8.4 Fertilization, Pregnancy, Labor, Delivery, Newborn Care, and Postpartum Care
Fertilization
There are two types of gametes involved in reproduction: the male gametes, called sperm, and female gametes, called ova. The male gametes are produced in the testes through a process called spermatogenesis, which begins at about 12 years of age. The female gametes are present at birth but are immature. They are stored in the ovaries until puberty, when one ovum ripens and is released about every 28 days in a process called oogenesis (ō-ŏ-JEN-ĕ-sĭs).[1]
After the ovum is released from the ovary, it is drawn into the Fallopian tube. If sexual intercourse occurs, millions of sperm are ejaculated into the vagina, but only a few reach the ovum. Fertilization (fĕr-tĭ-lĪ-zā-shŏn) occurs when a sperm and an ovum combine, also referred to as conception (kŏn-SEP-shŏn). See Figure 8.1[2] for an image of conception.

After a single sperm has entered the ovum, the wall of the ovum becomes hard and prevents other sperm from entering. The head of the sperm, containing the genetic information from the father, unites with the nucleus of the ovum, and a new cell is formed. Reproductive cells are haploid cells containing half of the genetic material needed to form a human being, so their combination forms a diploid cell called a zygote (ZĪ-gōt).[3]
During the first week after conception, the zygote divides and multiplies, going from a one-cell structure to two cells, then four cells, then eight cells, and so on. This process of cell division is called mitosis (mī-TŌ-sĭs). The zygote continues to divide and travel through the Fallopian tube for about 7-10 days, at which point it arrives in the uterus. Once in the uterus, the zygote implants itself in the endometrium (en-dō-MĒ-trē-ŭm), the inner lining of the uterus, where the embryonic stage begins about three weeks after conception.[4]
Human chorionic gonadotropin (hū-MĂN kor-ē-ON-ĭk gō-năd-ō-TRO-pin) is a hormone produced by cells that will eventually make up the placenta in the early stages of pregnancy. HCG can be detected by a blood pregnancy test at around 7-12 days after conception and by a urine pregnancy test about two weeks after conception. HCG increases quickly (almost doubling every three days) for the first eight to ten weeks of pregnancy.[5]
View the following YouTube video[6] illustrating conception: Fertilization
Embryonic Stage
An embryo (EM-brē-ō) is an organism in its early stages of development, specifically from Day 16 through Week 8. See Figure 8.2[7] for an image of a human embryo.

During the embryonic stage, blood vessels grow, forming the placenta. The placenta (plă-SEN-tă) is a structure that connects the fetus to the uterus, providing oxygen and nutrients from the mother to the developing embryo via the umbilical cord (ŭm-BĬL-ĭ-kăl kŏrd). Basic structures of the embryo start to develop into areas that will become the head, chest, and abdomen. During the embryonic stage, the heart begins to beat, and organs form and begin to function. At 22 days after conception, the neural tube forms along the back of the embryo, developing into the spinal cord and brain.[8]
About 20 percent of embryos do not successfully make it through the embryonic stage, usually due to chromosomal abnormalities. It is during this stage that the major structures of the body are forming, making the embryonic period a vulnerable time if the embryo is exposed to a harmful substance. Teratogens (tĕr-AT-ŏ-jĕnz), agents that cause malformations in a developing embryo, include alcohol, drugs, diseases, chemicals, and environmental exposures. Many mothers are not aware they are pregnant during the embryonic period, further increasing the risk of teratogen exposure to the developing embryo.[9]
Fetal Stage
When the embryo is about nine weeks old until birth, it is called a fetus (FĒ-tŭs). At the beginning of this stage, the fetus is about the size of a kidney bean and begins to take on the recognizable form of a human being. See Figure 8.3[10] for an image of an early fetus.

Mothers experience quickening (KWĬK-ĕn-ĭng), the first feeling of movement of the fetus in utero, around 16 to 20 weeks. By the time the fetus reaches the sixth month of development (23-24 weeks), it weighs up to 1.4 pounds. Hearing has developed, so the fetus can respond to sounds. The internal organs, such as the lungs, heart, stomach, and intestines, have formed enough that a fetus born prematurely at this point has a chance of survival with intensive medical care.
