4.7 Medical Specialists, Diagnostic Testing, and Procedures Related to the Respiratory System
Specialists
Pulmonologist
Respiratory medicine is concerned with the diagnosis and treatment of diseases related to the respiratory system. Respiratory medicine requires in-depth knowledge of internal medicine. A physician who specializes in diagnosing and treating respiratory system disease is called a pulmonologist (pŭl-mŏn-ŎL-ŏ-jĭst).[1]
For more information, visit the American Lung Association’s page on pulmonologists.
Respiratory Therapist
Respiratory therapists (rĕ-spĭr-ă-tōr-ē THĔR-ă-pĭsts) (RTs) are health care professionals that monitor, assess, and treat people who are having problems breathing. RTs are licensed in the state in which they practice. RTs are trained in ventilation and airway management, cardiopulmonary resuscitation, and oxygen and aerosol therapy. They provide care for patients undergoing cardiac stress-testing, pulmonary function testing, smoking cessation, high-risk births, rehabilitation, and surgery. They also assist in treating patients with asthma, COPD, heart failure, and pneumonia.[2]
For more information, visit the American Association for Respiratory Care’s What is an RT? web page.
Thoracic Surgeon
A thoracic surgeon (thō-RĂS-ĭk SŬR-jŏn) refers to a surgeon who has specialized in either thoracic (chest) surgery or cardiothoracic (heart and chest) surgery. They perform surgery for patients with serious conditions of the heart, lungs, and other structures in the chest cavity.[3]
To learn more about thoracic surgeons, visit WebMD’s What is a Thoracic Surgeon? web page.
Diagnostic Testing and Procedures
Arterial Blood Gas
Arterial blood gas (ar-TĬR-ē-ăl blŭd găs) (ABG) is a measurement of dissolved oxygen and carbon dioxide levels in blood taken from an artery. ABG is often obtained for patients who have deteriorating or unstable respiratory status requiring urgent and/or emergency treatment. An ABG is typically drawn in the forearm from the radial artery by a respiratory therapist, emergency or critical care nurse, or other health care provider.
