5.6 Diseases and Disorders of the Urinary System
Acute Kidney Failure
Acute kidney failure (ā-kūt kĭd-nē fāl-yŭr) is the rapid (less than two days) loss of kidney function. There are many possible causes of acute kidney failure. They include the following[1]:
- Acute tubular necrosis (damage to the renal tubules)
- Autoimmune kidney disease
- Decreased blood flow to the kidneys due to very low blood pressure, which can result from dehydration, hemorrhage, serious illness or injury, or surgery
- Disorders that cause clotting within the kidney’s blood vessels
- Infections that directly injure the kidney, such as acute pyelonephritis (severe infection of the kidneys)
- Pregnancy complications, including placental abruption (separation of the placenta from the uterine wall) or placenta previa (placenta blocking the cervix)
- Urinary tract blockage
- Illicit drugs such as cocaine and heroin
- Medicines including nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics and blood pressure medicines, intravenous contrast (dye), HIV medications, and some types of cancer
Acute kidney failure is diagnosed through blood and urine tests that measure creatinine, urea nitrogen, and protein levels in the blood and urine. Read more information about these diagnostic tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section.
Acute kidney failure is typically treated with dialysis and medications. Read more information about dialysis in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section.
Chronic Kidney Disease
Kidney disease is a leading cause of death in the United States. More than one in seven American adults have chronic kidney disease (KRŎN-ĭk kĭd-nē dĭ-ZĒZ) (CKD) where the kidneys are damaged and cannot filter blood as well as they should. Because of the decreased kidney function, excess fluid and waste products remain in the body and cause other health problems. CKD has varying levels of seriousness and usually gets worse over time, although treatment has been shown to slow its progression. If left untreated, CKD can progress to kidney failure. Kidney failure is also called end-stage renal disease (ĕnd-stāj rē-năl dĭ-ZĒZ).[2]
Risk factors for developing CKD include diabetes mellitus type 1 and type 2, high blood pressure, heart disease, family history of CKD, and obesity. People with CKD may not feel ill or notice any symptoms. The only way to diagnose CKD is through blood and urine tests that measure creatinine, urea nitrogen, and protein levels. Read more information about these diagnostic tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section.
CKD is treated by carefully managing blood pressure and diabetes to prevent further damage to the nephrons. If the kidneys stop working, dialysis or a kidney transplant is needed for survival.[3] Read more information about dialysis and kidney transplantation in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section.
Glomerulonephritis
Glomerulonephritis (glō-mĕr-ū-lō-nĕ-FRĪ-tĭs) involves inflammation of the glomerular capillaries. Glomerulonephritis can be caused by immune system problems, cancer, or infections such as strep infections, viruses, heart infections, or abscesses. It can develop quickly and lead to kidney failure, or it can become a chronic disease. Damage to the glomeruli affects their ability to filter correctly, and blood and protein can be lost in the urine. Common symptoms of glomerulonephritis include blood in the urine (hematuria), foamy urine (due to excess protein in the urine), and swelling (edema) of the face, eyes, ankles, feet, legs, or abdomen due to decreased protein (and osmotic pressure) in the bloodstream. Many diagnostic tests may be performed, but the diagnosis is typically confirmed by a kidney biopsy. Treatment depends upon the cause, but controlling high blood pressure with medications is usually the most important part of treatment. Drugs that suppress the immune system may also be prescribed.[4]
Hydronephrosis
Hydronephrosis (hī-drō-nĕ-FRŌ-sĭs) is the swelling of one or both kidneys because of urine backflow into the kidney. Several conditions can cause hydronephrosis, such as a kidney stone or other blockage in the ureters or back flow of urine from the bladder to the kidney, which is called vesicoureteral reflux (vĕs-ĭ-kō-yū-RĒT-ĕr-ăl rē-FLŬKS). Symptoms include back/side pain, an abdominal mass, nausea and vomiting, urinary tract infection (UTI), fever, dysuria (painful urination), and increased urinary frequency or urgency. Many diagnostic tests may be performed, such as an intravenous pyelogram. An intravenous pyelogram (IVP) is discussed in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section. Treatment is performed to treat the cause and may include placing a stent (tube) through the bladder and ureter to allow urine to flow from the kidney into the bladder, placing a tube into the kidney through the skin to allow the blocked urine to drain out of the body into a drainage bag, removing a stone causing the blockage, or performing surgery to correct the blockage or reflux.[5]
Nephrolithiasis
Nephrolithiasis (nĕf-rō-lĭ-THĪ-ă-sĭs), commonly referred to as kidney stones, is solid pieces of material that form in the kidney from substances in the urine, such as calcium or uric acid. A kidney stone, also called renal calculus (RĒ-năl KĂL-kŭ-lŭs), may be as small as a grain of sand or as large as a pearl. See Figure 5.12[6] for an image of various sizes of kidney stones. Most kidney stones pass out of the body without medical intervention, but some get stuck in the urinary tract, block the flow of urine, and cause severe pain. Pain is typically located in the back or side. People with kidney stones may have hematuria (blood in the urine), fever and chills, vomiting, foul-smelling urine that may appear cloudy, or dysuria (painful urination).[7]

Extracorporeal shock wave lithotripsy (LĬTH-ō-trĭp-sē) or commonly called ESWL is a procedure for treating stones in the kidney and ureter that does not require surgery. Instead, high-energy shock waves are passed through the body and used to break stones into pieces as small as grains of sand. Because of their small size, these pieces can then pass out the body with the urine.[8]
Nephrolithotomy (nĕf-rō-lĭ-THŎT-ŏ-mē) may be performed for patients who have large (two centimeters) or irregularly shaped kidney stones, stones that have not been broken up successfully by extracorporeal shock wave lithotripsy, or those who are not candidates for ureteroscopy. During this procedure, the surgeon enters the kidney through a small incision in the back and then threads a nephroscope (NĔF-rŏ-skōp), a miniature fiberoptic camera and then other small instruments, through the incision to remove the stone.[9]
Polycystic Kidney Disease
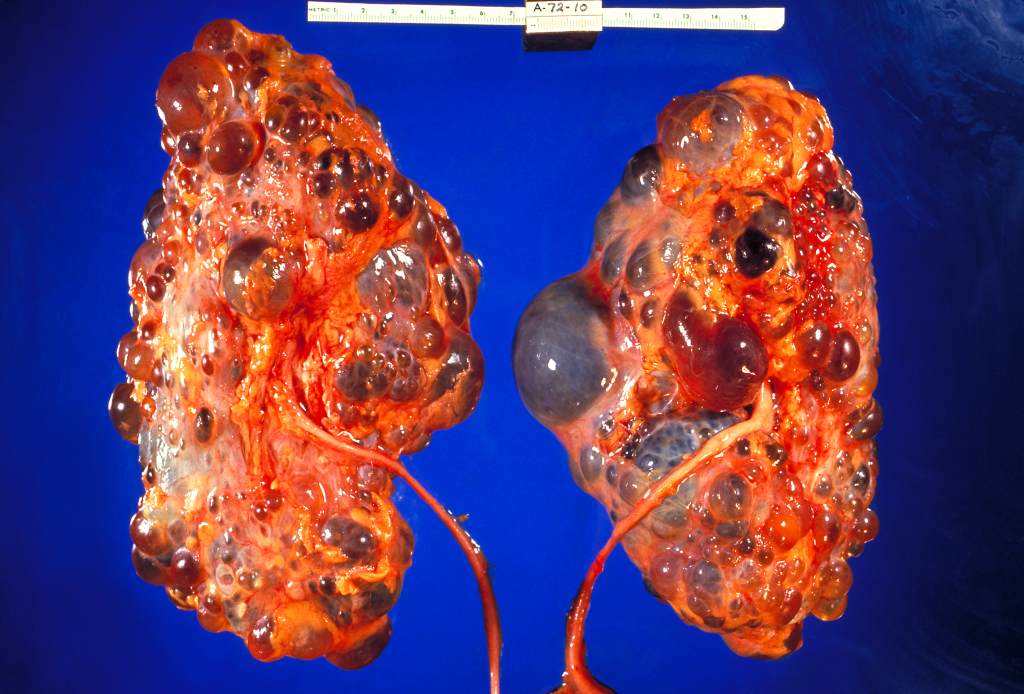
Polycystic kidney disease (pŏl-ē-SĬS-tĭk KĬD-nē dĭ-ZĒZ) (PKD) is an inherited genetic mutation that affects the kidneys and other organs. It is an inherited disorder that is passed down through families genetically. Clusters of fluid-filled sacs, called cysts, develop in the kidneys and interfere with their ability to filter waste products from the blood. See Figure 5.13[10] for an illustration of PKD. The growth of cysts causes the kidneys to become enlarged and can lead to chronic kidney disease (CKD). As CKD worsens, treatments for end-stage kidney disease may include dialysis or a kidney transplant. Cysts may also develop in other organs, particularly the liver. Cysts that are painful, infected, bleeding, or causing a blockage may need to be drained. There are usually too many cysts to make it practical to remove each cyst, so surgery to remove one or both kidneys may be needed.[11]
Renal Cell Cancer
Renal cell cancer (also called renal cell carcinoma) is the most common type of kidney cancer. Cancer occurs in tubules in the kidneys where urine is produced and collected. There are many types of treatments for renal cell cancer, including surgery, radiation therapy, chemotherapy, immunotherapy, and targeted therapy. The types of surgery that may be used are as follows[12]:
- Partial nephrectomy (nĕf-RĔK-tŏ-mē): A surgical procedure to remove the cancer within the kidney and some of the tissue around it.
- Simple nephrectomy (sĭm-pĭl nĕf-RĔK-tŏ-mē): A surgical procedure to remove the kidney.
- Radical nephrectomy (răd-ĭ-kăl nĕf-RĔK-tŏ-mē): A surgical procedure to remove the kidney, the adrenal gland, surrounding tissue, and, usually, nearby lymph nodes.
Urinary Incontinence
Urinary incontinence (YŪR-ĭ-nĕr-ē ĭn-KŎN-tĭ-nĕns) is the involuntary loss of urine. It is a common symptom that can seriously affect the physical, psychological, and social well-being of affected individuals.
There are many types and causes of urinary incontinence. A common type of incontinence is stress urinary incontinence (strĕs YŪR-ĭ-nĕr-ē ĭn-KŎN-tĭ-nĕns), a leakage of urine during moments of physical activity that increases abdominal pressure, such as coughing, sneezing, laughing, or exercise.[13] Overactive bladder is another type of incontinence where there is a frequent and sudden urge to urinate that can result in the individual not being able to make it to the restroom in time.
Diagnostic testing may be performed, such as a urinalysis to check for a urinary tract infection or urodynamic flow testing to evaluate bladder function, including filling, urine storage, and emptying.[14] Treatment of incontinence is based on the cause of incontinence and may include pelvic floor exercises, medications, or surgery.
Urinary Retention
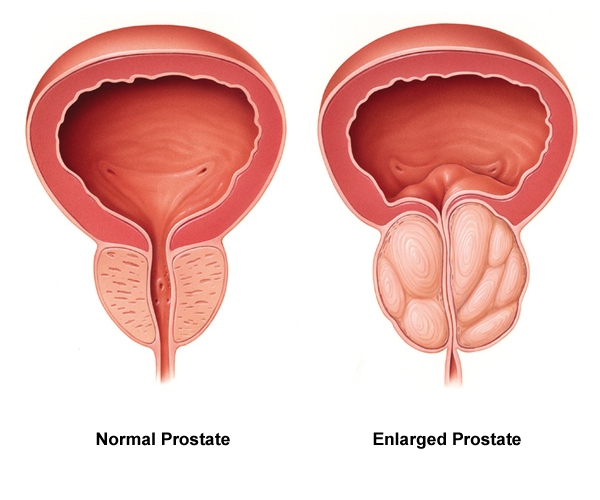
Urinary retention (YŪR-ĭ-nĕr-ē rĭ-TĔN-shŭn) is a condition that occurs when the patient cannot empty all of the urine from the bladder. Urinary retention can be acute (i.e., the sudden inability to urinate after receiving anesthesia during surgery) or chronic (i.e., a gradual inability to completely empty the bladder due to enlargement of the prostate gland in males). Urinary retention is caused by a blockage that prevents the flow of urine or the bladder not being able to create a strong enough force to expel all the urine. In addition to causing discomfort, urinary retention increases the patient’s risk for developing a urinary tract infection (UTI) or other complications. See Figure 5.14[15] for an image of an enlarged prostate gland blocking the flow of urine from the bladder into the urethra.
Symptoms of urinary retention can range from no symptoms to severe abdominal pain.[16] Health care providers use a patient’s medical history, physical exam findings, and diagnostic tests to determine the cause of urinary retention. Post-void residual (pōst voyd rĭ-ZĬD-ū-ăl) measurements can be taken when urinary retention is suspected by using a bladder scanner or inserting a catheter to determine how much urine is left in the bladder.[17]
Treatment for urinary retention depends on the cause. It may include urinary catheterization to drain the bladder, bladder training therapy, medications, or surgery.[18] A surgery called transurethral resection of the prostate (trăns-yū-RĒ-thrăl rĭ-SĔK-shŭn ăv thĕ PRŌS-tāt) (TURP) may be performed in males to treat urinary retention caused by an enlarged prostate that is not responsive to medication.
Urinary Tract Infection
A urinary tract infection (YŪR-ĭ-nĕr-ē trăkt ĭn-FĔK-shŭn) (UTI) is a common infection that occurs when bacteria, typically from the rectum, enter the urethra and infect the urinary tract. Infections can affect several parts of the urinary tract, but the most common type is a bladder infection, referred to as cystitis (sĭs-TĪ-tĭs). Kidney infections, referred to as pyelonephritis (pī-ĕl-ō-nĕ-FRĪ-tĭs), are more serious infections because they can have long-lasting effects on the kidneys.[19]
Some people are at higher risk of getting a UTI. UTIs are more common in females because their urethras are shorter and closer to the rectum, which makes it easier for bacteria to enter the urinary tract. Other factors that can increase the risk of UTIs include the following[20]:
- A previous UTI
- Sexual activity, especially with a new sexual partner
- Pregnancy
- Age (Older adults and young children are at higher risk.)