Between the seventh and ninth months, the fetus is primarily preparing for birth. It is exercising its muscles, and its lungs begin to expand and contract. Around 36 weeks, the fetus is almost ready for birth. It weighs about six pounds and is about 18.5 inches long. By Week 37 all organ systems are developed enough that the fetus could survive outside the mother’s uterus without many of the risks associated with premature birth. The fetus continues to gain weight and grow in length until approximately 40 weeks. See Figure 8.4[11] for an illustration of fetal growth.[12]

View the following TED Talk video[13] showing human development from conception on: Conception to Birth – Visualized
Pregnancy
A full-term pregnancy lasts approximately 270 days (approximately 38.5 weeks) from conception to birth. Because it is easier to remember the first day of the last menstrual period (last MEN-strū-ăl PĒ-rē-ŏd) (LMP) than to estimate the date of conception, obstetricians set the due date as 284 days (approximately 40.5 weeks) from the LMP. This assumes that conception occurred on Day 14 of the woman’s cycle. These 40 weeks of pregnancy are usually discussed in terms of three trimesters (TRĪ-mĕs-tĕrz), each trimester lasting approximately 13 weeks.
During the first trimester, it is common for the mother to experience nausea as a result of higher levels of estrogen in her body, commonly called “morning sickness.” Other symptoms during pregnancy may include heartburn, gas, hemorrhoids, backache, leg cramps, insomnia, constipation, and varicose veins.[14] See Figure 8.5[15] for an image of a pregnant woman.
Labor and Delivery
The process of childbirth, referred to as labor and delivery, is divided into three stages:
- First Stage: Cervical dilation
- Second Stage: Expulsion or birth
- Third Stage: Delivery of the placenta
See Figure 8.6[16] for an illustration of childbirth.
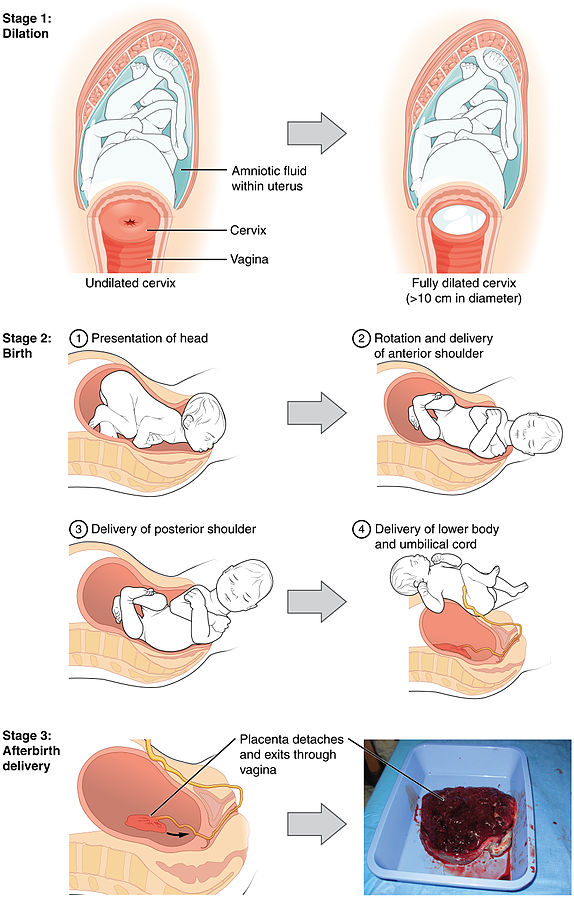
First Stage: Cervical Dilation
The first stage of labor begins with uterine contractions that initially last about 30 seconds and are spaced 15 to 20 minutes apart. Uterine contractions are the rhythmic tightening and shortening of the uterine muscles during labor. These contractions increase in duration and frequency to more than a minute long and three to four minutes apart. Women are typically advised to go to the hospital for delivery when contractions are coming about every five minutes. Some women experience Braxton-Hicks (BRAX-tŏn HIKS) contractions, which are irregular false contractions that occur before actual labor begins. Women are counseled that real labor pains typically increase with walking, resulting in the cessation of walking until the contraction stops. Labor may also begin with clear or pink-tinged mucus discharge (called a mucus plug) or a gush of amniotic fluid.[17]
During labor, the cervix dilates to ten centimeters (just under four inches) so it is wide enough to deliver the newborn’s head. Dilation may take around 12-16 hours for woman delivering their first child or about 6-9 hours for women who have previously given birth. However, labor varies widely among women and may take over 24 hours. In each subsequent labor, the labor stage tends to be shorter.[18]
Second Stage: Expulsion or Birth
The second stage involves the passage of the baby through the birth canal. Parturition (păr-tū-RĬSH-ŭn) is a medical term for the act of giving birth. This stage takes about 10-40 minutes. Contractions usually come about every 2-3 minutes, and the mother pushes and relaxes as directed by the medical staff.