Bronchoscopy
A bronchoscopy (bron-KOS-kŏ-pē) is a procedure used to visualize the bronchi with a bronchoscope (BRŎNG-kŏ-skōp), a thin, flexible tube with a light and a lens or small video camera on the end. The tube is inserted into the patient’s nose or mouth, down the throat, into the trachea (windpipe), and into the airways (bronchi and bronchioles) of the lungs. It is typically performed by a physician. See Figure 4.19[4] for an image of a bronchoscopy.

A bronchoscopy is performed to look for the causes of problems in the airways of the lungs or to further examine an abnormal area seen on an imaging test (such as a chest X-ray or CT scan).[5] Any abnormal areas in the airways that are seen with the bronchoscope can be biopsied to determine the cause of the abnormal finding. A biopsy is performed by passing long, thin instruments down the bronchoscope, such as small forceps (tweezers), needles, or brushes to collect the samples. Sterile salt water can also be flushed down the bronchoscope to rinse the airways and then suctioned up, which is referred to as a bronchial washing (BRŎNG-kē-ăl WŎSH-ing). The biopsy samples are visually examined under a microscope in a pathology lab.[6]
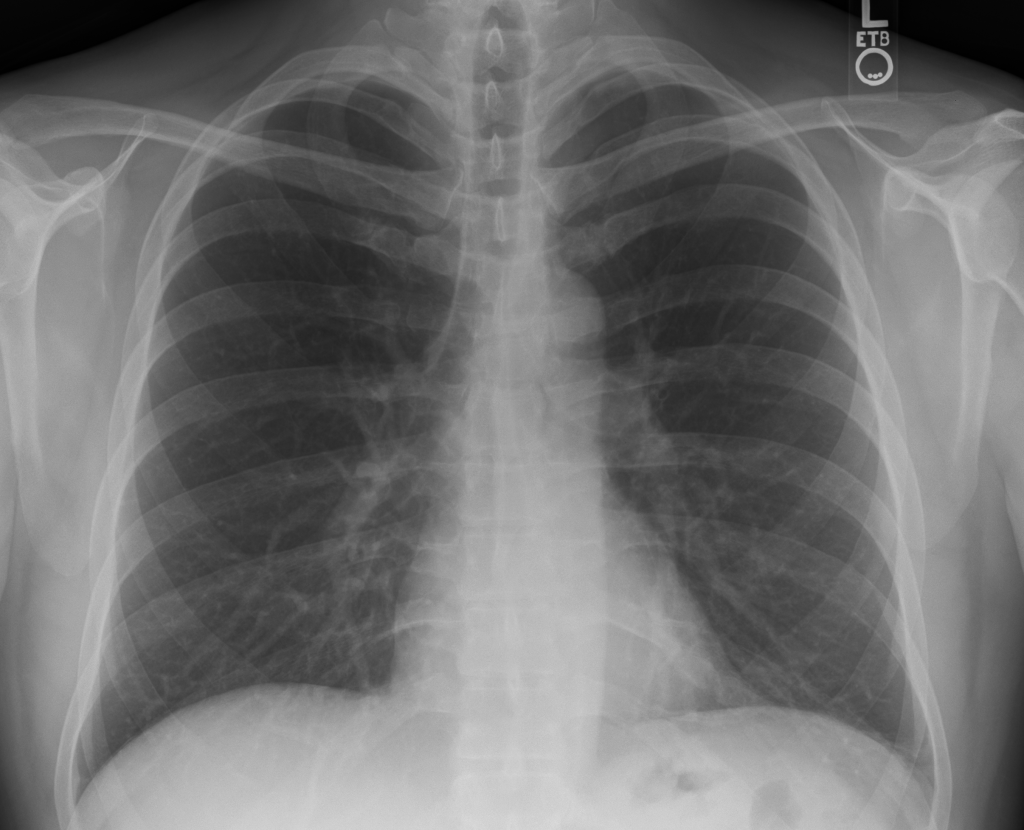
Chest X-Ray
As discussed earlier, a chest x-ray (CXR) is also referred to as a radiograph. Using a controlled beam of radiation, a CXR produces shadow-like images of organs and tissues like the bones, lungs, heart, and the diaphragm. After passing through the body, the beam hits a piece of film or a special detector. Tissues in the body absorb or block the radiation to varying degrees. Dense tissues, such as bones, block most radiation and appear white on the CXR. Soft tissues, like fat or muscle, block less radiation and show up in shades of gray. Organs that are mostly air (such as the lungs) appear black. Tumors are usually denser than the tissue around them, so they often show up as lighter shades of gray.[7] See Figure 4.20[8] for an image of a CXR. A CXR is used to diagnose a variety of respiratory conditions, such as pneumonia, pulmonary edema, and cancer.
