6.4 Anatomy of the Male Reproductive System
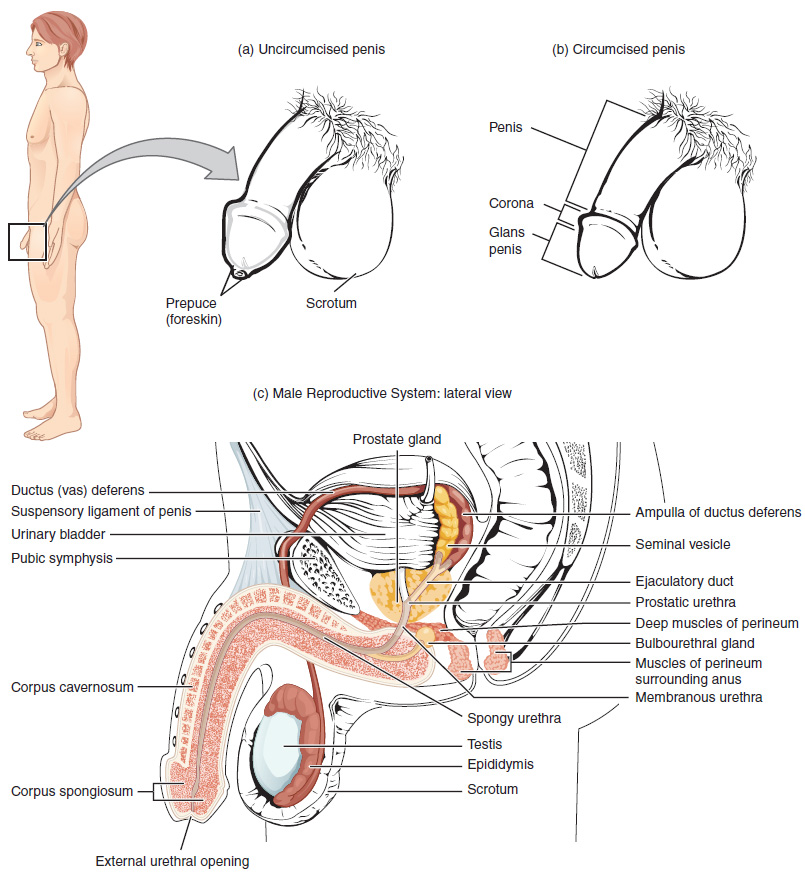
The structures of the male reproductive system include the testes and epididymis in the scrotum; the vas deferens, seminal vesicles, and bulbourethral glands; the prostate gland; and the penis. These structures are well-vascularized with many glands and ducts to promote the formation, storage, and ejaculation of sperm for fertilization and to also produce testosterone.[1]
See Figure 6.1[2] for an illustration of these structures of the male reproductive system.
Testes
The testes (TĔS-tēz) are the male reproductive organs. They produce both sperm and androgen (AN-drŏ-jĕn), (i.e., the male sex hormone testosterone), and are active throughout the reproductive life span of the male. There are two testes, each approximately four to five cm in length, that are housed within the scrotum (SKRŌ-tŭm), an external pouch.[3]
During the seventh month of the developmental period of a male fetus, the testes move through the abdominal musculature to descend into the scrotal cavity. This is called the “descent of the testes.” Cryptorchidism (krip-TOR-kĭd-izm) is the clinical term used when one or both of the testes fail to descend into the scrotum prior to birth.[4] Anorchism (ă-NOR-kĭzm) refers to the absence of one of the testes. See Figure 6.2[5] for an illustration of a testicle.
