7.6 Diseases and Disorders of the Female Reproductive System
Abnormal Vaginal Bleeding
Abnormal vaginal bleeding (ăb-nŏr-măl vă-jĭ-năl blēd-ing) refers to very heavy menstrual flow during menses, bleeding between menstrual cycles, or menses that lasts more than seven days. It also refers to bleeding that happens before puberty or after menopause. Very heavy bleeding during menses and/or bleeding that lasts more than seven days is called menorrhagia (mĕn-ō-RĀ-jē-ă). For example, women with menorrhagia may bleed enough to soak through one or more tampons or sanitary pads every hour.[1]
A common cause of abnormal bleeding is hormone imbalance referred to dysfunctional uterine bleeding (dĭs-fŭnk-shŭn-ăl yŪ-tĕr-ĭn blēd-ing). Dysfunctional uterine bleeding commonly occurs in teenagers or women approaching menopause (MEN-ŏ-poz) or the absence of menstruation when an egg is not released from the ovaries as it should (anovulation). Anovulation is a common condition for teenagers who recently started their menstrual cycles, as well as for women approaching menopause. When anovulation occurs, extended estrogen release causes the endometrial lining of the uterus to continue to grow until it gets too thick. When this thickened lining is shed during menstruation, it causes the bleeding to be very heavy. A hormonal imbalance can also cause the body not to know when to shed the lining, causing irregular bleeding (ĭ-rĕg-yŭ-lăr blēd-ing) or “spotting” between periods.[2]
Abnormal vaginal bleeding can also be caused by uterine fibroids (benign growths in the uterus), conditions related to pregnancy, and cancer of the uterus or cervix. Diagnostic testing includes pelvic ultrasounds and procedures such as endometrial biopsy or hysteroscopy. Treatment is based on the cause of the abnormal bleeding and may include medications, dilation and curettage (D&C), endometrial ablation, or hysterectomy.[3] Endometrial ablation (en-dō-MĒ-trē-ăl ă-BLĀ-shŏn) is a procedure that destroys the endometrial lining of the uterus to reduce or stop heavy menstrual bleeding. D&C and hysterectomies are further discussed in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Female Reproductive System” section of this chapter.
Medications and medication-secreting devices used to treat dysfunctional uterine bleeding are birth control pills and intrauterine devices (ĬN-tră-yŪ-tĕr-ēn dī-VĪS-ĭz) (IUDs). An IUD is a small, T-shaped device that typically contains hormones to prevent ovulation and the thickening of endometrial lining and prevent pregnancy. It is inserted through the cervix by a health care provider. Birth control pills contain hormones that prevent pregnancy by preventing the thickening of the endometrial lining. They can also help keep the menstrual cycle regular and reduce cramping during menstruation. However, some types of birth control pills, especially the progestin-only pill, can cause abnormal bleeding.[4]
Cancer
Common cancers affecting the female reproductive system include breast, cervical, ovarian, and endometrial.
Breast Cancer
Breast cancer (brest KAN-sĕr) occurs when breast cells mutate and become cancerous cells that multiply and form tumors. There are different kinds of breast cancer, depending on which cells in the breast turn into cancer. Most breast cancers begin in the ducts (called invasive ductal carcinoma) or lobules (called invasive lobular carcinoma). There are also other kinds of breast cancer. Breast cancer can spread outside the breast to other parts of the body through blood and lymph vessels. When breast cancer spreads to other parts of the body, it is said to have metastasized (mĕ-tăs-tă-sīzd).[5]
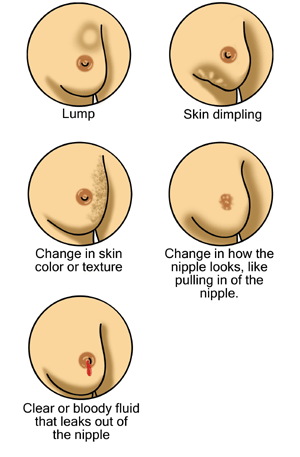
People of both genders who have a strong family history of breast cancer or inherited changes in BRCA1 and BRCA2 genes have a high risk of getting breast cancer. See Figure 7.6[6] for an illustration of signs of breast cancer. Warning signs of breast cancer include the following[7]:
- New lump in the breast or armpit.
- Thickening or swelling of part of the breast.
- Irritation or dimpling of breast skin.
- Redness or flaky skin in the nipple area or the breast.
- Pulling in of the nipple or pain in the nipple area.
- Nipple discharge other than breast milk, including blood.
- Any change in the size or the shape of the breast.
- Pain in any area of the breast.
The American Cancer Society recommends a mammogram every year for most women starting at age 45.[8] A mammogram (MĂM-ō-grăm) is a radiographic image of breast tissue that can detect signs of cancer, often before a lump is felt.