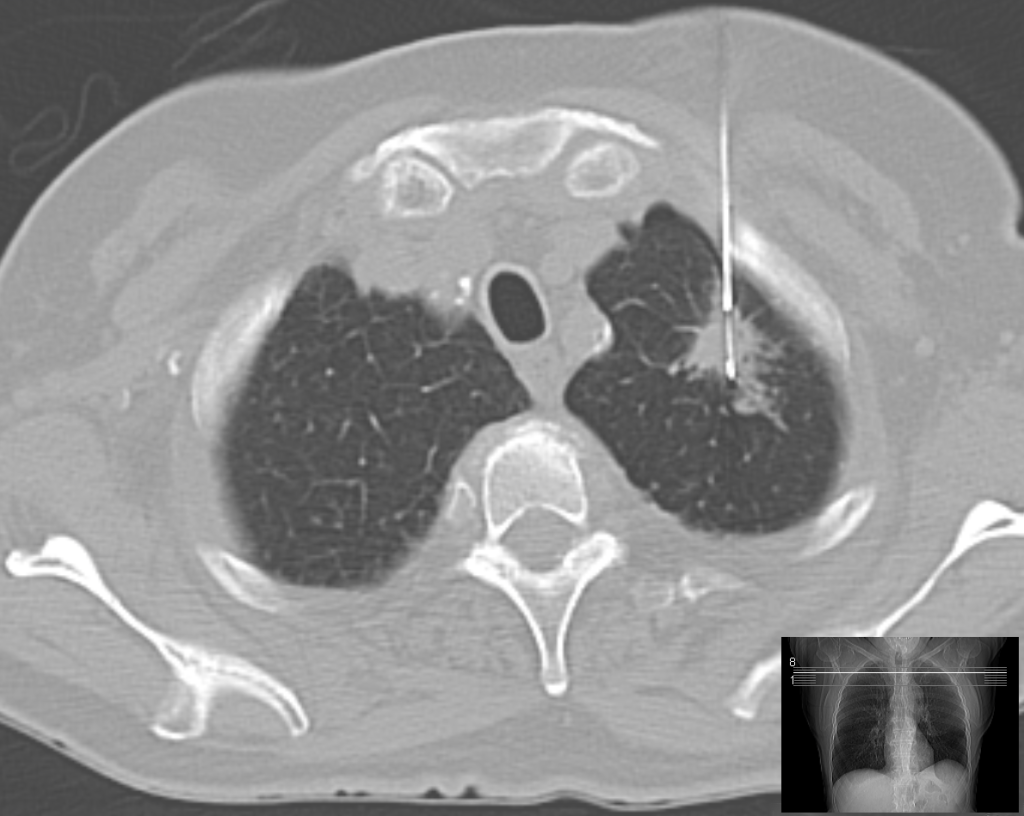
Computed Tomography (CT) Scan
A computed tomography scan (kŏm-PYŌŌ-tĕd tŏ-mŎG-ră-fē skăn) (CT) uses X-rays to make detailed cross-sectional images of a person’s body. Instead of taking one or two pictures like a regular X-ray, a CT scanner takes many pictures and then a computer combines them to create detailed images in slices of the part of the body being studied. See Figure 4.21[9] for an image of a CT scanner.

A CT scan is more likely to show lung tumors than routine chest X-rays. It can also show the size, shape, and position of any lung tumor and can help visualize enlarged lymph nodes that might contain cancer that has spread. A CT scan can also be used to look for masses in the liver, brain, and other organs that can occur if the cancer has metastasized.[10]
If a suspected area of cancer is deep within the body, a CT scan can be used to guide a biopsy needle into this area to obtain a tissue sample to biopsy for cancer. This procedure is referred to as a CT-guided needle biopsy (sē-tē GĪ-dĕd NĒ-dŭl BĪ-ŏp-sē).[11] See Figure 4.22[12] for an image of a CT-guided needle biopsy of the lung.
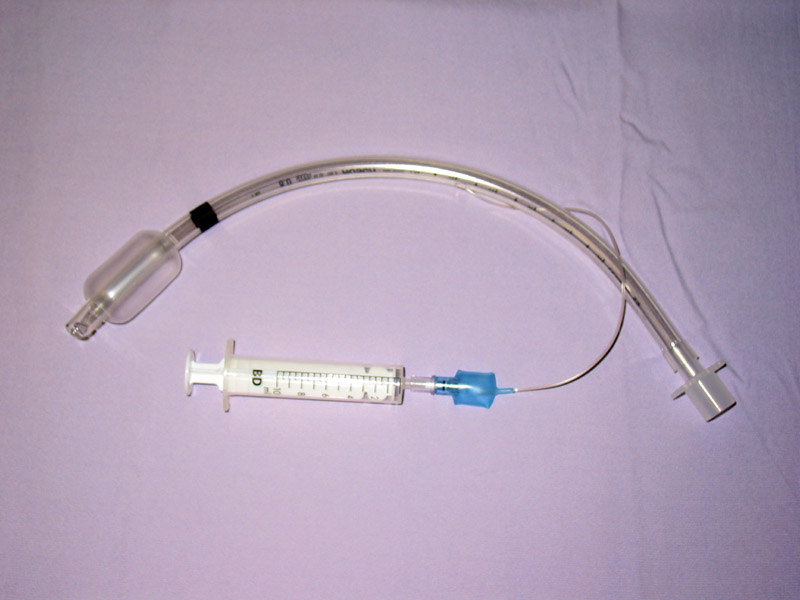
Endotracheal Intubation
When a patient is experiencing respiratory failure or receiving general anesthesia during surgery, an endotracheal tube (ĕn-dō-TRĀ-kē-ăl tūb) (ET tube) is inserted to maintain a patent airway by health care professionals with advanced training, such as a respiratory therapist, paramedic, anesthesiologist, or physician. The ET tube is sealed within the trachea with an inflatable cuff, and oxygen is supplied via a bag valve mask or via mechanical ventilation. See Figure 4.23[13] for an image of a cuffed endotracheal tube.