- Structural problems in the urinary tract, such as prostate enlargement
- Dehydration
- Uncontrolled diabetes
Symptoms of a UTI include the following[21]:
- Pain or burning while urinating (dysuria)
- Frequent urination (frequency)
- Urgency with small amounts of urine (oliguria)
- Bloody urine (hematuria)
- Pressure or cramping in the groin or lower abdomen
- Confusion or altered mental status in older adults
Symptoms of pyelonephritis include fever above 101 degrees F (38.3 degrees C), shaking chills, lower back pain or flank pain (i.e., on the sides of the back), and nausea or vomiting.[22] Older adults with a UTI may not exhibit these symptoms but often demonstrate an increased level of confusion. In some cases, UTIs can spread to the blood, leading to life-threatening infection called sepsis. Sepsis (SĔP-sĭs) occurs when the body’s infection-fighting processes work improperly and damage the organs. Sepsis may progress to septic shock, a dramatic drop in blood pressure that can damage the lungs, kidneys, liver, and other organs. When the damage is severe, it can lead to death. Early treatment of sepsis improves chances for survival.[23]
When a patient presents with symptoms of a UTI, the health care provider orders diagnostic tests that may include a urine dip, urinalysis, or urine culture & sensitivity. Read more about diagnostic tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section. Antibiotics are prescribed for urinary tract infections, and health teaching is provided to prevent future UTIs. Patients are also encouraged to drink extra fluids to help flush bacteria from the urinary tract.
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Acute Kidney Failure; [reviewed 2022, April 11]. https://medlineplus.gov/ency/article/000501.htm ↵
- Centers for Disease Control and Prevention. (2022, February 28). Chronic kidney disease basics. https://www.cdc.gov/kidneydisease/basics.html ↵
- Centers for Disease Control and Prevention. (2022, February 28). Chronic kidney disease basics. https://www.cdc.gov/kidneydisease/basics.html ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Glomerulonephritis; [reviewed 2021, July 27]. https://medlineplus.gov/ency/article/000484.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Hydronephrosis of One Kidney; [reviewed 2021, July 1]. https://medlineplus.gov/ency/article/000506.htm ↵
- “Kidney_stones_%28_renal_calculi_%29,_Бубрежни_камења_15.jpg” by Jakupica is licensed under CC BY-SA 4.0 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2016, Dec 8]. Kidney Stones; [cited 2023, Oct 12]. https://medlineplus.gov/kidneystones.html ↵
- National Kidney Foundation. (n.d.). Lithotripsy. https://www.kidney.org/atoz/content/lithotripsy ↵
- National Kidney Foundation. (n.d.). Percutaneous nephrolithotomy/nephrolithrotripsy. https://www.kidney.org/atoz/content/kidneystones_PNN ↵
- “Polycystic_kidneys,_gross_pathology_CDC_PHIL.png” by CDC/ Dr. Edwin P. Ewing, Jr. is licensed in the Public Domain. ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Polycystic Kidney Disease; [reviewed 2021, July 27]. https://medlineplus.gov/ency/article/000502.htm ↵
- National Cancer Institute. (2023, July 21). Renal cell cancer - PDQ patient version. National Institutes of Health. https://www.cancer.gov/types/kidney/patient/kidney-treatment-pdq#_1 ↵
- McClurg, D., Pollock, A., Campbell, P., Hazelton, C., Elders, A., Hagen, S., & Hill, D. C. (2016). Conservative interventions for urinary incontinence in women: An overview of Cochrane systematic reviews. The Cochrane Database of Systematic Reviews, 2016(9). https://doi.org/10.1002/14651858.CD012337 ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- “Normal-vs-enlarged-prostate.jpg” by Akcmdu9 is licensed under CC BY-SA 3.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Urinary retention. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-retention ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Urinary retention. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-retention ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Urinary retention. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-retention ↵
- Centers for Disease Control and Prevention. (2021, October 6). Urinary tract infection. https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/uti.html ↵
- Centers for Disease Control and Prevention. (2021, October 6). Urinary tract infection. https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/uti.html ↵
- Centers for Disease Control and Prevention. (2021, October 6). Urinary tract infection. https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/uti.html ↵
- Centers for Disease Control and Prevention. (2021, October 6). Urinary tract infection. https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/uti.html ↵
- Mayo Clinic. (2023). Sepsis. https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214 ↵

