6.8 Lung Cancer
Overview
Cancer is a disease where cells grow out of control. Lung cancer is a type of cancer that begins in the cells of the lungs. Lung cancer can also be cancer that has spread from other parts of the body called metastasis.
Lung cancer is commonly classified into two main categories called Non-Small Cell Lung Cancer (NSCLC) or Small Cell Lung Cancer (SCLS). Each type grows differently and is treated differently. NSCLC is the most common type of lung cancer, accounting for approximately 85% of all lung cancer cases. NSCLC includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. SCLC is a more aggressive type of cancer, often associated with a high growth rate and earlier metastasis.[1],[2]
Smoking is the greatest risk for lung cancer, but nonsmokers can also have lung cancer. Other risk factors include family history; exposure to secondhand smoke; infection with human immunodeficiency virus (HIV); and exposure to radon gas, radiation, air pollution, and other workplace exposures like asbestos, arsenic, and chromium.[3],[4]
The most common symptoms of lung cancer when it is initially diagnosed include worsening cough, dyspnea, pleuritic chest pain (i.e., worse on deep breathing or coughing), hemoptysis (blood-tinged sputum), malaise, weight loss, and hoarseness.[5]
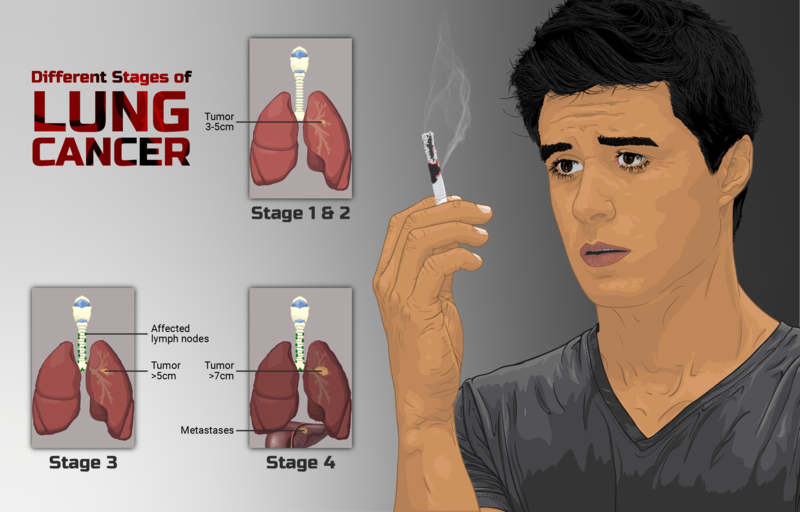
Staging is the process of determining how much cancer is within the body and if it has metastasized. Staging includes the location and size of the tumor, whether the cancer has spread to the lymph nodes, and whether the cancer has spread to the rest of the body. Stage has a critical role in the medical treatment plan. See Figure 6.25[6] for an illustration of the general stages of lung cancer.
Assessment
Early detection and diagnosis are crucial for identifying and managing lung cancer effectively. Clinical manifestations of lung cancer vary depending on the stage and type of lung cancer, as well as the individual’s overall health. See Table 6.8 for a summary of clinical manifestations of lung cancer by body system. Not all individuals with lung cancer will experience all these symptoms. Some symptoms are associated with advanced stages or specific types of lung cancer.
Table 6.8. Clinical Manifestations of Lung Cancer Across Body Systems[7],[8]
| Body System | Clinical Manifestations Across Body Systems |
|---|---|
| Respiratory | Persistent cough, often with hemoptysis, dyspnea, hoarseness or voice changes, recurrent respiratory infections, pleuritic chest pain, and pleural effusion |
| General | Unexplained weight loss, fatigue, weakness, fever, night sweats, and loss of appetite |
| Cardiovascular | Superior vena cava syndrome, a blockage of blood flow into the superior vena cava, often caused by cancer, leading to swelling in the face, neck, or upper chest |
| Nervous | Neurological symptoms, such as severe headache or seizures if cancer has metastasized to the brain |
| Musculoskeletal | Bone pain and fractures if cancer has metastasized to the bones |
| Hepatobiliary | Jaundice (yellowing of the skin and sclera) if cancer has spread to the liver |
| Renal | Hydronephrosis (blockage of the ureters, leading to kidney swelling) if cancer has affected the lymph nodes near the kidneys |
Diagnostic Testing
Diagnostic testing for lung cancer may include a variety of methods to confirm the presence of cancer, determine the type and stage of the cancer, and guide treatment decisions. Common diagnostic tests and procedures for lung cancer include the following[9],[10]:
- Chest X-ray: A chest X-ray is often the initial imaging test used to identify abnormal lung masses or other lung-related issues.
