14.6 Diseases and Disorders of the Muscular System
This section will provide an overview of common diseases and disorders of the muscular system.
Cerebral Palsy
Cerebral palsy (sĕr-Ē-brăl pôl-zē) (CP) is a group of disorders that affects the ability to move and maintain balance and posture. CP is the most common motor disability in childhood. “Cerebral” means having to do with the brain, and “palsy” means weakness or problems with using the muscles. CP is caused by abnormal brain development or damage to the developing brain that affects the ability to control muscles.[1]
The symptoms of CP vary from person to person. A person with severe CP might require the use of special equipment to walk or might not be able to walk at all and need lifelong care. A person with mild CP, on the other hand, might walk a little awkwardly, but otherwise not require specialized care. Doctors classify CP according to the main type of movement disorder involved. Depending on which areas of the brain are affected, one or more of the following movement disorders can occur[2]:
- Spasticity (spăs-TĬS-ĭ-tē): Stiff muscles
- Dyskinesia (dĭs-kĭ-NĒ-zē-ă): Uncontrollable movements
- Ataxia (ă-TĂK-sē-ă): Poor balance and coordination
There is no cure for CP, but treatment can improve the quality of life for people who have the condition. After CP is diagnosed, a team of health professionals works with the child and family to develop a plan to help the child reach their optimal potential. Common treatments include medications; surgery; braces; and physical, occupational, and speech therapy.[3]
See Figure 14.6[4] for an image of David Smith who has cerebral palsy and has won several Paralympian awards. Paralympians are athletes with a range of impairments who compete in the Paralympics, a competition similar to the Olympics. Paralympic athletes inspire people around the world with their performance and focus on moving forward and never giving up.[5]

Contracture
A contracture (kŏn-TRĂK-chŭr) is a condition of shortening and hardening of muscles, tendons, or other tissue, often leading to deformity and rigidity of joints. Contractures are caused by immobility and can be the result of several disorders such as a stroke, cerebral palsy, or muscular dystrophy. Contractures may be prevented and/or treated with braces, physical therapy, and range-of-motion exercises. See Figure 14.7[6] for an image of a hand contracture.

Fibromyalgia
Fibromyalgia (fī-brō-mī-AL-jē-ă) is defined as pain in muscle fibers. It is a condition that causes widespread pain, sleep problems, fatigue, and often emotional distress. Fibromyalgia affects about 2% of the adult population in the United States. The cause of fibromyalgia is not known, but it can be effectively treated and managed. Fibromyalgia is diagnosed by health care providers based on the patient’s history, physical examination, X-rays, and blood work.[7]
Fibromyalgia is treated by a doctor or team of health care professionals who specialize in the treatment of fibromyalgia. A combination of treatments is typically prescribed, which may include the following[8]:
- Medications, including prescription drugs and over-the-counter pain relievers
- Aerobic exercise and muscle strengthening exercise
- Patient education classes
- Stress management techniques such as meditation, yoga, and massage
- Good sleep habits to improve the quality of sleep
- Cognitive behavioral therapy, a type of talk therapy that helps people change the way they think about their life circumstances
Muscular Dystrophy
Muscular dystrophy (mŭs’kyŭ-lăr DĬS-trŏ-fē) (MD) refers to group of diseases caused by abnormal muscle development due to gene mutations. Muscular dystrophy can run in families, or a person can be the first in their family to have muscular dystrophy. Over time, muscle weakness decreases mobility and makes it difficult to perform everyday tasks. There are many types of muscular dystrophy, each affecting specific muscle groups. Each type has signs and symptoms that appear at different ages and vary in severity.[9]
An example of one type of MD is Duchenne muscular dystrophy (DMD), a genetic disorder characterized by progressive muscle degeneration and weakness due to the alterations of a muscle protein called dystrophin. DMD symptom onset is in early childhood, usually between the ages 2 and 3. The disease primarily affects boys. Muscle weakness is the principal symptom of DMD and begins by first affecting the proximal muscles (those closest to the core of the body) and later affecting the distal limb muscles. The child with DMD might have difficulty jumping, running, and walking. Other symptoms include enlargement of the calves, a waddling gait, and lumbar lordosis (an inward curve of the spine). The heart and respiratory muscles are affected as well. Progressive weakness and scoliosis result in impaired pulmonary function, which can eventually cause acute respiratory failure. Treatment of DMD requires multidisciplinary care to coordinate specialized assessments and interventions needed to maximize function and quality of life. Due to recent advances in cardiology and pulmonology, people with DMD are living longer than ever and often well into adulthood.[10]
The impact of DMD can be significantly minimized by keeping the body as flexible, upright, and mobile as possible. As muscle deteriorates, a person with muscular dystrophy often develops contractures. If not treated, contractures can become severe, causing discomfort and restricting mobility and flexibility. Contractures can affect the knees, hips, feet, elbows, wrists, and fingers. However, there are many ways to minimize and postpone contractures. Range-of-motion exercises, performed on a regular schedule, help delay contractures by keeping tendons from shortening prematurely. Braces on the lower legs also can help keep the limbs stretched and flexible, delaying the onset of contractures. Eventually, a wheelchair is needed, typically by about age 12. Although a child and parents may dread using a wheelchair, many people find that when they start to use one, they are more mobile, energetic, and independent than when trying to walk without assistance.[11] See Figure 14.8[12] for an image of child with MD using a specialized wheelchair called an “Easy Stand” that supports him while sitting and also allows him to stand for periods of time.