Normally, the head of the baby emerges first, referred to as a cephalic presentation (sĕ-FAL-ĭk prē-zen-TĀ-shŏn). Crowning (KROWN-ĭng) refers to the appearance of the baby’s head at the vaginal opening.
The baby’s head is turned when it is in the head-down position, referred to as cephalic version (sĕ-FAL-ĭk VĔR-zhŏn), so that one shoulder can emerge, followed by the other shoulder. The rest of the baby quickly passes through, and then the umbilical cord is clamped and cut.[19]
In some cases, the baby is not in a head-down position during labor and delivery. Breech (brēch) refers to a feet-first position that requires additional interventions by medical staff and perhaps delivery by cesarean section.
Third Stage: Delivery of Placenta
The third stage is relatively painless in comparison to the other stages. During this stage, the placenta is delivered. This typically occurs within 20 minutes after delivery of the baby.[20] Following delivery, if the mother experienced tearing of the perineum, it is repaired by the obstetrician or midwife. The perineum (pĕr-ĭ-NĒ-ŭm) is the area between the vagina and the anus. An episiotomy (ĕp-ĭ-zē-OT-ŏ-mē) is a surgical incision of the vulva to widen the vaginal opening to prevent ripping or tearing of the perineum during delivery.
View the following YouTube video[21] on childbirth: Patient Education Animation: Labor and Vaginal Birth
Cesarean Section
Cesarean section (si-ZAR-ē-ăn SEK-shŏn), also known as C-section, is delivery of the fetus through an abdominal incision made by the obstetrician. Cesarean sections are performed when a vaginal delivery would put the baby or mother at risk. Common reasons for C-sections include obstructed labor based on the shape of the mother’s pelvis, breech presentation of the baby, complications with the placenta or umbilical cord, twin pregnancy, or high blood pressure in the mother.[22]
Newborn Assessment
The average newborn weighs approximately 7.5 pounds. In the minutes following birth, a newborn must undergo dramatic body system changes to be able to survive outside the womb. The Apgar score (AP-gar skōr) is an evaluation of a newborn’s physical condition within one to five minutes after birth and was developed by and named for Virginia Apgar (making this an eponym).
The technique for determining an Apgar score is quick, easy, painless, and does not require any instruments except for a stethoscope. A convenient way to remember the five scoring criteria is to apply the mnemonic APGAR[23]:
- Appearance (skin color)
- Pulse (heart rate)
- Grimace (reflex)
- Activity (muscle tone)
- Respiration
Skin color, heart rate, reflex, muscle tone, and respiration are assessed, and each criterion is assigned a score of 0, 1, or 2. Scores are taken at one minute after birth and again at five minutes after birth. After each time the scores are taken, the five scores are added together. High scores (out of a possible 10) indicate the baby has made the transition well, whereas lower scores indicate that the baby may be in distress. See Figure 8.7[24] for APGAR criteria.[25]
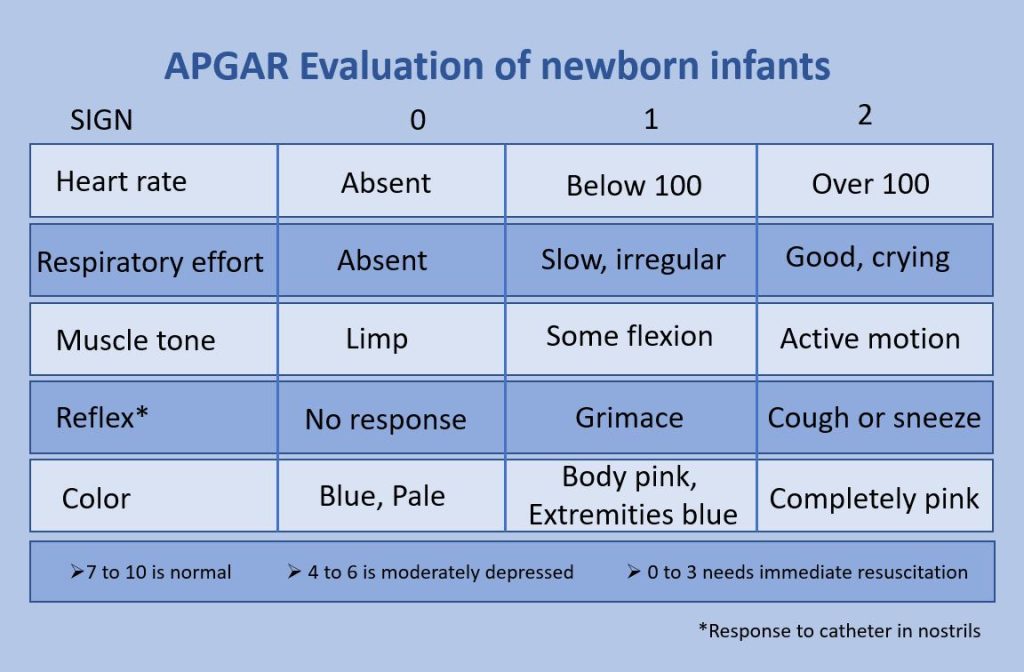
Of the five Apgar criteria, heart rate and respiration are the most critical. Poor scores for either of these measurements may indicate the need for immediate medical attention to resuscitate or stabilize the newborn. In general, any score lower than 7 at the five-minute mark indicates that medical assistance may be needed. A total score below 5 indicates an emergency situation. Normally, a newborn will get an intermediate score of 1 for some of the Apgar criteria and will progress to a 2 by the five-minute assessment. Scores of 8 or above are normal.[26]
Many newborns are covered with lanugo (lă-NOO-gō), a fine, downy hair and vernix (VĔR-nĭks), a white, waxy substance covering the skin. Within 24-48 hours of birth, newborns pass their first stool, called meconium (mē-KŌ-nē-ŭm). Meconium is dark, thick, and sticky. Sometimes a fetus passes meconium if they are stressed during labor and delivery. If the fetus inhales meconium into the lungs in utero, it can cause severe respiratory complications. This condition is called meconium aspiration (mĕ-KŌ-nē-ŭm AS-pĭ-RĀ-shŏn).
