12.6 Diseases and Disorders of the Digestive System
Common diseases and disorders of the digestive system are discussed in this section.
Celiac Disease
Celiac disease (SĒ-lē-ăk dĭ-ZĒZ) is a chronic digestive and autoimmune disease that damages the small intestine. It is triggered by eating foods containing gluten. Gluten is a protein found in foods containing wheat, barley, or rye. When a person with celiac disease eats gluten, an immune response is triggered to the gluten protein in the small intestine. Celiac disease can cause long-lasting digestive problems and prevent absorptions of nutrients. It is diagnosed with blood tests and biopsy taken during an upper GI endoscopy. Individuals with celiac disease must avoid gluten in their diets and often take dietary supplements.[1] Read more about upper GI endoscopy in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Digestive System” section.
Cholecystitis and Gallstones
Cholecystitis (kō-lĕ-sis-TĪT-ĭs) is inflammation of the gallbladder. The gallbladder stores and distributes bile through the bile ducts. A gallstone (GAWL-stōn) is a piece of hardened bile residue that can form for a variety of reasons, including elevated cholesterol levels. When a gallstone gets stuck in a bile duct, it can cause bile to back up into the gallbladder, causing severe upper right abdominal pain and swelling, chest pain, back pain, nausea, vomiting, and fever. The condition of having gallstones is cholelithiasis (kō-li-lith-Ī-ă-sĭs). See Figure 12.15[2] for an image of a gallstone in the gallbladder on an ultrasound. An inflamed gallbladder can be an urgent problem requiring immediate surgery or a slow response to long-term inflammation.[3]

Cholecystitis is diagnosed with blood tests and an abdominal ultrasound. To remove gallstones, a procedure called an endoscopic retrograde cholangiopancreatography (en-dŏ-SKOP-ik rĕ-trō-grād kō-LAN-jē-ō-pan-krē-ă-TŎG-ră-fē) (ERCP) may be performed that combines an upper endoscopy with X-ray technology. The doctor visualizes the biliary system and then removes gallstones during an endoscopy to relieve immediate symptoms. Cholecystectomy (kō-lĕ-sis-TEK-tŏ-mē) refers to surgery to remove the gallbladder to prevent repeat episodes of gallbladder inflammation, typically performed with a laparoscope (LAP-ă-rō-skōp), an instrument used to view the abdominal cavity.[4]
Cirrhosis
Cirrhosis (sĭr-RŌ-sĭs) is a serious, life-threatening condition where the liver becomes scarred and permanently damaged. The most common causes of cirrhosis are alcoholism and liver disease like hepatitis B or hepatitis C. Symptoms of cirrhosis may not appear until the liver is badly damaged and may include the following[5]:
- Fatigue and weakness
- Pruritis (itching of the skin)
- Poor appetite and weight loss without trying
- Nausea and vomiting
- Pain in the upper right side of the abdomen
- Easy bleeding and bruising
- Ascites (ă-SĪ-tēz), abdominal swelling due to fluid retention (See Figure 12.16[6] for an image of ascites.)
- Jaundice (JAWN-dĭs), yellowed discoloration of the skin and eyes.

Diagnostic testing for cirrhosis includes blood tests that evaluate liver function, liver ultrasound, CT scan, and liver biopsy. Treatment includes treating the cause of the cirrhosis, including treating infections and abstaining from alcohol.[7]
Colon Cancer
Colon cancer (KŌ-lŏn KAN-sĕr) is the third most common cancer diagnosed in people in the United States. It develops from polyps in the lining of the colon and typically affects people aged 50 years and older. Individuals can greatly reduce their risk for colon cancer by having regular screenings for polyps, including stool-based testing or a colonoscopy.[8] Read more about these tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Digestive System” section.
Risk factors for colon cancer include a personal or family history of colon polyps or colon cancer and inflammatory bowel disease like Crohn’s disease and ulcerative colitis. Early symptoms of colon cancer include blood in the stool and persistent bowel changes like diarrhea and constipation. Colon cancer is diagnosed with biopsies taken during a colonoscopy.[9]
Depending on the severity of colon cancer, there are many types of surgeries that may be performed[10]:
- Polypectomy (pŏl-ĭ-PĔK-tō-mē): Removal of polyps.
- Partial colectomy (pahr-shul kō-LEK-tŏ-mē), also called colon resection surgery (KŌ-lŏn rĭ-SĔK-shŭn SUR-jĕr-ē): The section of the colon containing the tumor is removed, and healthy colon sections are reattached in a procedure called anastomosis (ăn-ăs-tō-MŌ-sĭs).
- Colon resection with colostomy (KŌ-lŏn rĭ-SĔK-shŭn wĭth kŏl-ŌS-tŏ-mē): The section of the colon that contains the tumor is removed, but healthy colon sections cannot be reattached, so a colostomy is performed. In a colostomy (kŏ-LOS-tŏ-mē), the colon is attached to an opening in the abdominal wall called a stoma. Instead of eliminating feces through the anus, it is collected in an external bag.
- Radiofrequency ablation (RĀ-dē-ō-FRĒ-kwĕn-sē ă-blā-shŭn): Heat is used during a procedure to destroy cancer cells.
In addition to surgery, additional medical treatment may be required, such as chemotherapy or targeted therapy (treatment that targets the genes, proteins, and tissues that help colon cancer cells grow and multiply).[11]
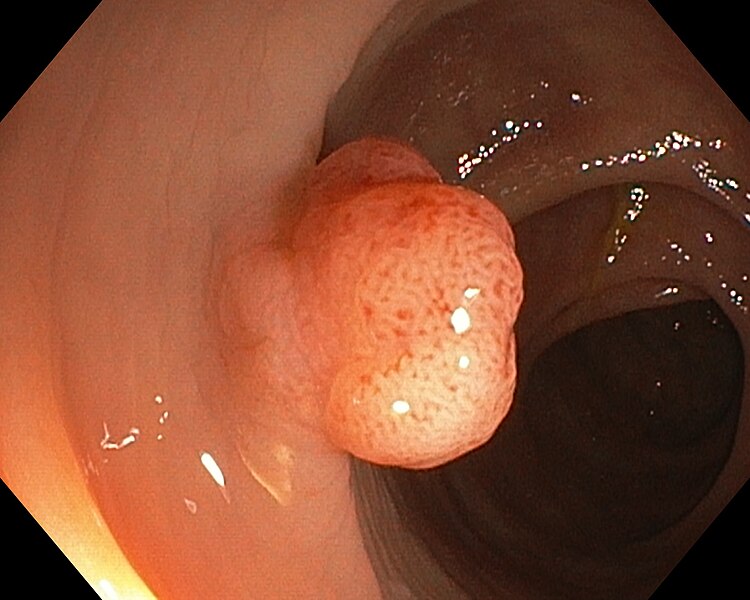
Colon Polyps
Colon polyps (KŌ-lŏn PŎL-ĭps) are growths on the inner lining of the colon and rectum. See Figure 12.17[12] for an image of a colon polyp seen on colonoscopy. Most polyps are not cancerous, but some may develop into colon cancer over time. Anyone can develop colon polyps. Risk factors for developing colon polyps are age of 50 years or older, personal or family history or colon polyps or colon cancer, obesity, and smoking. People can greatly reduce their risk for colon cancer if polyps are removed in a procedure called a polypectomy (pŏl-ĭ-PĔK-tō-mē). Read more about these tests in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Digestive System” section.
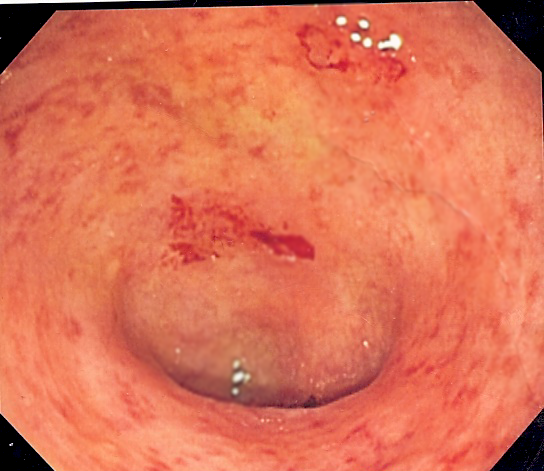
Crohn’s Disease and Ulcerative Colitis
Crohn’s disease (krōnz diz-ĒZ) and ulcerative colitis (UL-sĕr-ă-tiv kō-LĪ-tĭs) are chronic inflammatory bowel diseases (IBD) that cause inflammation and ulcers in the digestive tract. See Figure 12.18[13] for an image of ulcerative colitis on a colonoscopy, illustrating how the internal surface of the colon is blotchy and broken in places. Symptoms include abdominal pain, diarrhea, weight loss, and fatigue. These diseases are typically diagnosed with procedures like upper GI endoscopy, colonoscopy, and upper GI series.[14] Read more about these procedures in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Digestive System” section.