People suspected of having breast cancer or those at high risk may have additional diagnostic tests, such as the following[9]:
- Breast ultrasound (brĕst ŭl-tră-sound): A breast ultrasound uses sound waves to make images, called sonograms, of areas inside the breast.
- Diagnostic mammogram (dī-ăg-nŏs-tĭk mă-mō-grăm): If an area of the breast looks abnormal on a screening mammogram, a diagnostic mammogram is performed to get a more detailed X-ray of the breast.
- Breast magnetic resonance imaging (brĕst măg-NĔT-ĭk rĕz-ŏ-NĂNS ĬM-ă-jĭng) (MRI): A breast MRI is a kind of body scan that uses a magnet linked to a computer. The MRI scan makes detailed pictures of areas inside the breast.
- Biopsy (BĪ-ŏp-sē): Tissue, fluid, and/or lymph nodes are removed by a health care provider and sent to a laboratory to be examined under a microscope. There are different kinds of biopsies, such as a fine-needle aspiration, sentinel lymph node biopsy, core biopsy, or open biopsy.
If breast cancer is diagnosed, other diagnostic tests are performed to check for metastasis, including chest X-rays, CT scans, and PET scans. Read more information about these types of diagnostic tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Respiratory System.”
Breast cancer is treated in several ways, depending on the type of breast cancer and how far it has spread in the body. People with breast cancer often get more than one kind of treatment. Treatments may include the following[10]:
- Surgery (SŬR-jĕr-ē): There are different types of surgery, depending on how far the cancer has spread in the breasts, lymph nodes, and surrounding tissue.
- Breast-conserving surgery (brĕst kŏn-sĕr-vĭng sŭr-jĕr-ē): Breast-conserving surgery removes the cancer and some normal tissue around it, but not the breast itself. This type of surgery may also be called lumpectomy, partial mastectomy, segmental mastectomy, quadrantectomy, or breast-sparing surgery.
- Total mastectomy (tō-tăl mas-TEK-tŏ-mē): Total mastectomy removes the breast that has cancer and some of the lymph nodes in the armpit. This procedure is also called a simple mastectomy.
- Modified radical mastectomy (mŏd-ĭ-fīd răd-ĭ-kăl mas-TEK-tŏ-mē): The whole breast that has cancer and most of the lymph nodes surrounding the breast are removed.
- Chemotherapy (kē-mō-THĔR-ă-pē): Specific medications are prescribed by physicians to shrink or kill specific types of cancer cells. Chemotherapy may be given as pills or administered intravenously, depending on the type of medication prescribed.
- Hormonal therapy (hôr-MŌ-năl THĔR-ă-pē): Special medications are used to block cancer cells from getting the hormones they need to grow.
- Targeted therapy (TĂR-gĭ-tĕd THĔR-ă-pē): Targeted therapy works with the body’s immune system to help it fight cancer cells or to control side effects from other cancer treatments.
- Radiation therapy (rā-dē-Ā-shŏn THĔR-ă-pē): Radiation therapy uses high-energy rays (similar to X-rays) to kill the cancer cells.
Doctors from different specialties often work together to treat breast cancer. Surgeons (SŬR-jŏns) are doctors who perform operations. Medical oncologists (mĕd-ĭ-kăl ŏn-KOL-ŏ-jĭsts) are physicians who specialize in the treatment of cancer with medication. Radiation oncologists (rā-dē-Ā-shŏn ŏn-KOL-ŏ-jĭsts) are physicians who specialize in the treatments of cancer with radiation.
