20.5 Wound Dressings
Wound dressings should be selected based on the type of the wound, the cause of the wound, and the characteristics of the wound. A specially trained wound care nurse should be consulted, when possible, for appropriate selection of dressings for chronic wounds. See Table 20.5 for commonly used wound dressings and associated nursing considerations.[1] See additional information about many types of wound dressings in Appendix B – Wound Dressings, including indications and instructions for use.
Table 20.5 Wound Dressings[2]
| Type of Dressing | Description | Nursing Considerations |
|---|---|---|
| Sterile gauze
(see Figure 20.22[3]) Kerlix (see Figure 20.23[4])
|
Can be used as a primary dressing or moistened wound packing. |
|
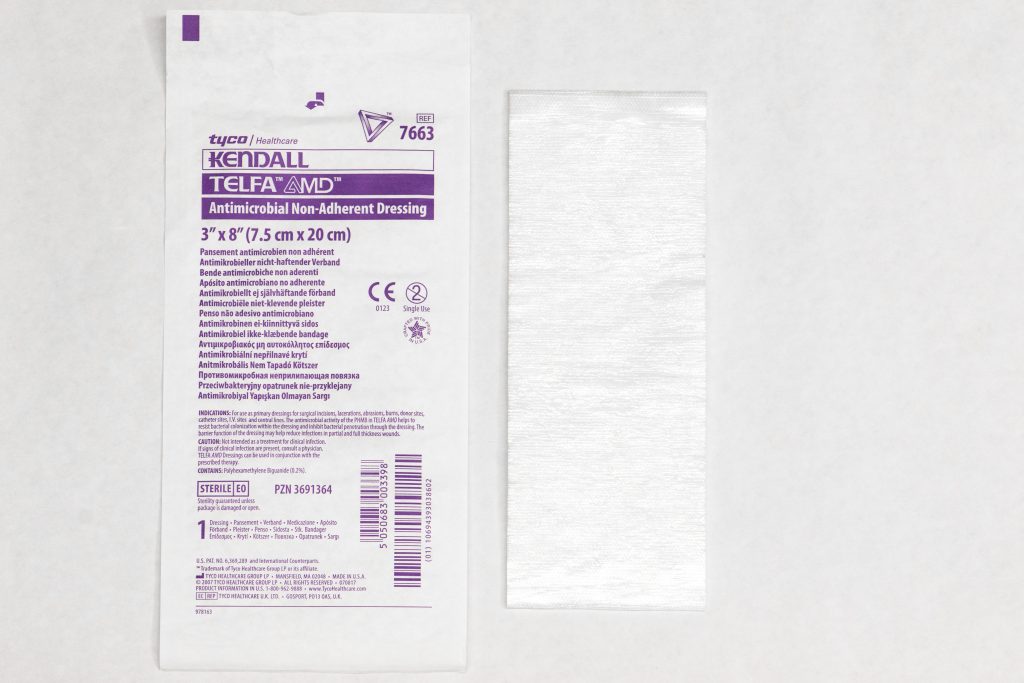
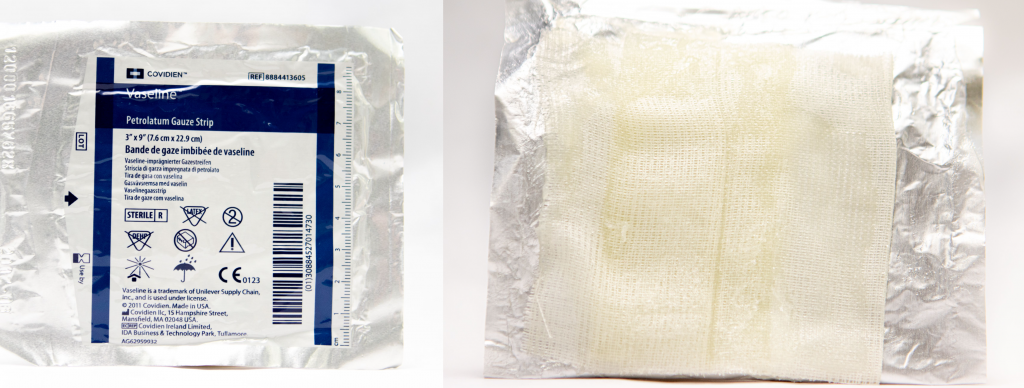
| Nonadherent dressings, nonadherent gauze, or petroleum impregnated gauze
Nonadherent dressing (see Figure 20.24[5]) Petroleum impregnated gauze (see Figure 20.25[6])
|
Applied over open wounds and covered with a secondary dressing. Nontraumatic to skin and wound base. May be applied over skin tears. |
|
| Transparent films
(see Figure 20.26[7])
|
Can be used on wounds with minimal or no exudate to retain moisture. Commonly used to secure other dressing materials such as foam. |
|
| Hydrocolloids
(see Figure 20.27[8])
|
Used as an occlusive dressing to prevent contaminants, promote a moist wound environment, and cause autolytic debridement. Thicker hydrocolloids absorb moderate amounts of drainage. |
|
| Hydrogels
|
Creates a moist wound environment in wounds with little or no exudate. If in gel form, apply directly to the wound and cover with secondary dressing. |
|
| Silicone-based dressings
|
Nonadherent dressing used on moderately to highly exudative wounds. Nontraumatic to wound bed and promotes a moist wound environment. |
|
| Foam
(see Figure 20.28[9]) |
Nonadherent and absorptive. |
|
| Alginate/hydrofibers
(see Figure 20.29[10]) |
Nonadherent and highly absorptive for highly exudative wounds. Used for wound packing in full-thickness wounds such as Stage 3 or 4 pressure injuries. |
|