Postpartum Period
The postpartum (pōst-PÄR-tŭm) period begins immediately after childbirth as the mother’s body, including hormone levels and uterus size, returns to a nonpregnant state. The terms puerperium, puerperal period, or postpartum period are commonly used to refer to the first six weeks following childbirth. During this time, the mother is monitored for bleeding, bowel and bladder function, and baby care. The infant’s health is also monitored, and vaccines are administered. The postpartum period can be divided into three stages[27]:
- Acute phase: Six to 12 hours after childbirth
- Subacute postpartum period: Two to six weeks after childbirth
- Delayed postpartum period, which can last up to six months.
Acute Phase
The first 6 to 12 hours after childbirth is the initial or acute phase of the postpartum period. During this time the mother is monitored by nurses or midwives for potential complications such as postpartum hemorrhage. Immediately after childbirth, the infant is placed directly on the mother’s chest whenever possible. See Figure 8.8[28] for an image of chest-to-chest positioning of the mother and infant.[29]

The greatest health risk during the acute phase is postpartum bleeding. Following delivery, the area where the placenta was attached to the uterine wall bleeds, and the uterus must contract to prevent blood loss. After contraction takes place, the fundus (top) of the uterus can be palpated as a firm mass at the level of the navel. It is important that the uterus remains firm, and nurses or midwife will make frequent assessments of both the fundus and the amount of bleeding. Uterine massage is commonly used to help the uterus contract and prevent postpartum hemorrhage.[30]
Subacute Postpartum Period
The subacute postpartum period lasts two to six weeks. During this time, lochia (LŌ-kē-ă), vaginal discharge after birth, will turn color from bright red, to brownish, to yellow. It will gradually decrease in amount and cease at around five or six weeks.[31]
At two to four days postpartum, a woman’s breast milk will generally come in and is called lactation (lăk-TĀ-shŏn). Mothers are encouraged to breastfeed their babies every three hours during the day and night. During pregnancy and the first few days after delivery, colostrum (kŏ-LOS-trŭm), a thin, milky fluid, is secreted by the breast. Colostrum is rich in immunoglobulin A (IgA), which helps protect the infant from infection. Colostrum also helps to establish a normal gut microbiome in the infant and further protects against infection. Human colostrum is ideal for newborns and is preferable over formula or milk from other animals.[32]
Approximately 70-80% of postpartum women will experience the “baby blues” for a few days due to the rapid change in hormone levels. However, some women experience more serious clinical depression during pregnancy or after childbirth, referred to as peripartum depression (pĕr-ĭ-PÄR-tŭm di-PRESH-ŭn), also known as postpartum depression. They may feel depressed, anxious, guilty, agitated, or weepy. They may not want to hold or care for their newborn, even in cases in which the pregnancy was desired and intended. Family and friends who recognize these symptoms in a pregnant or postpartum woman should encourage them to see a health care provider for treatment.[33]
Delayed Postpartum Period
The delayed postpartum period starts after the subacute postpartum period and lasts up to six months. During this time, the mother’s muscles and connective tissue return to a pre-pregnancy state. During this period, infant sleeping during the night gradually increases and maternal sleep generally improves.[34]
Other Definitions Related to Obstetrics
- Abortion (ă-BOR-shŏn) (AB): Termination of pregnancy before the fetus is viable. Medically, this term refers to spontaneous miscarriages, as well as elective termination of pregnancy.