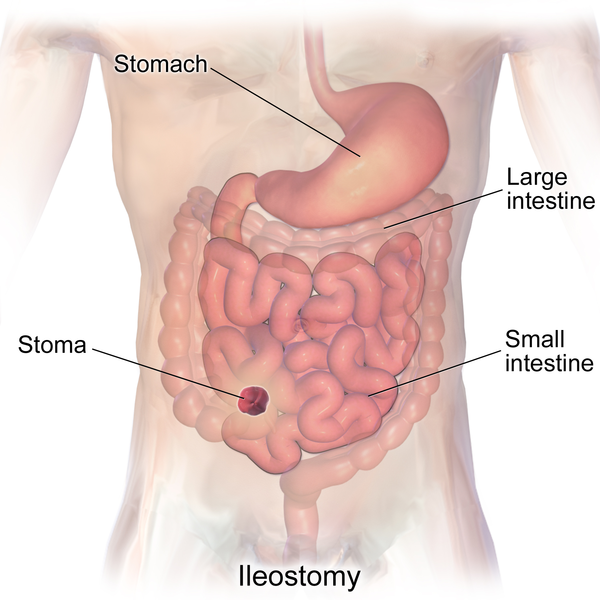
Crohn’s disease and ulcerative colitis are treated with medications, bowel rest, and surgery. No single treatment works for everyone with Crohn’s disease. The goals of treatment are to decrease the inflammation in the intestines and prevent flare-ups of symptoms. Surgery may include small bowel resection (SMOL BOW-ĕl rĭ-SĔK-shŭn) or large bowel resection (LARJ BOW-ĕl rĭ-SĔK-shŭn), where part of the bowel is removed. In severe cases, proctocolectomy (prŏk-tō-kō-LEK-tŏ-mē) is performed where the entire colon and rectum are removed. An ileostomy (IL-ē-OS-tŏ-mē) is created, where part of the ileum is brought through an artificial opening in the abdomen called a stoma (STŌ-mă). A removable external collection pouch, called an ostomy appliance (ŎS-tŏ-mē ă-PLĪ-ăns), connects to the stoma and collects stool instead of it passing through the anus.[15] See Figure 12.19[16] for an illustration of an ileostomy and a stoma.
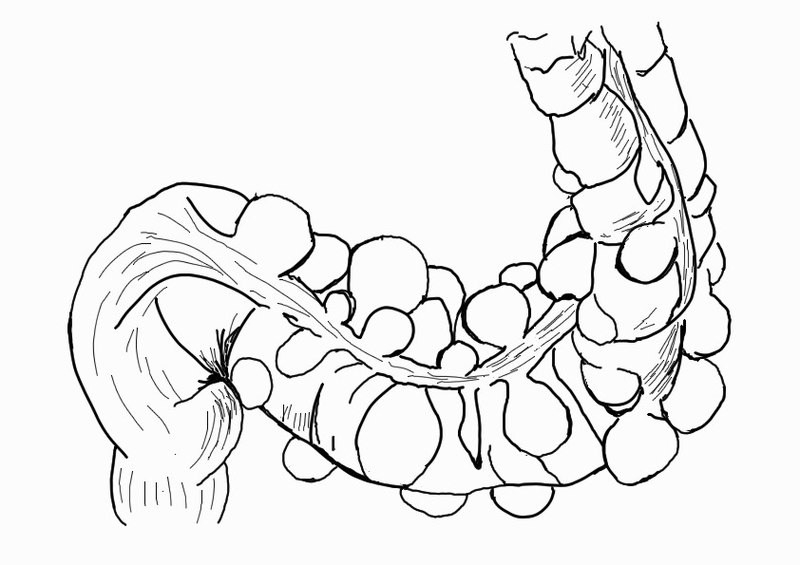
Diverticulosis and Diverticulitis
Diverticula (dī-vĕr-TIK-yū-lă) are small, bulging pouches that form in the lower part of the large intestine (colon). Diverticula are common, especially after age 40, and seldom cause problems. The presence of diverticula is known as diverticulosis (dī-vĕr-tik-yŭ-LŌ-sĭs). See Figure 12.20[17] for an illustration of diverticulosis. If one or more of the pouches become inflamed or infected, this condition is called diverticulitis (dī-vĕr-tik-yŭ-LĪT-ĭs). Diverticulitis can cause severe abdominal pain, fever, nausea, and a change in bowel habits. Diverticulitis is diagnosed with a CT scan, which can identify inflamed or infected pouches. Mild diverticulitis can be treated with rest, diet changes, and antibiotics. Severe or recurring diverticulitis may require bowel resection surgery.[18]