Magnetic Resonance Imaging (MRI)
Similar to CT scans, magnetic resonance imaging (măg-NĔT-ĭk rĕz-ŏ-năns ĬM-ă-jing) (MRI) scans show detailed images of soft tissues in the body. However, MRI scans use radio waves and strong magnets instead of radiation. MRI scans are used to diagnose many medical conditions, such as soft tissue abnormalities, tears in ligaments, joint abnormalities, and tumors. They are also used to evaluate for metastasis of cancer to other areas of the body, such as the brain, liver, lungs, and bones.[14]
Mechanical Ventilation
A mechanical ventilator (mĕ-kăn-Ĭ-kăl vĕn-tĬ-lā-tŏr) is a machine attached to an endotracheal tube to assist or replace spontaneous breathing. Mechanical ventilation is termed invasive because it requires placement of an endotracheal tube in the trachea. Mechanical ventilators are typically managed by respiratory therapists. See Figure 4.24[15] for an image of a simulated patient who is intubated with an endotracheal tube that is attached to a mechanical ventilator.

Needle Biopsy
During a needle biopsy (NĒ-dŭl BĪ-ŏp-sē), doctors use a needle to obtain a small sample of cells from a suspicious area (mass) to examine under a microscope. An advantage of needle biopsies is that they don’t require a surgical incision. There are a variety of types of needle biopsies. One type of needle biopsy is a fine needle aspiration biopsy (fīn NĒ-dŭl ăs-pĭ-RĀ-shŭn BĪ-ŏp-sē) (FNA). During this procedure, a syringe with a very thin, needle is used to aspirate (ĂS-pĭ-rāt) or withdraw cells and small fragments of tissue. An FNA biopsy is often used to check for cancer in lymph nodes.[16]
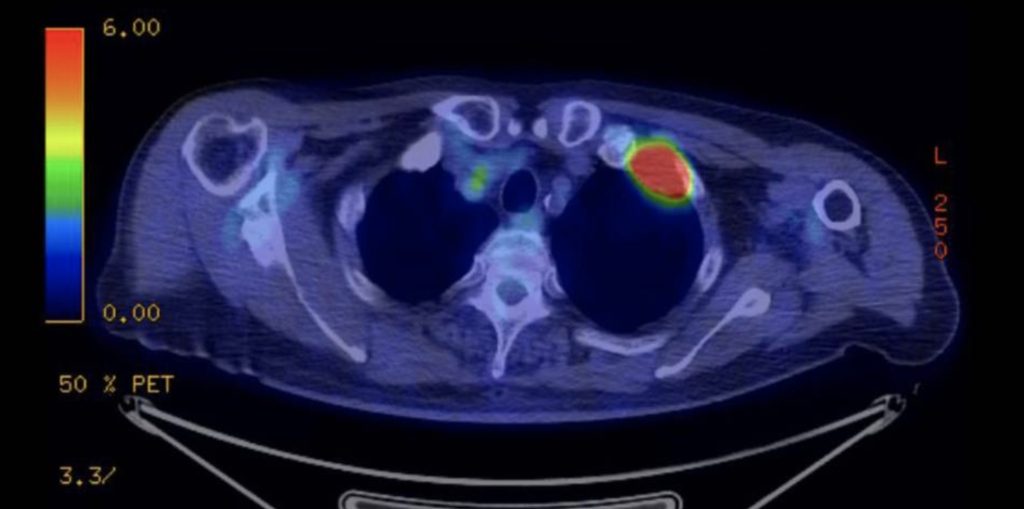
Positron Emission Tomography Scan