Myasthenia Gravis
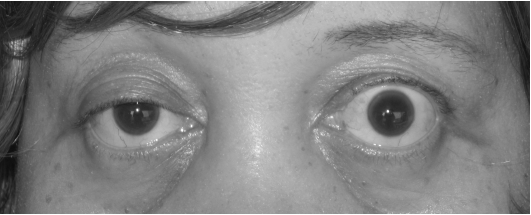
Myasthenia gravis (mī-ăs-THĒ-nē-ă GRĂ-vĭs) (MG) is a chronic, autoimmune neuromuscular disease that causes weakness in voluntary muscles, including those required for breathing and swallowing. Onset of symptoms can be rapid and include the following[13]:
- Myasthenia (mī-ăs-THĒ-nē-ă): Abnormal weakness of voluntary muscles
- Ocular myasthenia (Ō-kyŭ-lăr mī-ăs-THĒ-nē-ă): Weakness of the eye muscles
- Ptosis (TŌ-sĭs): Drooping of one or both eyelids (See Figure 14.9[14] for an image of ptosis.)
- Diplopia (dĭ-PLŌ-pē-ă): Blurred or double vision
- Dysphagia (dĭs-FĀ-jē-ă): Difficulty swallowing
- Dyspnea (dĭsp-NĒ-ă): Shortness of breath
- Dysarthria (dĭs-ĂR-thrē-ă): Impaired speech
Sometimes the muscles that control breathing weaken to the point where a person needs a ventilator to breathe. This is called a myasthenic crisis and requires immediate emergency medical care. A myasthenic crisis may be triggered by infection, stress, surgery, or an adverse reaction to medication.[15]
MG is diagnosed by health care providers based on a physical exam, blood tests, and electromyography (EMG). Read more about EMG in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Muscular System” section. MG is treated with medications that improve neuromuscular transmission and increase muscle strength. Immunosuppressive medications may be prescribed to impact the autoimmune response. In some cases, a thymectomy (i.e., removal of the thymus) may be performed to rebalance the immune system and decrease MG symptoms.[16]
Paralysis
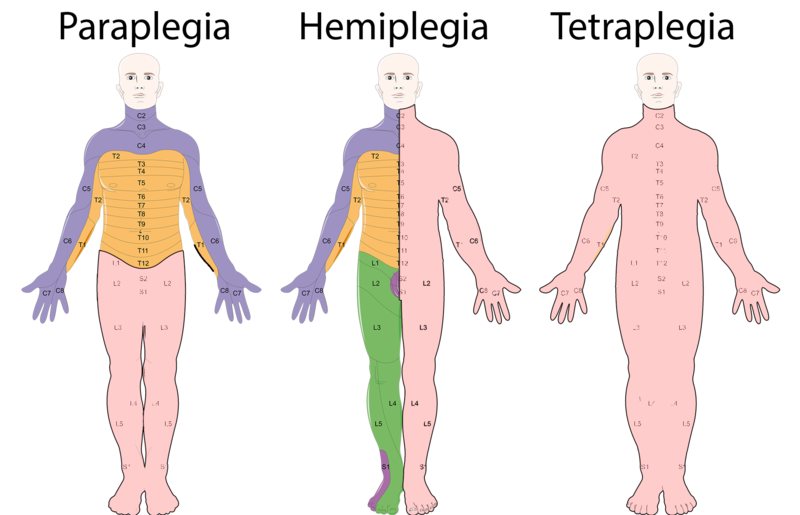
Paralysis (păr-ă-LĪ-sĭs) occurs when an injury or medical condition disrupts the nerve signals to the muscles, resulting in being unable to make voluntary movements. Common causes of paralysis include spinal cord injuries and strokes. Paralysis can be localized, where it affects specific areas of the body, such as the face. For example, Bell’s palsy temporarily paralyzes facial muscles. Paralysis can also be generalized where it affects a larger area of the body. There are categories of generalized paralysis based on its extent. Common categories include hemiplegia, paraplegia, and quadriplegia/tetraplegia[17]
- Hemiplegia (hĕm-ē-PLĒ-jē-ă): Paralysis affects one side of the body, for example, an arm and a leg on the same side.
