain, preparing the client for surgery if indicated, and ensuring optimal nutrition.
Nursing diagnoses for clients with cholecystitis are created based on the specific needs of the client, their signs and symptoms, and the etiology of the disorder. These nursing diagnoses guide the creation of client specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Possible nursing diagnoses for those with cholecystitis are as follows[8],[9]:
- Acute Pain
- Anxiety
- Deficient Fluid Volume
- Imbalanced Nutrition: Less than Body Requirements
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes for some of the above nursing diagnoses are as follows:
- The client will rate their pain at 3 or less on a scale of 0 to 10 within two hours.
- The client will describe three ways to manage preoperative anxiety after the teaching session.
- The client will exhibit blood pressure and heart rate within normal limits for age, moist mucous membranes, and urine output appropriate for age during their hospital stay.
- The client will achieve a weight within a healthy range according to their height within three months.
Interventions
Medical Interventions
For clients with cholecystitis and gallstones who have minimal symptoms or those who are not surgical candidates, the provider may recommend a conservative approach with a low-fat diet to manage symptoms. However, cholecystitis is generally treated by surgically removing the gallbladder, also known as a cholecystectomy. The preferred approach is laparoscopic removal, but an open approach may be needed in some clients. For clients in which surgery is not a good option, a drain may be placed through the skin into the gallbladder to allow for bile drainage. Another option is to place the client on a medication that can dissolve gallstones, such as ursodiol. Clients with stones in the bile duct may require an ERCP prior to gallbladder removal.[10] For more information on the ERCP procedure, review the “Common Laboratory and/or Diagnostic Tests” subsection of the “General Assessment of the Gastrointestinal System” of this chapter.
Nursing Interventions
For the client with cholecystitis, the following nursing interventions can be divided into nursing assessments, nursing actions, and client teaching.[11]
Nursing Assessments
- Assess vital signs as changes in vitals could indicate that a complication is occurring.
- Complete focused abdominal assessments, noting abdominal pain, nausea, and/or vomiting.
Nursing Actions
- Complete a preoperative checklist when preparing the client for a cholecystectomy. To review information on preoperative checklists and preparing a client for surgery, visit the “Perioperative Care” chapter.
- Administer IV fluids and pain medications as ordered by the provider.
Client Teaching
- Remain on a low-fat diet prior to surgery and during the initial postoperative period. After the gallbladder is removed, fat breakdown does not occur as quickly, and, therefore, fatty foods may cause gastrointestinal upset. With time, the liver will increase bile production, and these symptoms should improve.
- Report symptoms of jaundice (yellow eyes, light-colored stools, and dark urine) as this can indicate the presence of remaining gallstones or other complications. See Figure 11.27[12] for an image of a client with scleral icterus (yellowing of the eyes).
- Educate the postoperative client about shoulder pain. Right shoulder pain is common after a laparoscopic cholecystectomy due to the insertion of carbon dioxide during the surgery. Walking will help reduce the pain. Shoulder pain should completely resolve within two to three days after the surgery. Monitor the incision/dressing daily and notify the provider of any signs of infection (redness, warmth, drainage, increasing pain, or fever). Teach how to self-manage wound care as indicated.

Evaluation
Evaluation of client outcomes refers to the process of determining whether or not client outcomes were met by the indicated time frame. This is done by reevaluating the client as a whole and determining if their outcomes have been met, partially met, or not met. If the client outcomes were not met in their entirety, the care plan should be revised and reimplemented. Evaluation of outcomes should occur each time the nurse assesses the client, examines new laboratory or diagnostic data, or interacts with another member of the client’s interdisciplinary team.
![]() RN Recap: Cholecystitis
RN Recap: Cholecystitis
View a brief YouTube video overview of cholecystitis[13]:
- “Gallstones.JPG” by Alex Khimich (talk) is in the Public Domain ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- “2425_Gallbladder.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2020). Nursing diagnoses: Definitions and classification, 2021-2023 (12th ed.). Thieme. ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- Jones, M. W., Genova, R., & O'Rourke, M.C. (2023). Acute Cholecystitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459171/ ↵
- “Scleral_Icterus.jpg” by Sheila J. Toro is licensed under CC BY 4.0 ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 11 - Cholecystitis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/cTqorDEVA8o?si=77fpCynZluxUr0aD ↵
Inflammation of the gallbladder due to impaired flow of bile due to blockage by gallstones or a poorly functioning gallbladder.
Surgical removal of the gallbladder.