During a positron emission tomography scan (pŏz-Ĭ-trŏn ĭ-MĬSH-ən tŏ-mŏG-ră-fē skăn) (PET), a slightly radioactive substance is injected into the patient’s blood. If cancer cells are present in the body, they have a higher uptake of this radioactive substance and appear as a highlighted area on the scan. Often a PET scan is combined with a CT scan so the highlighted areas on the PET scan can be easily visualized with the corresponding image on the CT scan. PET/CT scans are useful to determine if cancer has spread to other parts of the body.[17] See Figure 4.25[18] for an image of a PET/CT scan showing a red highlighted area of radioactive substance, indicating cancer cells have spread to this area of the body.
Pulmonary Function Tests
Pulmonary function tests (PŬL-mŏ-nā-rē fŭnk-shŭn tĕsts) (PFTs) allow physicians and respiratory therapists to evaluate the respiratory function of patients with various types of lung disease. PFTs do not provide a specific diagnosis, but the results are combined with other assessment data to reach a diagnosis. PFTs also help determine the severity of pulmonary disease, assess the patient’s response to treatment, and monitor for possible disease progression over time.[19]
Spirometry (spī-RŎM-ĕ-trē) is a common PFT that measures the patient’s ability to inhale and exhale air relative to time using a device called a spirometer. Spirometry is used for diagnosis and therapeutic management of common respiratory disorders, such as asthma and chronic obstructive pulmonary disease (COPD). The primary measurements during spirometry testing are forced vital capacity (FVC), forced expiratory volume exhaled in the first second (FEV1), and the FEV1/FVC ratio. The spirometry procedure has three phases that include maximal inspiration, a “blast” of exhalation, and a complete exhalation.[20] View an illustration of spirometry in Figure 4.26.[21]

View the following YouTube video[22] for more information about spirometry: How To Do a Spirometry Test and Interpret the Results
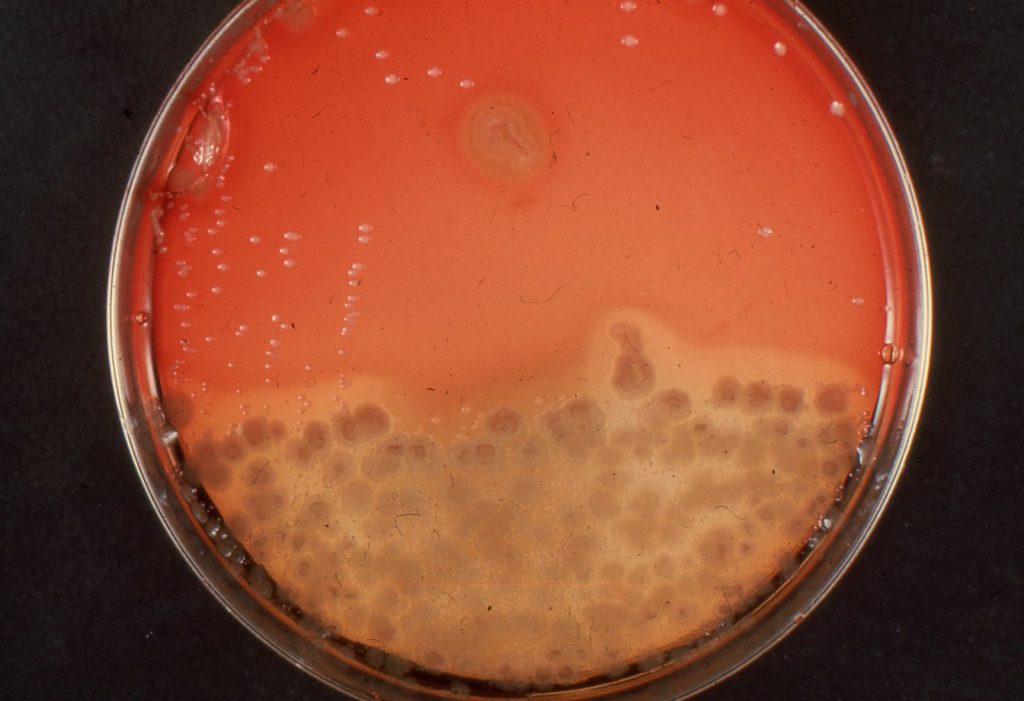
Sputum Culture