Cervical Cancer
Cervical cancer (SĔR-vi-kăl KAN-sĕr) is mostly caused by the human papillomavirus (HYŪ-măn pă-pĭ-lō-mă VĪ-rŭs) (HPV). HPV is passed from one person to another during sexual contact. HPV causes cervical cells to change into abnormal cells (called dysplasia), which over time can become cancer. Cervical cancer is highly curable when found and treated early. Early cervical cancer does not cause symptoms, so routine PAP smears are recommended to screen for cancer. Most women between the ages of 21 and 65 should have a PAP smear every three to five years, depending upon their risk factors.[11]
The Papanicolaou smear (păp-ă-NĒ-kă-low smēr), commonly referred to as a PAP smear, is a cytological study that screens for cancer in the cervix before symptoms even occur. During a PAP smear, a health care provider inserts a speculum (SPEK-yŭ-lŭm) into the patient’s vagina to allow visualization of the cervix and obtains samples of cervical cells for laboratory analysis. An HPV test (H-P-V tĕst) is also typically performed during a PAP smear to check for infection with high-risk types of HPV that cause cancer.[12]
There are several types of abnormal cells that may be found on PAP smears. For example, low-grade squamous intraepithelial lesions (lō-grād SKWĀ-mŭs ĭn-tră-ĕ-pĭ-THĒ-lē-ăl LĒ-zhŭns) (LSIL) refer to slightly abnormal changes that are usually caused by an HPV infection that require additional diagnostic testing. High-grade squamous intraepithelial lesions (hī-grād SKWĀ-mŭs ĭn-tră-ĕ-pĭ-THĒ-lē-ăl LĒ-zhŭns) (HSIL) refer to abnormal cervical cells that could become cancer if not treated. Adenocarcinoma in situ (ăd-ĕ-nō-kăr-sĭ-NŌ-mă ĭn SĪ-tū) means an advanced lesion (i.e., area of abnormal tissue) was found in the tissue of the cervix and requires a biopsy.[13]
Additional diagnostic testing, such as a colposcopy, is performed for abnormal cell changes on PAP smears. A colposcopy (kŏl-PŎS-kō-pē) is a procedure in which a lighted, magnifying instrument called a colposcope is used to visually examine the cervix and potentially remove tissue for biopsy.[14]
Treatment for cervical cancers often includes excisional or ablative treatments[15]:
- Cold knife conization (kŏn-Ī-ZĀ-shŏn): A scalpel or laser knife is used to remove a cone-shaped section of abnormal tissue in the cervix. This procedure is done at the hospital and requires general anesthesia.
- Loop electrosurgical excision procedure (lōōp ĕ-lĕk-trō-SŬR-jĭ-kăl ĕk-SĬZ-shŭn prō-SĒ-jŭr) (LEEP): Electrical current is passed through a thin wire loop to remove abnormal tissue in the cervix. Local anesthesia is used to numb the area, so this procedure can be performed in the health care provider’s office.
- Cryotherapy (krī-ō-THĔR-ă-pē): A special cold probe is used to destroy abnormal tissue by freezing it. This procedure is done in the health care provider’s office. It takes only a few minutes and usually does not require anesthesia.
- Laser therapy (LĀ-zĕr THĔR-ă-pē): A laser (narrow beam of intense light) is used to destroy abnormal tissue. This procedure is done at the hospital, and general anesthesia is used.
Endometrial Cancer
The most common type of uterine cancer is endometrial cancer (en-dō-MĒ-trē-ăl KAN-sĕr). A common symptom of endometrial cancer is postmenopausal vaginal bleeding.[16]
Diagnostic testing for endometrial cancer includes a transvaginal ultrasound and endometrial sampling. Endometrial sampling (ĕn-dō-MĒ-trē-ăl săm-plĭng) is the removal of tissue from the endometrium by a health care provider who inserts a brush, curette, or thin, flexible tube through the cervix and into the uterus. The tool is used to gently scrape a small amount of tissue from the endometrium and then remove the tissue samples. A pathologist views the tissue under a microscope to look for cancer cells. Alternatively, dilation and curettage (D&C) or hysteroscopy may be performed.[17] Read more information about D&C and hysteroscopy procedures in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Female Reproductive System” section.
If endometrial cancer is diagnosed, additional diagnostic tests are performed to see if the cancer has spread to other parts of the body, including chest X-rays, CT scans, MRIs, and PET scans. Read more information about these types of diagnostic tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Respiratory System.
Treatment for endometrial cancer may include surgery, such as a hysterectomy, bilateral oophorectomy, and lymph node dissection. Hysterectomy and oophorectomy are discussed in more detail in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Female Reproductive System” section. A lymph node dissection (lĭmf nōd dĭ-sĕk-shŏn) is a surgical procedure in which the lymph nodes are removed from the pelvic area, and a sample of tissue is examined under a microscope by a pathologist for signs of metastatic cancer. This procedure is also called lymphadenectomy (lĭmf-ăd-ĕ-NEK-tŏ-mē). Other treatments include radiation therapy, chemotherapy, hormone therapy, and targeted therapy.[18]
Ovarian Cancer
Ovarian cancer (ō-VAR-ē-ăn KAN-sĕr) is cancer that grows in the tissues of the ovary. Ovarian cancer has few symptoms other than possible pain and/or swelling in the pelvic area, so it often metastasizes before it is diagnosed. Some types of ovarian cancer are caused by mutations in genes called BRCA1 or BRCA2, so women who have a family history of ovarian cancer are at an increased risk. Other types of ovarian cancer are caused by metastatic cancer from other sites, such as breast, cervical, or colon cancer. Some women who have an increased risk of ovarian cancer may choose to have an oophorectomy to remove healthy ovaries as a preventative measure.[19]
Diagnostic tests for ovarian cancer include blood tests, a transvaginal ultrasound, or CT scans. After ovarian cancer has been diagnosed, additional diagnostic tests, such as an MRI or PET scans, are done to determine if cancer cells have spread within the ovaries or to other parts of the body. Treatment may include surgery, such as a hysterectomy, salpingo-oophorectomy, or omentectomy. Hysterectomy, salpingo-oophorectomy, and oophorectomy procedures are discussed in more detail in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Female Reproductive System” section. An omentectomy (ō-mĕn-TEK-tŏ-mē) is removal of tissue in the peritoneum that contains blood vessels, nerves, lymph vessels, and lymph nodes. The peritoneum (pĕr-ĭ-tō-NĒ-ŭm) is the tissue that lines the abdominal wall and covers most of the organs in the abdomen. Additional treatments may include chemotherapy, targeted therapy, radiation therapy, and immunotherapy.[20]
Endometriosis
Endometriosis (en-dō-mē-trē-Ō-sĭs) is a disorder in which tissue similar to the endometrium grows outside the uterus, typically on the ovaries, in Fallopian tubes, and in the pelvis. Estrogen causes these implants to thicken, bleed, and break down during menstrual cycles. Because there is no way for the blood to exit the body, surrounding tissue becomes inflamed and creates scar tissue, which can interfere with the normal functioning of nearby organs and cause pain. Endometriosis can also cause infertility if the ovaries are affected.[21] See Figure 7.7[22] for an illustration of endometriosis.