![]"Hydrocolloid.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 Photo showing hydrocolloid and packaging](https://wtcs.pressbooks.pub/app/uploads/sites/29/2020/11/Hydrocolloid-1024x683.jpg)

![]"Foam Dressing 3I3A0406.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 Photo showing foam dressing and packaging](https://wtcs.pressbooks.pub/app/uploads/sites/29/2020/11/Foam-Dressing-3I3A0406-1024x683.jpg)
!["Alginate Dressing 3I3A0396.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0[/footnote] Photo showing alginate dressing and packaging](https://wtcs.pressbooks.pub/app/uploads/sites/29/2020/11/Alginate-Dressing-3I3A0396-1024x683.jpg)
Types of Tape
There are several types of tape that can be used to secure dressings. The most commonly used types of tape are medical transpore, micropore paper, cloth, and waterproof tape.
- Medical transpore tape (often referred to as “medi-pore”) is inexpensive, durable, and very sticky. It has tiny holes in it that allow air to reach the skin underneath and sweat and body fluid to pass through it without causing it to come off. However, it leaves residue and can damage sensitive skin.
- Micropore paper tape is gentle on skin and doesn’t leave residue, but it is not waterproof and doesn’t work well on irregular areas. It allows air to reach the skin underneath.
- Cloth tape sticks well, allows air to reach the skin, and does not leave a residue. It has high strength so it can be used to secure a splint. However, it is not flexible or waterproof and can be difficult to tear.
- Waterproof tape is more expensive, but it is flexible and doesn’t leave residue. It sticks well to skin but does not stick well to hair. It is waterproof when applied to dry skin.
Read Inside First Aid’s 5 Different Types of Medical Tapes and How to Use Them webpage about different types of medical tape.
Wound Vacs
The term wound vac refers to a device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing. During a wound vac procedure, the nurse applies a special foam dressing over an open wound and seals it with a thin film layer. The film has an opening that rubber tubing fits through to connect to a vacuum pump. Once connected, the vacuum pump removes fluid from the wound while also helping to pull the edges of the wound together. A person with a wound vac typically wears the device 24 hours a day while the wound is healing.[11] See Figure 20.30[12] for an image of a wound vac foam dressing attached to suctioning by a wound vac device. Figure 20.31[13] demonstrates the progression of a wound healing with a wound vac from image A to D.

- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Sterile 4x4 Dressing and Package 3I3A0330.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Kerlix with Package 3I3A0365.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Nonadherent Dressing and Packaging 3I3A0203.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Vaseline Gauze Package -1 3I3A0296.jpg” and “Vaseline Gauze Dressing 3I3A0299” by Deanna Hoyord, Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- “Transparent Film.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Hydrocolloid.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Foam Dressing 3I3A0406.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Alginate Dressing 3I3A0396.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Yetman, D. (2020, March 23). What you need to know about vacuum-assisted wound closure (VAC). Healthline. https://www.healthline.com/health/wound-vac#how-it-works ↵
- “KCI Wound Vac01.jpg” and “KCI Wound Vac02.jpg” by Noles1984 at English Wikipedia are in the Public Domain. ↵
- “0100-6991-rcbc-44-01-00081-gf1.gif” by unknown is licensed under CC BY 4.0. Access for free at https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-69912017000100081#f1 ↵
A device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing.