- Ectopic pregnancy (ek-TOP-ik PREG-năn-sē): Pregnancy occurring outside the uterus, commonly in the Fallopian tube.
- Gestation (jĕs-TĀ-shŏn): The period of development during pregnancy.
- Gravida (GRĂV-ĭ-dă): A woman who is or has been pregnant, regardless of outcome.
- Induction (in-DŬK-shŏn): A process of bringing on or starting labor through medical interventions such as a membrane sweep and/or the intravenous administration of oxytocin to the mother.
- Multigravida (mŭl-tĭ-GRĂV-ĭ-dă): A woman who has been pregnant two or more times regardless of outcome.
- Multipara (mŭl-TĬP-ă-ră): A woman who has given multiple births to an offspring after 20 weeks, live or stillborn.
- Neonate (NĒ-ō-nāt): An infant from birth to four weeks of age.
- Nulligravida (nŭl-ĭ-GRĂV-ĭ-dă): A woman who has never been pregnant.
- Oligohydramnios (ŏl-ĭg-ō-hī-DRĂM-nē-ōs): Minimal amniotic fluid within the placental sac that can restrict the fetus from movement and growth.
- Oxytocin (ŏk-sē-TŌ-sĭn): A hormone that stimulates contractions during labor and the secretion of milk.
- Para (PĂR-ă): A woman who has given birth to an offspring after 20 weeks, live or stillborn.
- Placenta abruptio (plă-SENT-ā ă-BRŬP-shē-ō): Premature separation of the placenta from the uterine wall.
- Placenta previa (plă-SENT-ā PRĒ-vē-ă): An abnormally low implantation of the placenta on the uterine wall, which can result in hemorrhage. Mothers with placenta previa may require a C-section.
- Prenatal (prē-NĀT-ăl): Pertaining to before birth.
- Stillborn (STIL-bōrn): The birth of an infant who has died in the uterus.
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- “Sperm-egg.jpg” by Unknown author is licensed in the Public Domain. ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- Cleveland Clinic. (2022, March 11). Human chorionic gonadotropin. https://my.clevelandclinic.org/health/treatments/4423-vasectomy ↵
- Nucleus Medical Media. (2013, January 31). Fertilization [Video]. YouTube. All rights reserved. https://youtu.be/_5OvgQW6FG4?si=siTDwkcpfKtYJ9LC ↵
- “9-Week_Human_Embryo_from_Ectopic_Pregnancy.jpg” by Ed Uthman from Houston, TX, USA is licensed under CC BY 2.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- “Human_fetus_10_weeks_with_amniotic_sac_-_therapeutic_abortion.jpg” by suparna sinha is licensed under CC BY-SA 2.0 ↵
- “CNX_Psych_09_02_Stages.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://open.maricopa.edu/devpsych/chapter/chapter-2-genetics-and-prenatal-development/ ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- Tsiaras, A. (2010, December). Conception to birth -- Visualized [Video]. Ted.com. All rights reserved. https://www.ted.com/talks/alexander_tsiaras_conception_to_birth_visualized ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- “PregnantWoman.jpg” by Ken Hammond is licensed in the Public Domain. ↵
- “2920_Stages_of_Childbirth-02.jpg” by OpenStax College is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- Nucleus Medical Media. (2012, August 20). Patient education animation: Labor and vaginal birth [Video]. YouTube. All rights reserved. https://youtu.be/ZDP_ewMDxCo?si=kFvTxtkYvr0TH8Te ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “APGAR_score.jpg” by Dr.Vijaya chandar is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- “Postpartum_baby2.jpg” by Tom Adriaenssen is licensed under CC BY-SA 2.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Jozsa & Thistle and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵