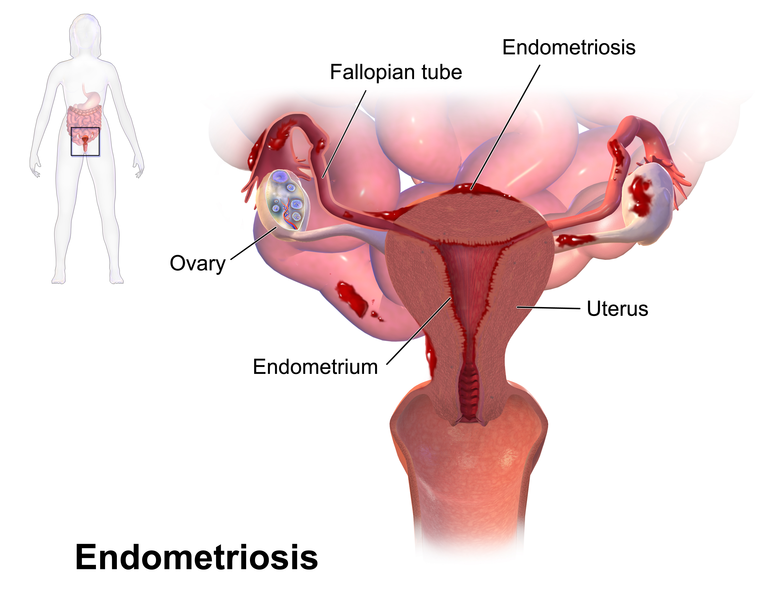
Symptoms of endometriosis include dysmenorrhea (dĭs-mĕn-ŏ-RĒ-ă) or painful menstruation for several days that may include low back and abdominal pain. Dysparenuria (dĭs-păr-ĕn-ŪR-ē-ă) or pain with intercourse is common, as well as pain with bowel movements or urination. Excessive bleeding or bleeding between menstruation may occur.[23]
Endometriosis may be diagnosed with a transvaginal ultrasound or a laparoscopy. During a laparoscopy (lăp-ă-RŎS-kŏ-pē), the patient is under general anesthesia, and a surgeon makes a tiny incision near the navel and inserts a laparoscope, looking for signs of endometrial tissue outside the uterus. A laparoscopy can be performed to provide information about the location, extent, and size of endometrial implants, as well as remove them for biopsy. In severe cases of endometriosis, an oophorectomy (removal of an ovary) or a hysterectomy may be required.[24]
Menopause
Menopause (MEN-ŏ-poz), the cessation of menstruation, is part of the normal aging process and typically occurs in the 40s or 50s. A woman has reached menopause when she has not had a period for one year. Menopause occurs because the woman’s ovaries stop producing the hormones estrogen and progesterone. Menopause can also be triggered by surgical removal of the ovaries because of their role in producing these hormones.
Many women experience symptoms for many years before menopause[25]:
- A change in menses, such as shorter or longer menses, lighter or heavier menstrual flow, or more or less time between menstrual cycles
- Hot flashes and/or night sweats
- Trouble sleeping
- Vaginal dryness
- Bladder incontinence
- Mood swings
- Trouble focusing
- Less hair on head and more on face
For some women, menopausal symptoms can be severe and disruptive, requiring treatment by a health care provider.
Ovarian Cyst
An ovarian cyst (ō-VĀR-ē-an sĭst) is a fluid-filled sac in the ovary. The two most common types of ovarian cysts are follicle cysts and corpus luteum cysts. In a normal menstrual cycle, an ovary releases an ovum (egg) each month. The ovum grows inside a tiny sac called a follicle that breaks open to release the egg. Follicle cysts form when the follicle doesn’t break open to release the egg, causing it to continue growing into a cyst. Follicle cysts often have no symptoms and typically resolve in one to three months.
During normal ovulation, after the follicle breaks open and releases the egg, the empty follicle sac shrinks into a mass of cells called a corpus luteum. Corpus luteum cysts form if the empty follicle sac doesn’t shrink as it should, but instead reseals itself and builds up with fluid. Most corpus luteum cysts go away after a few weeks, but they can grow to ten centimeters (four inches) wide and cause pain. They may also bleed or cause the ovary to twist, requiring surgery such as a laparoscopy or a laparotomy[26]:
- Laparoscopy (lap-uh-ROSS-kuh-pee): During this surgery, the physician makes a very small incision above or below the umbilicus (navel) and inserts instruments with a camera to look inside the pelvic area and remove the cyst, which is then sent to a pathology lab for analysis. This type of surgery is typically performed for smaller cysts that appear benign (i.e., not cancerous) on the ultrasound.
- Laparotomy (lap-uh-ROT-uh-mee): A laparotomy is typically performed for large cysts or those that are suspicious on ultrasound as cancerous. This surgery uses a larger incision in the abdomen to remove the cyst, and then the cyst is sent to a pathology lab for analysis.
Pelvic Inflammatory Disease
Pelvic inflammatory (PĔL-vĭk ĭn-flă-MĂ-tŏ-rē) disease (PID) is inflammation of some or all of the female reproductive organs, resulting from the spread of bacteria from the cervix and vagina. PID is a serious complication of chlamydia and gonorrhea. The most common symptoms of PID are the following[27]:
- Lower abdominal and pelvic pain
- Increased vaginal discharge
- Irregular menstrual bleeding
- Fever (>38° C or >101°F)
- Pain with intercourse
- Painful and frequent urination
- Cervical motion tenderness
Complications of PID include tubo-ovarian abscess, infertility, ectopic pregnancy, and chronic pelvic pain. A tubo-ovarian abscess (TŪ-bō ō-VAR-ē-ăn ăb-sĕs) is an inflammatory mass involving the Fallopian tube and ovary and requires hospital admission. Treatment includes broad-spectrum antibiotics with or without a drainage procedure. Surgery may be required for patients with a suspected rupture or who fail to respond to antibiotics.[28] An ectopic pregnancy (ĕk-TŌP-ĭk PRĔG-năn-sē) is the implantation of an embryo outside of the uterus, typically in the fallopian tube.
Polycystic Ovary Syndrome
Polycystic ovary syndrome (pŏl-ē-SĬS-tĭk Ō-vă-rē SĬN-drōm) (PCOS) is a condition characterized by hormone imbalances, ovulatory dysfunction, and multiple ovarian cysts (i.e., small sacs of fluid). Fluid-filled cysts containing immature eggs are called follicles. Instead of releasing an egg during ovulation, the follicles (cysts) build up and enlarge. See Figure 7.8[29] for an illustration of PCOS.
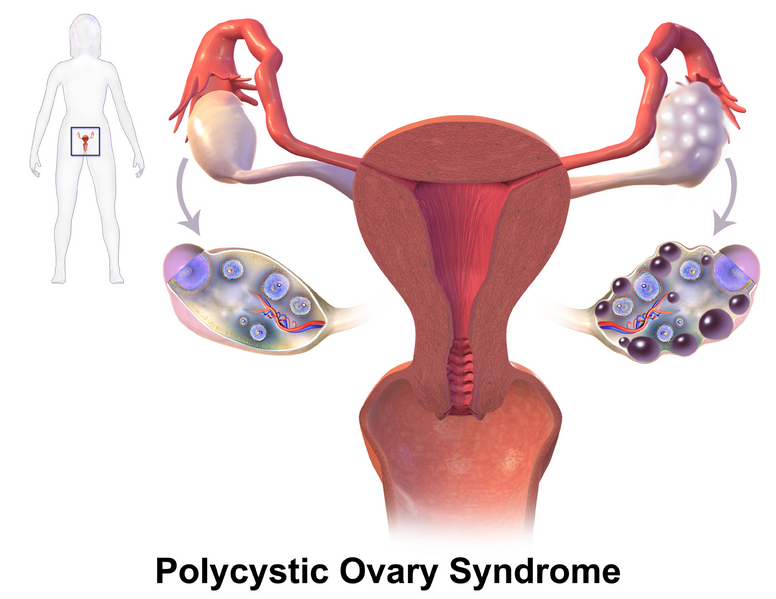
PCOS has no known cause, but it is associated with obesity and excessive insulin production. Common symptoms of PCOS include oligomenorrhea, amenorrhea, polymenorrhea, and enlarged ovaries due to multiple cysts or follicles. High levels of androgen hormones associated with PCOS can cause hirsutism (HĬR-sū-tĭz-ŭm) or excess facial and body hair. PCOS can also cause infertility.[30]
PCOS is diagnosed with blood tests and a transvaginal ultrasound. Treatments for PCOS include birth control pills to control menstrual cycles, diabetes medications to reduce insulin resistance, and medication to promote ovulation.