- Paraplegia (păr-ă-PLĒ-jē-ă): Paralysis affects both legs and sometimes the torso.
- Quadriplegia or Tetraplegia (kwŏd-rĭ-PLĒ-jē-ă or tĕt-ră-PLĒ-jē-ă): Paralysis involves all limbs, with little or no movement from the neck down.
See Figure 14.10[18] for an illustration of paraplegia, hemiplegia, and tetraplegia (quadriplegia), where pink indicates the area of muscle paralysis. Because muscle paralysis is caused by disruption of nerve signals, the cervical (C), thoracic (T), and lumbar (L) nerves are labelled in the image.
Paralysis is also classified by its effect on muscles in terms of being flaccid or spastic[19]:
- Flaccid (FLĂS-ĭd): The muscles atrophy (ĂT-rŏ-fē) (i.e., shrink) due to loss of function.
- Spastic (spăs-TĬK): The muscles tighten, causing uncontrollable jerks and spasms.
There is no cure for permanent paralysis caused by spinal nerve damage because the spinal cord can’t heal itself. However, rehabilitative services like physical and occupational therapy can help people with paralysis live independently and enjoy quality of life. Equipment used for rehabilitative/restorative care may include the following[20]:
- Adaptive equipment (ă-DĂP-tĭv ĭ-KWĬP-mĕnt): Equipment that allows people to feed themselves or drive.
- Assistive equipment (ă-SĬS-tĭv ĭ-KWĬP-mĕnt): Equipment that enhances mobility, such as wheelchairs, scooters, crutches, and canes.
- Orthotic/prosthetic devices (ŏr-THŎT-ĭk/prŏs-THĔT-ĭk dĭ-VĪS-ĕz): Devices that support the limbs and prevent contractures, such as braces.
- Voice-activated technology (vois-ăk-TĬV-ā-tĕd tĕk-NŎL-ŏ-jē): Technology that doesn’t require the need for touch or movement, such as computers, lighting systems, and phones.
See Figure 14.11[21] for an image of Mark Manion, founder of “Mark Speaks Out.” Mark was permanently disabled during a cross-country biking trip when he was struck by a drunk driver. He travels the country educating and inspiring audiences on how he has effectively coped with his life circumstances.