A sputum culture (SPYŌŌ-tŭm KŬL-chŭr) is a diagnostic test that evaluates the type and number of bacteria present in mucus from the respiratory tract. The patient is asked to cough deeply and spit any mucus that comes up into a sterile specimen container. Care must be taken to ensure the specimen only contains mucus and not saliva. The sample is sent to a lab where it is placed in a special dish and examined for two to three days or longer to see if bacteria or other disease-causing pathogens grow. See Figure 4.27[23] for an image of a sputum culture.
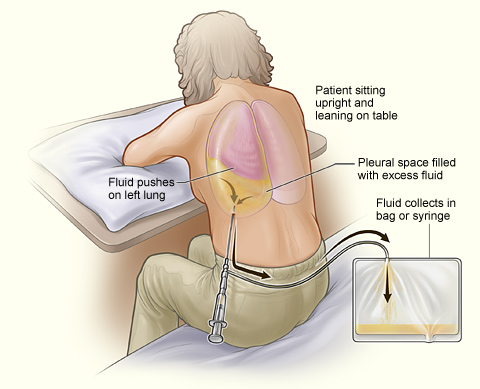
Thoracentesis
If fluid has collected in the pleural space around the lungs (called a pleural effusion), health care providers perform a procedure called a thoracentesis (thor-uh-sen-TEE-sis) to remove the fluid. Pleural effusion is typically caused by a medical condition, such as pneumonia, heart failure, infection, or lung cancer.
During a thoracentesis, the patient’s skin is numbed, and a needle is inserted between the ribs to aspirate (i.e., suction) the fluid for examination in the lab. If recurrent pleural effusions cause the patient to have trouble breathing, thoracentesis may be repeated to remove additional fluid to help the patient breathe better.[24] See Figure 4.28[25] for an illustration of removal of fluid during a thoracentesis.
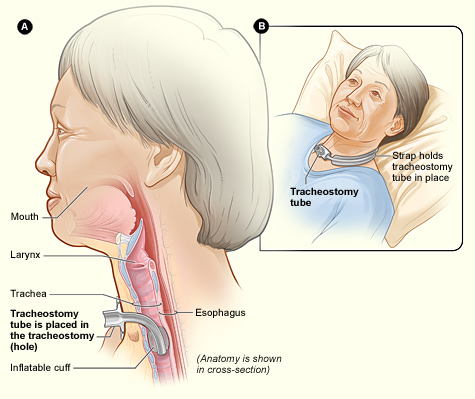
Tracheostomy
A tracheostomy (trā-kē-ŎS-tŏ-mē) is a surgically created opening, called a stoma, that goes from the front of the patient’s neck into the trachea. A tracheostomy tube is placed through the stoma into the trachea to maintain a patent (open) airway and to administer oxygen. A tracheostomy may be an emergent procedure performed due to an airway obstruction or a planned procedure to manage a disease process. See Figure 4.29[26] for an illustration of a patient with a tracheostomy tube in place.
Respiratory Equipment
There are various types of medical devices related to the respiratory system.