Premenstrual Syndrome (PMS)
Premenstrual syndrome (prē-MĔN-stroo-ăl SĬN-drōm) (PMS) is a syndrome involving physical and emotional symptoms occurring up to ten days before menstruation. Symptoms may include fluid retention (bloating), headaches, nervous tension, irritability, and breast tenderness. For some women, these symptoms can be so severe it causes them to miss work or school. Researchers think that PMS happens in the days after ovulation because estrogen and progesterone levels begin falling dramatically if the egg is not fertilized. PMS symptoms go away within a few days after menses begins and hormone levels begin rising again.[31].
Premenstrual Dysphoric Disorder
Premenstrual dysphoric (prē-MĔN-strŭ-ăl dis-FŌR-ĭk) disorder (PMDD) is a disorder that affects about 5% of menstruating females. It has similar symptoms as premenstrual syndrome (PMS) but is more serious. PMDD causes severe irritability, depression, or anxiety in the week or two before the menstrual cycle, and these issues go away two to three days after menstruation starts. Symptoms can include the following[32]:
- Lasting irritability or anger that may affect other people
- Feelings of sadness or despair, or even thoughts of suicide
- Feelings of tension or anxiety
- Panic attacks
- Mood swings or crying often
- Lack of interest in daily activities and relationships
- Trouble thinking or focusing
- Tiredness or low energy
- Food cravings or binge eating
- Trouble sleeping
- Feeling out of control
- Physical symptoms, such as cramps, bloating, breast tenderness, headaches, and joint or muscle pain
Women with PMDD require medications and other treatments such as the following[33]:
- Antidepressants called selective serotonin reuptake inhibitors (SSRIs) that increase serotonin levels in the brain
- Birth control pills to help regulate hormone levels
- Over-the-counter pain relievers, such as ibuprofen, naproxen, or aspirin to help relieve physical symptoms
- Stress management and relaxation techniques
- Healthy lifestyle changes, such as healthy food choices across the food groups, cutting back on salty and sugary foods, and getting more physical activity
Prolapse
A prolapse (PRŌ-laps) is the displacement of an organ or anatomic structure from its normal position. A uterine prolapse (ŪT-ĕ-rīn PRŌ-laps) is the downward displacement of the uterus into the vagina. A uterine prolapse occurs when the pelvic floor muscles and ligaments stretch and weaken until they no longer provide enough support for the uterus. As a result, the uterus slips down into or protrudes out of the vagina. Uterine prolapse most often affects people after menopause who have had one or more vaginal deliveries. Surgery may be required to treat the prolapse.[34]
An anterior vaginal prolapse (vă-jĭ-năl PRŌ-laps), also known as a cystocele (SĬS-tō-sēl) or a protrusion of the bladder, is when the bladder drops from its usual position in the pelvis into the vagina. Anterior vaginal prolapse occurs when the pelvic floor becomes weak or if too much pressure is put on the pelvic floor. This can happen over time, during vaginal childbirth, or with chronic constipation, violent coughing, or heavy lifting. Surgery may be required to treat the prolapse.[35]
A posterior vaginal prolapse, also known as a rectocele (RĔK-tō-sēl) or rectal prolapse, is when the rectum protrudes into the vagina.
Sexually Transmitted Infections
Sexually transmitted infections (STI), also known as sexually transmitted diseases, can cause serious disease in both men and women. For brevity of this textbook, STIs are thoroughly discussed in the “Sexually Transmitted Infections” subsection of the “Diseases and Disorders of the Male Reproductive System” section in the “Male Reproductive System Terminology” chapter. Review that section for information about signs and symptoms of several STIs in females.
Uterine Fibroid
A uterine fibroid (ŪT-ĕ-rīn FIB-royd) is a benign tumor in the muscular wall of the uterus in women. See Figure 7.9[36] for an illustration of fibroids.