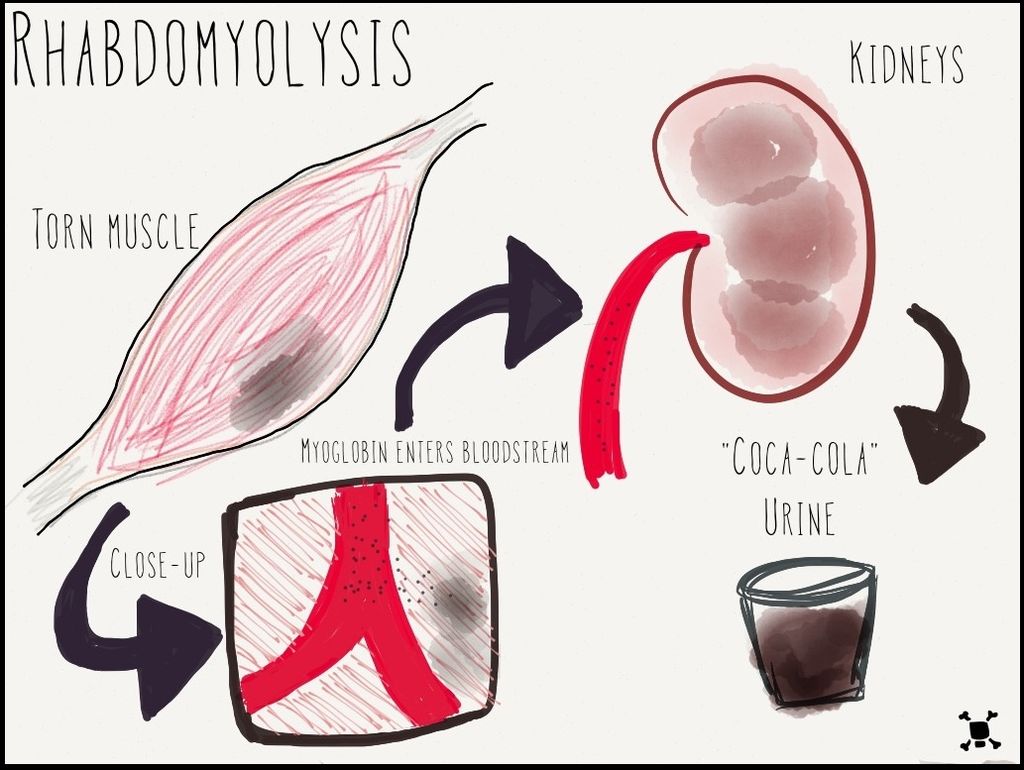
Rhabdomyolysis
Rhabdomyolysis (rab-dō-mī-OL-ĭ-sĭs) refers to the breakdown of muscles that causes damage to the kidney. When muscle is damaged, a protein called myoglobin (mī-Ō-glŏ-bĭn) is released into the bloodstream and is filtered out of the body by the kidneys. Myoglobin breaks down into substances that damage kidney cells.[22] See Figure 14.12[23] for an illustration of rhabdomyolysis.
Rhabdomyolysis may be caused by injury or any other condition that damages skeletal muscle. Potential causes of rhabdomyolysis include the following conditions[24]:
- Trauma or crush injuries
- Use of drugs such as cocaine, amphetamines, statins, heroin, or phencyclidine (PCP)
- Genetic muscle diseases
- Extremes of body temperature
- Ischemia or death of muscle tissue
- Low phosphate levels
- Seizures or muscle tremors
- Severe exertion, such as marathon running or calisthenics
- Lengthy surgical procedures
- Severe dehydration
Symptoms of rhabdomyolysis include dark, red, or cola-colored urine; decreased urine output; weakness; and myalgia (mī-AL-jē-ă) (i.e., muscle pain). Rhabdomyolysis is diagnosed with blood tests, including creatine kinase (CK), myoglobin, and creatinine, as well as urine tests such as urinalysis and urine myoglobin. Rhabdomyolysis is treated with intravenous fluids that contain bicarbonate. In cases causing severe kidney damage, dialysis may be required.[25]
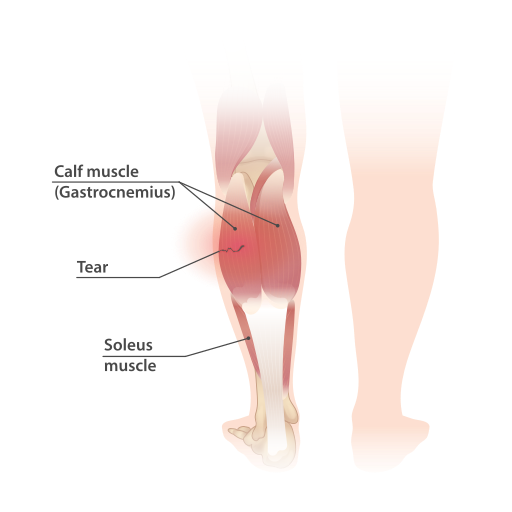
Strain
A strain (strān) is an injury to a muscle or tendon from being overstretched or torn, causing pain. Strains can be caused by an injury, overusing a muscle, or using a muscle in the wrong way (such as twisting the back while lifting a heavy object). A strain is different from a sprain (sprān), which is an injury to a joint when a ligament is stretched or torn. See Figure 14.13[26] for an illustration of a muscle strain and tear. Initial treatments for strains and sprains are similar and can be easily recalled by the mnemonic called RICE, which stands for the following[27]:
- Rest: Rest the strain or sprain for at least 24 hours. The health care provider may recommend not putting any weight on the injured area for 48 to 72 hours, so crutches may be needed for lower extremity injuries.