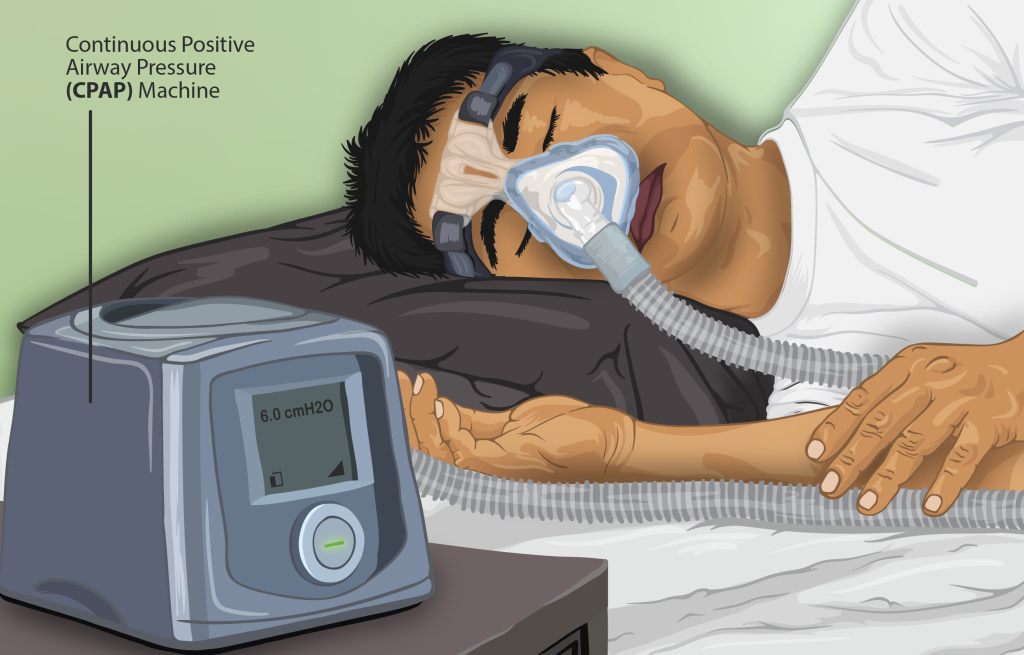
Continuous Positive Airway Pressure (CPAP)
A continuous positive airway pressure device (kŏn-TĬN-yū-ŭs POZ-ĭ-tĭv AIR-wā PRESS-ŭr dĭ-VĪS) (CPAP) is used for people who are able to breathe spontaneously on their own but need help in keeping their airway unobstructed, such as those with obstructive sleep apnea. The CPAP device consists of a special mask that covers the patient’s nose, or nose and mouth, and is attached to a machine that continuously applies mild air pressure to keep the patient’s airways from collapsing. See Figure 4.30[27] for an illustration of a patient wearing a CPAP device while sleeping.
Bilevel Positive Airway Pressure (BiPAP)
A bilevel positive airway pressure (BĪ-lĕv-ĕl PŎZ-ĭ-tĭv ĀR-wā PRĔSH-ŭr) (BiPAP) device is similar to a CPAP device in that it is used to prevent airways from collapsing, but BiPAP devices have two pressure settings. One setting occurs during inhalation, and a lower pressure setting is used during exhalation. Patients using BiPAP devices in their home environment for obstructive sleep apnea often find these two pressures more tolerable because they don’t have to exhale against continuous pressure. In acute care settings, BiPAP devices are also used for patients in acute respiratory distress as a noninvasive alternative to intubation and mechanical ventilation and are managed by respiratory therapists. See Figure 4.31[28] for an image of a simulated patient wearing a BiPAP mask in a hospital setting.

Nasal Cannula
A nasal cannula (NĀ-zăl KĂN-yū-lă) is the simplest and most commonly used oxygenation device. It consists of oxygen tubing connected to two short prongs that are inserted into the patient’s nares (nostrils). See Figure 4.32[29] for an image of a nasal cannula. Nasal cannulas are used for short- and long-term therapy and are best used with stable patients who require low amounts of oxygen, such as patients with COPD.