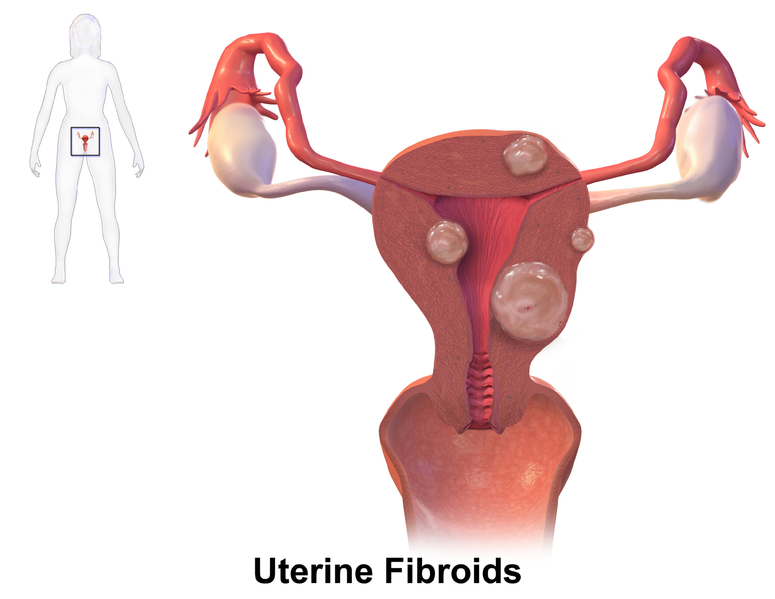
The cause of fibroids is unknown. Symptoms of uterine fibroids are as follows[37]:
- Dysmenorrhea
- Menorrhagia
- Metrorrhagia
- A feeling of fullness in the lower abdomen
- Frequent urination
- Dyspareunia
- Lower back pain
- Reproductive problems, such as infertility, multiple miscarriages, or early labor
Symptomatic uterine fibroids may be treated with birth control pills or medications to shrink the fibroids. For women with fibroids with moderate or severe symptoms, several types of surgery may be used to treat them[38]:
- Myomectomy (mī-ō-MĔK-tŏ-mē): Surgery that removes fibroids without taking out healthy tissue of the uterus. This surgery is best for women who wish to have children after treatment. It can be major surgery (involving cutting into the abdomen) or performed with laparoscopy or hysteroscopy.
- Hysterectomy (his-tĕ-REK-tŏ-mē): Surgery to remove the uterus when fibroids are large, if the women is experiencing very heavy bleeding, or if the woman is near menopause or does not want future pregnancy. Read more about different types of hysterectomies in the “Medical Specialties, Diagnostic Testing, and Procedures Related to the Female Reproductive System” section.
- Endometrial ablation (ĕn-dō-MĒ-trē-ăl ă-blā-shŏn): The lining of the uterus is removed or destroyed to control very heavy bleeding. This can be done using several methods such as a laser, wire loops, electric current, microwaves, freezing, and other methods. This procedure usually is considered minor surgery and can be done on an outpatient basis or in a doctor’s office. A woman cannot have future pregnancies after this procedure.
- Myolysis (mī-OL-ŏ-sĭs): A needle is inserted into the fibroids, guided by laparoscopy, and electric current or freezing is used to destroy the fibroids.
- Uterine fibroid embolization (ŪT-ĕ-rīn FĪ-brŏyd ĕm-bō-lĭ-ZĀ-shŏn) (UFE) or uterine artery embolization (ŪT-ĕ-rīn ăr-tĕr-ē ĕm-bō-lĭ-ZĀ-shŏn) (UAE): A thin tube is threaded into the blood vessels that supply blood to the fibroid, then tiny plastic particles are injected into the blood vessels to block the blood supply to the fibroid. The lack of blood supply causes the fibroid to shrink.
Toxic Shock Syndrome
Toxic shock syndrome (TŌK-sĭk SHŌK SĪN-drōm) (TSS) is a severe bacterial infection that has many causes, including superabsorbent tampon (TĂM-pon) use. Tampons are cotton plugs used to absorb menstrual flow. TSS is caused by Staphylococcus and Streptococcus bacteria, and symptoms include sudden high fever, vomiting or diarrhea, a rash resembling a sunburn on the palms and soles, confusion, muscle aches, headaches, low blood pressure, and seizures. TSS can cause acute kidney failure and death. To help prevent TSS, the U.S. Food and Drug Administration requires manufacturers to use standard measurement and labeling for absorbency and to print guidelines on the boxes. Women should use the lowest absorbency tampon required for their flow and change tampons at least every four to eight hours.[39]
Vaginal Candidiasis
Vaginal candidiasis (vă-jĭ-năl kăn-dĭ-DĪ-ă-sĭs), also called a yeast infection, is a common fungal infection of the vagina and the vulva that causes thick, white discharge and intense itching. It is typically treated with medication inserted vaginally.[40]
- Family Doctor. (2023, June). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Family Doctor. (2023, June). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Family Doctor. (2023, June). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Family Doctor. (2023, June). Abnormal uterine bleeding. American Academy of Family Physicians. https://familydoctor.org/condition/abnormal-uterine-bleeding ↵
- Centers for Disease Control and Prevention. (2023, July 25). What is breast cancer? https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm ↵
- “En_Breast_cancer_illustrations.png” by Morning2k for the National Institutes of Health is licensed in the Public Domain. ↵
- Centers for Disease Control and Prevention. (2023, July 25). What is breast cancer? https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm ↵
- American Cancer Society. (2023). Breast cancer. https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html ↵
- Centers for Disease Control and Prevention. (2023, July 25). What is breast cancer? https://www.cdc.gov/cancer/breast/basic_info/what-is-breast-cancer.htm ↵