Esophageal Cancer
Esophageal cancer (ĭ-sŏf-ă-JĒ-ăl KAN-sĕr) starts in the tissues of the esophagus. Tumors caused by esophageal cancer may not cause noticeable symptoms until the cancer has spread. As the tumor grows, it starts to block the esophagus, and the person may have trouble swallowing or notice that it hurts to swallow. Esophageal cancer typically affects men who are age 60 or older and grows and spreads rapidly. Risk factors include tobacco use, alcohol use, obesity, chronic gastroesophageal reflux disease, and Human papillomavirus (HPV). Diagnostic tests include an upper GI series or upper GI endoscopy with biopsy. An esophagectomy (ĕ-sŏf-ă-JĔK-tŏ-mē) is the most common treatment for early-stage esophageal cancer. It involves removing some or most of the esophagus and creating a new esophagus by pulling up part of the stomach into the chest and neck. Chemotherapy, radiation, targeted therapy, and immunotherapy are also commonly prescribed treatments.[19]
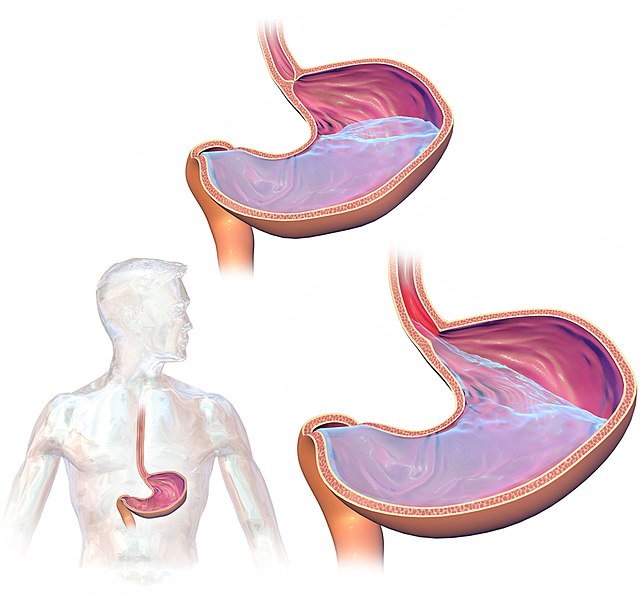
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GAS-trō-ĕ-sŏf-ă-JĒ-ăl REE-flŭks dĭ-ZĒZ) (GERD) occurs when stomach acid repeatedly flows back into the esophagus from the stomach. The acid irritates the lining of the esophagus and causes an ulcer. See Figure 12.21[20] for an illustration of GERD and backup of acid into the esophagus. GERD is typically diagnosed with a procedure called an upper GI endoscopy. Most people are able to manage the discomfort of GERD with lifestyle changes and medications.[21] Read more about upper GI endoscopy in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Digestive System” section.