Read more information about additional oxygenation devices such as a high-flow nasal cannula, non-rebreather mask, partial rebreather mask, Venturi mask, oxymask, and oxymizer in the “Oxygenation Equipment” section of the “Oxygen Therapy” chapter of Open RN Nursing Skills, 2e.
Pulse Oximeter
A pulse oximeter (pŭls ŏk-SĬM-ĭ-tŏr) is a commonly used portable device used to obtain a patient’s oxygen saturation level, often referred to as a pulse oximetry reading. The pulse oximeter analyzes light produced by the probe as it passes through the finger to determine the saturation level of hemoglobin with oxygen while also analyzing the pulse rate See Figure 4.33[30] for an image of a portable pulse oximeter. The normal range for a pulse oximetry reading for an adult without an underlying respiratory condition is 94-100%.

- American Lung Association. (2019, May 14). Know your providers - What does a pulmonologist do? https://www.lung.org/blog/know-your-providers-pulmonologist ↵
- American Association for Respiratory Care. (n.d.). What is an RT? https://www.aarc.org/careers/what-is-an-rt/ ↵
- WebMD. (2023, July 8). What is a thoracic surgeon? https://www.webmd.com/a-to-z-guides/what-is-a-thoracic-surgeon ↵
- “Bronchoskopie_Bronchoalveoläre_Lavage.jpg” by User:MrArifnajafov is licensed under CC BY-SA 3.0 ↵
- American Cancer Society. (2019, January 14). Bronchoscopy. https://www.cancer.org/cancer/diagnosis-staging/tests/endoscopy/bronchoscopy.html ↵
- American Cancer Society. (2019, January 14). Bronchoscopy. https://www.cancer.org/cancer/diagnosis-staging/tests/endoscopy/bronchoscopy.html ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- “Chest Xray PA 3-8-2010.png” by Stillwaterising is licensed under CC0 ↵
- “Moderní_výpočetní_tomografie_s_přímo_digitální_detekcí_rentgenového_záření.jpg” by Tomáš Vendiš is licensed under CC BY-SA 4.0 ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- “Biopsie_Lunge_Computertomographie_BC.png” by Hellerhoff is licensed under CC BY-SA 3.0 ↵
- “Sondeintubation.jpg” by bigomar2 is licensed under CC BY-SA 3.0 ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- “Simulated intubated patient on a mechanical ventilator” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- “Anterior_Pancoast_tumor_PET.jpg” by Soichi Oka, Kenji Ono, Kenta Kajiyam, and Katsuma Yoshimatsu is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of StatPearls by Ponce, Sankari, & Sharma and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ponce, Sankari, & Sharma and is licensed under CC BY 4.0 ↵
- “Spirometry_Part_1.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- BMJ Learning. (2020, July 1). How to do a spirometry test and interpret the results [Video]. YouTube. All rights reserved. https://youtu.be/jSkwBoed6Tw?si=AQxyjWNULZLAgC2t ↵
- “m241-8 Blood agar culture of sputum from patient with pneumonia. Comprimised host. Colonies of Candida albicans and pseudomonas aeruginosa (LeBeau)” by Microbe World is licensed under CC BY-NC-SA 2.0 ↵
- American Cancer Society. (2022, August 15). Tests for lung cancer. https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/how-diagnosed.html ↵
- “Thoracentesis.jpg” by National Heart, Lung and Blood Institute is licensed in the Public Domain. ↵
- “Tracheostomy NIH.jpg” by National Heart, Lung, and Blood Institute is in the Public Domain. ↵
- “Depiction of a sleep apnea patient using a CPAP machine” by https://www.myupchar.com/en is licensed under CC BY 4.0 ↵
- “Simulated patient wearing a BiPAP mask” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Image00011.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/5-5-oxygen-therapy-systems/ ↵
- “OxyWatch_C20_Pulse_Oximeter.png” by Thinkpaul is licensed under CC BY-SA 3.0 ↵