- National Cancer Institute. (2023, August 23). Breast cancer treatment - (PDQ) patient version. National Institutes of Health. https://www.cancer.gov/types/breast/patient/breast-treatment-pdq#_185 ↵
- National Cancer Institute. (2021, September). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021, September). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021, September). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021, September). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2021, September). Understanding cervical changes: A health guide. National Institutes of Health. https://www.cancer.gov/publications/patient-education/understanding-cervical-changes ↵
- National Cancer Institute. (2023, June 26). Endometrial cancer screening (PDQ) - patient version. National Institutes of Health. https://www.cancer.gov/types/uterine/patient/endometrial-screening-pdq ↵
- National Cancer Institute. (2023, June 26). Endometrial cancer screening (PDQ) - patient version. National Institutes of Health. https://www.cancer.gov/types/uterine/patient/endometrial-screening-pdq ↵
- National Cancer Institute. (2023, June 26). Endometrial cancer screening (PDQ) - patient version. National Institutes of Health. https://www.cancer.gov/types/uterine/patient/endometrial-screening-pdq ↵
- National Cancer Institute. (2022, December 22). Ovarian, epithelial, fallopian tube, and primary peritoneal cancer treatment (PDQ®)– patient version. National Institutes of Health. https://www.cancer.gov/types/ovarian/patient/ovarian-epithelial-treatment-pdq ↵
- National Cancer Institute. (2022, December 22). Ovarian, epithelial, fallopian tube, and primary peritoneal cancer treatment (PDQ®)– patient version. National Institutes of Health. https://www.cancer.gov/types/ovarian/patient/ovarian-epithelial-treatment-pdq ↵
- Mayo Clinic. (2018, July 24). Endometriosis. https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656 ↵
- “Blausen_0349_Endometriosis.png” by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014 is licensed under CC BY 3.0 ↵
- Mayo Clinic. (2018, July 24). Endometriosis. https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656 ↵
- Mayo Clinic. (2018, July 24). Endometriosis. https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2016, Oct 1]. Menopause; [reviewed 2016, cited 2023, Oct 8.] https://medlineplus.gov/menopause.html ↵
- Office on Women's Health. (2021, February 22). Ovarian cysts. https://www.womenshealth.gov/a-z-topics/ovarian-cysts ↵
- Centers for Disease Control and Prevention. (2021, July 22). Pelvic inflammatory disease (PID)- CDC detailed fact sheet. https://www.cdc.gov/std/pid/stdfact-pid-detailed.htm ↵
- Centers for Disease Control and Prevention. (2021, July 22). Pelvic inflammatory disease (PID)- CDC detailed fact sheet. https://www.cdc.gov/std/pid/stdfact-pid-detailed.htm ↵
- “PCOS_%28Part_2%29.png” by BruceBlaus is licensed under CC BY 4.0 ↵
- Mayo Clinic. (2022, September 8). Polycystic ovary syndrome (PCOS). https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439 ↵
- Office On Women's Health. (2021, February 22). Premenstrual syndrome (PMS). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome# ↵
- Office On Women's Health. (2021, February 22). Premenstrual dysphoric disorder (PMDD). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd ↵
- Office on Women's Health. (2021, February 22). Premenstrual dysphoric disorder (PMDD). https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd ↵
- Mayo Clinic. (2022, September 8). Uterine prolapse. https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/symptoms-causes/syc-20353458 ↵
- Mayo Clinic. (2023, April 6). Anterior vaginal prolapse. https://www.mayoclinic.org/diseases-conditions/cystocele/symptoms-causes/syc-20369452 ↵
- “Uterine_Fibroids.png” by BruceBlaus is licensed under CC By 4.0 ↵
- Office on Women's Health. (2021, February 19). Uterine fibroids. https://www.womenshealth.gov/a-z-topics/uterine-fibroids ↵
- Office on Women's Health. (2021, February 19). Uterine fibroids. https://www.womenshealth.gov/a-z-topics/uterine-fibroids ↵
- Mayo Clinic. (2022, March 23). Toxic shock syndrome. https://www.mayoclinic.org/diseases-conditions/toxic-shock-syndrome/symptoms-causes/syc-20355384 ↵
- Mayo Clinic. (2022). Yeast infection (Vaginal). https://www.mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999 ↵