- Ice: Apply ice as soon as possible after the injury to reduce swelling. The ice should not be applied directly to the skin but should be wrapped in a cloth to avoid tissue injury. Ice should be applied for 5 to 20 minutes, four to eight times a day, for the first 48 hours or until swelling improves.
- Compression: Compress the area with an elastic wrap or bandage to reduce swelling.
- Elevate: Elevate the injured limb above your heart whenever possible to help prevent or limit swelling.
Tendonitis
Tendonitis (ten-dŏ-NĪT-ĭs) refers to inflammation of a tendon, causing pain around a joint. Tendonitis usually happens after repeated injury to an area such as the wrist or ankle. Common forms of tendonitis are named after the sports that increase their risk, such as tennis elbow, golfer’s elbow, pitcher’s shoulder, swimmer’s shoulder, and jumper’s knee. Health care providers diagnose tendonitis based on medical history, a physical exam, and possible imaging tests. Initial treatment is focused on reducing pain and swelling with RICE (rest, ice, compression, and elevation). Other treatments may include ultrasound, physical therapy, steroid injections, and surgery in severe cases.[28]
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- “David_Smith_and_his_Boccia_medals_(cropped).jpg” by Richard Gillin from St Albans, UK is licensed under CC BY-SA 2.0 ↵
- International Paralympic Committee. (n.d.). FAQ. https://www.paralympic.org/frequently-asked-questions ↵
- “Freeman-Sheldon_syndrome.JPG” by MI Poling at English Wikipedia is licensed under CC BY-SA 2.5 ↵
- Centers for Disease Control and Prevention. (2020, January 6). Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm ↵
- Centers for Disease Control and Prevention. (2020, January 6). Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm ↵
- Centers for Disease Control and Prevention. (2022, November 21). What is muscular dystrophy? https://www.cdc.gov/ncbddd/musculardystrophy/facts.html ↵
- Muscular Dystrophy Association. (n.d.). Duchenne muscular dystrophy. https://www.mda.org/disease/duchenne-muscular-dystrophy ↵
- Muscular Dystrophy Association. (n.d.). Duchenne muscular dystrophy. https://www.mda.org/disease/duchenne-muscular-dystrophy ↵
- “3576255511_4c36222845_b.jpg” by EasyStand is licensed under CC BY-NC-ND 2.0 ↵
- National Institute of Neurological Disorders and Stroke. (2023, November). Myasthenia gravis. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis ↵
- “Ptosis_myasthenia_gravis.jpg” by Mohankumar Kurukumbi, Roger L Weir, Janaki Kalyanam, Mansoor Nasim, Annapurni Jayam-Trouth is licensed under CC BY 2.0 ↵
- National Institute of Neurological Disorders and Stroke. (2023, November). Myasthenia gravis. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis ↵
- National Institute of Neurological Disorders and Stroke. (2023, November). Myasthenia gravis. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- “Neurological_Levels_%26_Types_of_Paralysis.png” by Servier Medical Art is licensed under CC BY 2.0 ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- “USMC-100519-M-3215R-002.jpg” by unknown author for United States Marine Corps is licensed in the Public Domain ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- “Rhabdo.jpg” by AquapatMedia is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- “Calf_muscle_strain_and_tear.svg” by InjuryMap is licensed under CC BY-SA 4.0 ↵
- Mayo Clinic. (2022, March 22). Sprain: First aid. https://www.mayoclinic.org/first-aid/first-aid-sprain/basics/art-20056622 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2022, Apr. 4]. Tendinitis; [cited 2017, Mar. 16]. https://medlineplus.gov/tendinitis.html ↵