- Computed Tomography (CT) Scan: CT scans provide detailed cross-sectional images of the lungs and are often used to assess the size, location, and extent of lung tumors.
- Positron Emission Tomography (PET) Scan: PET scans help determine if lung cancer has spread to other parts of the body. It involves the injection of a radioactive tracer that is absorbed by fast-growing cells.
- MRI (Magnetic Resonance Imaging): In some cases, an MRI may be used to provide additional information, especially if there are concerns about the involvement of nearby structures.
- Sputum Cytology: Sputum is analyzed under a microscope to check for cancer cells.
- Bronchoscopy: A thin, flexible tube with a light and camera is inserted through the nose or mouth into the airways to collect small tissue samples.
- Biopsy: A biopsy is the definitive diagnostic procedure for lung cancer. There are several ways to obtain tissue samples for analysis:
- Needle Biopsy (Fine Needle Aspiration or Core Biopsy): A thin, hollow needle is used to extract a sample of tissue from the lung, often guided by imaging (CT or ultrasound).
- Surgical Biopsy: In some cases, a surgeon may perform a surgical procedure to remove a larger tissue sample for diagnosis. This may be necessary when other biopsy methods are inconclusive.
- Endobronchial Ultrasound (EBUS): EBUS is a minimally invasive procedure used to obtain tissue samples from lymph nodes and lesions in the chest. It is often performed during bronchoscopy.
If cancer is confirmed, additional tests are performed to determine the stage of the cancer and whether the cancer has spread to distant organs.
Nursing Diagnoses
Nursing diagnoses for clients with lung cancer focus on addressing the unique challenges and needs associated with this condition. The nursing priorities are centered around providing comprehensive care, managing symptoms, and enhancing the client’s overall well-being while preventing complications.
Common nursing diagnoses for clients with cancer include the following[11]:
- Impaired Gas Exchange
- Decreased Activity Tolerance
- Disturbed Body Image
- Fear
- Imbalanced Nutrition: Less Than Body Requirements
- Powerlessness
- Risk for Spiritual Distress
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to lung cancer are as follow:
- The client will maintain oxygen saturation within the prescribed target range (e.g., greater than 92%).
- The client will report decreased pain, at or below a level they have reported as “acceptable.”
- The client will maintain an effective breathing pattern with a respiratory rate below 20 breaths per minute.
- The client will verbalize three positive coping strategies before discharge from the hospital.
Interventions
Medical Interventions
Medical interventions for lung cancer vary based on the type and stage of cancer, as well as the client’s overall health. These interventions aim to diagnose, treat, manage, and support clients with lung cancer and include surgical interventions, radiation therapy, chemotherapy, immunotherapy, and palliative or hospice care[12],[13]:
- Surgical Interventions: Surgical interventions may include any of the following procedures:
- Lobectomy: Removal of an entire lobe of the lung.
- Pneumonectomy: Removal of an entire lung.
- Segmentectomy or Wedge Resection: Removal of a portion of the lung.
- Video-Assisted Thoracoscopic Surgery (VATS): A minimally invasive surgical approach for diagnostic and therapeutic purposes.
- Chest Wall Resection: Involves removing parts of the chest wall if the cancer has spread.
- Radiation Therapy: Radiation therapy may be used to shrink or destroy cancer cells.
- External Beam Radiation: Delivers targeted radiation to the tumor to shrink or destroy cancer cells.
- Brachytherapy: Delivers internal radiation using implanted radioactive sources.
- Stereotactic Radiosurgery (SRS): Precisely targets small tumors with high-dose radiation.
- Chemotherapy: Chemotherapy is used to treat cancer or prevent its spread.
- Systemic Chemotherapy: Administered orally or intravenously to treat cancer that has spread to other areas.
- Adjuvant Chemotherapy: Given after surgery to reduce the risk of cancer recurrence.