Hepatitis
Hepatitis (hep-ă-TĪT-ĭs) is a general term used to describe inflammation of the liver. Liver inflammation can be caused by several viruses (such as hepatitis B and hepatitis C), drugs, excessive alcohol intake, genetic disorders, or by an overactive immune system that mistakenly attacks the liver, called autoimmune hepatitis. Symptoms include right upper quadrant abdominal pain, jaundice, light-colored stools, dark colored urine, fatigue, nausea, vomiting, and ascites (abdominal swelling due to fluid retention). See Figure 12.22[22] for an image of jaundice. Hepatitis is diagnosed with blood tests, ultrasound of the liver, and liver biopsy. Treatment focuses on preventing further damage to the liver and cirrhosis.[23]

Hernia
A hernia occurs when an organ or fatty tissue squeezes through a weak spot in a surrounding muscle or connective tissue. A hiatal hernia (hī-Ā-tăl HĔR-nē-ă) is a condition in which the upper part of the stomach bulges through an opening in the diaphragm. A large hiatal hernia can cause acid to back up into the esophagus, causing gastroesophageal reflux disorder (GERD). Medications usually resolve the GERD symptoms, but very large hiatal hernias may require surgery.[24]
Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (ĬR-ĭ-tă-bl BOWL SĬN-drōm) (IBS) is a group of symptoms that occur together, including repeated pain in the abdomen and changes in bowel movements, which may be diarrhea, constipation, or both. Individuals with IBS have these symptoms without any visible signs of damage or disease in the digestive tract. Health care providers diagnose IBS based on a medical history and physical exam. Diagnostic testing, like upper GI endoscopy and colonoscopy, may be performed to rule out other conditions. IBS is treated with diet changes.[25]
Pancreatitis
Pancreatitis (pan-krē-a-TĪT-ĭs) is inflammation of the pancreas. Pancreatitis can be an acute or chronic condition. Acute pancreatitis appears suddenly and lasts a short time. Chronic pancreatitis is a long-term condition, and the damage to the pancreas can get worse over time. Pancreatitis can be caused by blockage in the bile duct caused by gallstones, heavy alcohol use, diabetes, and pancreatic cancer. However, sometimes a cause is never found. Severe pancreatitis requires treatment in a hospital and can cause life-threatening complications.[26]
Peptic Ulcer Disease
Peptic ulcer disease (PĔP-tĭk UL-sĕr dĭ-ZĒZ) (PUD) refers to ulcers in the stomach lining (gastric ulcers) or the duodenum (duodenal ulcers). See Figure 12.23[27] for an image of an ulcer on an upper endoscopy. PUD can cause complications such as bleeding, perforation, or blockage in the stomach or duodenum. A common symptom of PUD is pain in the upper part of the abdomen. Common causes of PUD are Helicobacter pylori (H. pylori) infection and use of nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, ibuprofen, and naproxen.[28]
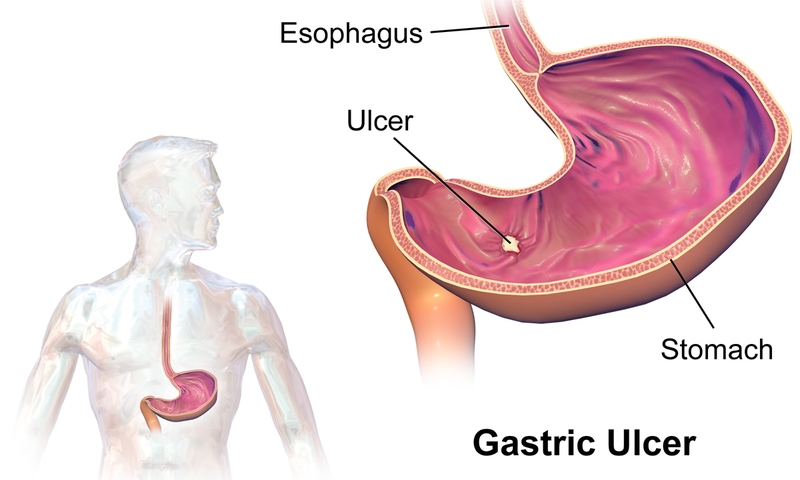
Common diagnostic tests for PUD include blood tests for H. pylori, a urea breath test, an upper GI endoscopy, or an upper GI series. In a urea breath test (yŏŏ-RĒ-ă brĕth tĕst), the patient swallows a capsule, liquid, or pudding that contains urea that is “labeled” with a special carbon atom. If H. pylori is present, the bacteria convert the urea into carbon dioxide. After a few minutes, the patient breathes into a container, exhaling carbon dioxide. The exhaled breath is evaluated by a medical lab technician. If the test detects the labeled carbon atoms, an H. pylori infection is confirmed.[29] Read more about upper GI endoscopy and upper GI series in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Digestive System” section.