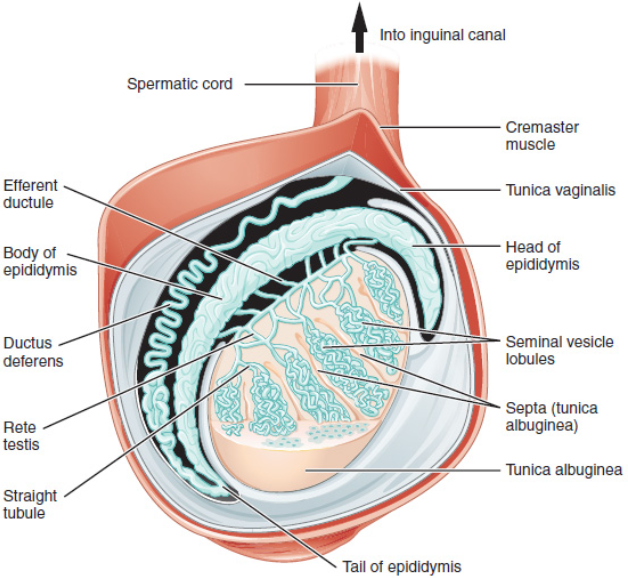
The spermatic cord (spur-MAT-ĭk KORD) is a bundle of blood vessels, nerves, and ducts that connect the testicles to the abdominal cavity through the inguinal canal. There are several disorders related to the spermatic cord. The spermatic cord is sensitive to torsion (TOR-shŏn), in which the testicle rotates within its sac and blocks its own blood supply. An inguinal hernia (IN-gwĭ-năl HUR-nē-ă) can occur, referring to protrusion of abdominal contents through the inguinal canal into the scrotum. Varicose veins can occur in the spermatic cord, referred to as varicocele (VAR-ĭ-kō-sēl). Though often asymptomatic, about one in four men with varicocele may experience infertility.[6]
Each testis is divided by septa into 300 to 400 structures called lobules. Within the lobules, sperm develop in structures called seminiferous tubules (sem-ĭ-NIF-ĕr-ŭs TŪ-būls). Newly produced sperm leave the seminiferous tubules and travel to the epididymis (ep-ĭ-DID-ĭ-mĭs), a coiled tube on top of the testes where the newly formed sperm continue to mature for an average of 12 days. As they are moved along the length of the epididymis, the sperm further mature and acquire the ability to move under their own power. Once inside the female reproductive tract, they will use this ability to move independently toward the unfertilized egg. Mature sperm are stored in the tail of the epididymis until ejaculation occurs.[7]
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the vas deferens (VĀS DEF-ĕr-ĕnz). Sperm make up only 5 percent of the final volume of semen (SĒ-mĕn), the thick, milky fluid that a male ejaculates. This fluid is produced by accessory glands of the male reproductive system, the seminal vesicles (SEM-ĭ-năl VES-ĭ-kĕlz), the prostate, and the bulbourethral glands. From here, the semen travels through the urethra to the outside of the body during ejaculation.[8]
Because the vas deferens is easily accessible within the scrotum, surgical sterilization to interrupt sperm delivery can be performed by cutting and sealing a small section of the vas deferens, referred to as a vasectomy (vă-SEK-tō-mē). Read more about vasectomy in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Male Reproductive System” section.
Prostate and Bulbourethral Glands
As sperm pass through the vas deferens at ejaculation, they mix with fluid produced by the associated seminal vesicle. Seminal vesicle fluid contains large amounts of fructose, which is used by the sperm mitochondria to generate energy to allow movement through the female reproductive tract. The seminal fluid, now containing both sperm and seminal vesicle secretions, moves into the associated ejaculatory duct. The paired ejaculatory ducts transport the seminal fluid into the prostate gland.[9]
The prostate (PRŌS-tāt) is a gland that is anterior to the rectum at the base of the bladder and surrounds the urethra. A normal prostate gland is the size of a walnut. It excretes an alkaline, milky fluid in semen to coagulate (thicken) and then decoagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract, providing time for sperm to utilize the fructose provided by seminal vesicle secretions. When semen regains its fluid state, the sperm can pass farther into the female reproductive tract.[10]
The final addition to semen is made by two bulbourethral glands (bul-bō-ū-RĒ-thrăl glandz) that release a thick, salty fluid to lubricate the end of the urethra and the vagina, as well as cleanse urine residue from the urethra. The fluid from these accessory glands is released after the male becomes sexually aroused and shortly before the release of the semen, so it is often referred to as pre-ejaculate. It is possible for bulbourethral fluid to pick up sperm already present in the urethra and cause pregnancy. Semen moves into the penis via the urethra, a multifunction anatomical structure that also transports urine from the bladder.[11]
Penis
The penis (PĒ-nĭs) is a male reproductive organ that is flaccid during nonsexual actions, such as urination, and becomes stiff and rod-like during sexual arousal. When erect, the stiffness of the penis allows it to penetrate into the vagina and deposit semen into the female reproductive tract, referred to sexual intercourse or coitus (KŌ-ĭ-tŭs).
The glans penis (glănz PĒ-nĭs) refers to the tip of the penis. Circumcision (sĭr-kŭm-SIZH-ŏn) is the surgical removal of the foreskin (FŌR-skin), also called prepuce (PRĒ-pyūs), a fold of skin that covers the tip of the penis. Read more about circumcision in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Male Reproductive System” section.
- This work is a derivative of StatPearls by Gurung, Yetiskul, & Jialal and is licensed under CC BY 4.0 ↵
- “Figure_28_01_01.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Figure_28_01_03.JPG” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