- Immunotherapy: Immunotherapy enhances the immune system’s ability to recognize and attack cancer cells, using medications like checkpoint inhibitors (e.g., PD-1 or PD-L1 inhibitors).
- Palliative and Hospice Care: Palliative and hospice care focuses on relieving symptoms, improving quality of life, managing pain and breathlessness, and other side effects. Palliative care may be prescribed any time after diagnosis to address comfort, symptom management, and support. Hospice care is available for clients with advanced or terminal lung cancer whose life expectancy is six months or less.
Nursing Interventions
Nursing interventions focus on symptom management and emotional support to promote overall well-being.
Medication Management
Specially trained oncology nurses administer chemotherapy, but all nurses administer prescribed medications for symptom control and monitor for side effects.
Pain Management
Nurses help manage the client’s pain and other discomfort through pharmacological and nonpharmacological interventions, based on the client’s preferences.
Dyspnea Management
Nurses monitor the client’s level of dyspnea and provide strategies to manage shortness of breath, such as coughing and breathing techniques, positioning, and oxygen therapy. Review enhanced breathing and coughing techniques in the “General Nursing Interventions Related to Respiratory Alterations” subsection earlier in this chapter.
Energy Management
Nurses teach clients to use energy conservation techniques to manage fatigue associated with the disease process, medical interventions, and medications.
Review energy management techniques in the “Anemia” section of the “Hematological Alterations” chapter.
Psychosocial Support
Emotional distress commonly occurs in clients diagnosed with cancer and their family members. Side effects and adverse effects associated with the disease and medical treatments can compound this emotional distress. Most people experience feelings of grief and loss when cancer is diagnosed. They may experience spiritual distress with a common question being, “Why me?” Nurses can play an important role in helping clients find spiritual support and a feeling of hope, even in the midst of terminal cancer.
Nurses offer emotional support, empathy, and active listening to help clients and their family members cope with feelings resulting from the diagnosis, treatment, and resulting changes in role performance. Information is reinforced on medical treatments, as well as on available resources, counseling, and support groups. Nurses assess for signs of anxiety and depression and refer clients and family members to counseling as needed. Relaxation techniques and mindfulness practices are encouraged as positive coping strategies. Palliative care services are offered to manage symptoms, relieve pain, and enhance the client’s quality of life. Nurses also initiate discussions about advance care planning and end-of-life preferences with clients and their family members.
Read more about palliative care, the loss/grief response, and end-of-life care in the “Grief and Loss” chapter of Open RN Nursing Fundamentals, 2e. Read more about the nursing role in spiritual care in the “Spirituality” chapter of Open RN Nursing Fundamentals, 2e.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Lung Cancer
RN Recap: Lung Cancer
View a brief YouTube video overview of lung cancer[14]:
- Centers for Disease Control and Prevention. (2023). What is lung cancer? https://www.cdc.gov/lung-cancer/about/ ↵
- Thomas, K. W., Gould, M., K., & Naeger, D. (2023). Overview of the initial evaluation, diagnosis, and staging of patients with suspected lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Centers for Disease Control and Prevention. (2023). What is lung cancer? https://www.cdc.gov/lung-cancer/about/ ↵
- Thomas, K. W., Gould, M., K., & Naeger, D. (2023). Overview of the initial evaluation, diagnosis, and staging of patients with suspected lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Centers for Disease Control and Prevention. (2023). What is lung cancer? https://www.cdc.gov/lung-cancer/about/ ↵
- “Depiction_of_a_person_smoking_and_stages_of_Lung_Cancer.png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- Thomas, K. W., Gould, M., K., & Naeger, D. (2023). Overview of the initial evaluation, diagnosis, and staging of patients with suspected lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Midthun, D. E. (2022). Clinical manifestations of lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Thomas, K. W., Gould, M., K., & Naeger, D. (2023). Overview of the initial evaluation, diagnosis, and staging of patients with suspected lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Midthun, D. E. (2022). Clinical manifestations of lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Thomas, K. W., Gould, M., K., & Naeger, D. (2023). Overview of the initial evaluation, diagnosis, and staging of patients with suspected lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Midthun, D. E. (2022). Clinical manifestations of lung cancer. UpToDate. https://www.uptodate.com/ ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 6 - Lung cancer [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/GJl_bdFDL0k?si=byMSu9Dnj4C4ZlVM ↵
Compression of the superior vena cava by a cancerous tumor.