Peritonitis
Peritonitis (per-ĭt-ŏ-NĪT-ĭs) refers to inflammation of the peritoneum, the tissue that lines the inside of the abdominal cavity. It is typically caused by an infection or by leakage of body fluids from one of the abdominal organs (such as an inflamed appendix, intestine, pancreas, or gallbladder). Infection of the peritoneum is especially dangerous because it can impact the functioning of the abdominal organs and also transfer bacteria to the bloodstream where it can cause a life-threatening infection called sepsis. Health care providers treat peritonitis as an emergency because it can become severe very quickly. It is treated with intravenous antibiotics. Common symptoms of peritonitis are as follows[30]:
- Mild to severe abdominal pain with sensitivity to touch
- Swollen, distended abdomen
- Paralytic ileus (păr-ă-LĬT-ĭk Ī-lē-ŭs), which is when the bowels become temporarily paralyzed
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Celiac disease. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease ↵
- “Gallstone_in_neck_of_Gallbladder_on_CT.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- Cleveland Clinic. (2023, September 21). Cholecystitis. https://my.clevelandclinic.org/health/diseases/15265-gallbladder-swelling--inflammation-cholecystitis ↵
- Cleveland Clinic. (2023, September 21). Cholecystitis. https://my.clevelandclinic.org/health/diseases/15265-gallbladder-swelling--inflammation-cholecystitis ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Cirrhosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis ↵
- “16650267836_eda1d47696_k.jpg” by John Campbell is licensed in the Public Domain. ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Cirrhosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis ↵
- Cleveland Clinic. (2022, November 14). Colorectal (colon) cancer. https://my.clevelandclinic.org/health/diseases/14501-colorectal-colon-cancer ↵
- Cleveland Clinic. (2022, November 14). Colorectal (colon) cancer. https://my.clevelandclinic.org/health/diseases/14501-colorectal-colon-cancer ↵
- Cleveland Clinic. (2022, November 14). Colorectal (colon) cancer. https://my.clevelandclinic.org/health/diseases/14501-colorectal-colon-cancer ↵
- Cleveland Clinic. (2022, November 14). Colorectal (colon) cancer. https://my.clevelandclinic.org/health/diseases/14501-colorectal-colon-cancer ↵
- “600H0019.jpg” by Vivat.iden is licensed under CC BY-SA 4.0 ↵
- “UC_granularity.png” by unknown author is licensed under CC BY-SA 3.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Crohn's disease. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Crohn's disease. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease ↵
- “Ileostomy.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Sigmoid_diverticulum_(diagram).jpg” by Anpol42 is licensed under CC BY-SA 4.0 ↵
- Mayo Clinic. (2022, April 19). Diverticulitis. https://www.mayoclinic.org/diseases-conditions/diverticulitis/symptoms-causes/syc-20371758 ↵
- Cleveland Clinic. (2022, September 6). Esophageal cancer. https://my.clevelandclinic.org/health/diseases/6137-esophageal-cancer ↵
- “GastroEsophageal_Reflux_Disease_(GERD).jpg” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020, July). Diagnosis of GER & GERD. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/diagnosis ↵
- “Scleral_Icterus.jpg” by Sheila J. Toro is licensed under CC BY 4.0 ↵
- Johns Hopkins Medicine. (n.d.). Hepatitis. https://www.hopkinsmedicine.org/health/conditions-and-diseases/hepatitis ↵
- Mayo Clinic. (2021, February 23). Hiatal hernia. https://www.mayoclinic.org/diseases-conditions/hiatal-hernia/symptoms-causes/syc-20373379 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Irritable bowel syndrome. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome ↵
- Mayo Clinic. (2023, September 23). Pancreatitis. https://www.mayoclinic.org/diseases-conditions/pancreatitis/symptoms-causes/syc-20360227 ↵
- “Gastric_Ulcer.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Peptic ulcers (stomach and duodenal ulcers). National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Peptic ulcers (stomach and duodenal ulcers). National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers ↵
- Cleveland Clinic. (2022, November 2). Peritonitis. https://my.clevelandclinic.org/health/diseases/17831-peritonitis ↵

