5.5 Physiology of the Urinary System
The kidneys filter all the blood in your body every 30 minutes and create urine. They remove waste products and excess fluid and also regulate electrolytes and hormones that control blood pressure, stimulate production of red blood cells, and keep bones healthy.[1]
Filtration, Reabsorption, and Secretion
As previously discussed in “Anatomy of the Urinary System,” blood enters the kidneys via the renal arteries and is filtered by nephrons, where many functions take place. Three principal functions of the nephron are filtration, reabsorption, and secretion. Secondary functions of the nephron include controlling blood pressure (via the production of renin), producing red blood cells (via the hormone erythropoietin), and absorbing calcium.[2]
The initial filtering of the blood takes place in the glomerulus, a cluster of capillaries surrounded by the glomerular capsule within the nephron. The renal tubule receives this filtered fluid, called glomerular filtrate, and electrolytes and water are reabsorbed in different parts of the renal tubule and returned to circulation. The final end product of the filtered fluid is urine.[3]
Glomerular Filtration
The first step in urine production is glomerular filtration (glō-MER-yū-lăr fĭl-TRĀ-shŭn). In this process, water and most of the solutes in the blood pass through the wall of glomerular capillaries into the glomerular capsule and then into the renal tubule. This process filters the blood and creates a filtrate that does not contain blood cells or large proteins, referred to as glomerular filtrate.[4]
The volume of filtrate formed by both kidneys per minute is called the glomerular filtration rate (glō-MER-yū-lăr fĭl-TRĀ-shŭn rāt) (GFR). GFR is used to assess how well the kidneys are functioning. The heart pumps about five liters of blood per minute when a person is resting, and approximately 20 percent of this (i.e., one liter) enters the kidneys to be filtered per minute. On average, this results in the production of about 115 mL/min of filtrate produced by the nephrons. However, 99 percent of this filtrate is returned to the circulation by reabsorption so that only about 1–2 liters of urine are produced per day.[5]
GFR is influenced by hydrostatic pressure, osmotic pressure, and oncotic pressures. Hydrostatic (hī-drō-STAT-ik) pressure refers to the pressure produced by a fluid against a surface. Glomerular filtration occurs as hydrostatic pressure forces fluid and solutes through the semipermeable barrier of the glomerular capillary membrane. The movement of solutes out of the blood is limited by their size. Glomerular filtration occurs when glomerular capillary hydrostatic pressure exceeds the luminal hydrostatic pressure of glomerular capsule.[6] See Figure 5.8[7] for an illustration of hydrostatic pressure in a capillary.
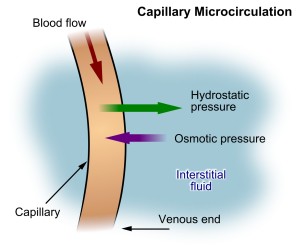
Another force, called osmotic pressure, also controls the movement of water. Osmosis (ŏz-MŌ-sĭs) refers to the movement of water across a semipermeable membrane that is impermeable to a solute. As long as the concentration of water differs on both sides, water will move in the direction of lower pressure until the osmotic pressure on both sides of the membrane is equal. For this reason, a proper concentration of solutes in the blood is important in maintaining osmotic pressure in the glomerulus, as well as systemically throughout the body.[8]
A third force, called oncotic pressure (ŏn-KŎT-ĭk PRĔSH-ŭr), is created by the protein content of the blood that helps holds water inside of capillaries. There are urinary system disorders in which too much protein passes through during filtration into the glomerular filtrate. This excess protein in the filtrate leads to a deficiency of circulating proteins in the blood. In turn, the presence of excess protein in the urine allows it to retain more water in the filtrate and results in an increase in urine volume. Because there is less circulating protein in the blood (principally albumin), the osmotic pressure of the blood also falls. Less osmotic pressure tips the balance towards hydrostatic pressure, which causes water to be pushed out of the capillaries. The net effect is that water is lost from the circulation into interstitial tissues and cells. This “plumps up” the tissues and cells, a condition called edema (ĭ-DĒ-mă) or puffy, swollen tissue due to accumulation of fluid.[9]
Tubular Reabsorption and Secretion
After glomerular filtration, the filtrate continues to undergo modification through secretion and reabsorption in the renal tubules before urine is produced and collected in the collecting ducts. During this process, some substances are reabsorbed, whereas others are secreted. In fact, 99 percent of the water and most of the solutes that were filtered out during glomerular filtration are reabsorbed in the tubules. A blood vessel runs alongside the tubule. As the filtered fluid moves along the tubule, a blood vessel reabsorbs almost all of the water, along with minerals and nutrients the body needs, and returns them to the body via the renal vein. The remaining fluid and wastes in the tubule become urine.[10]
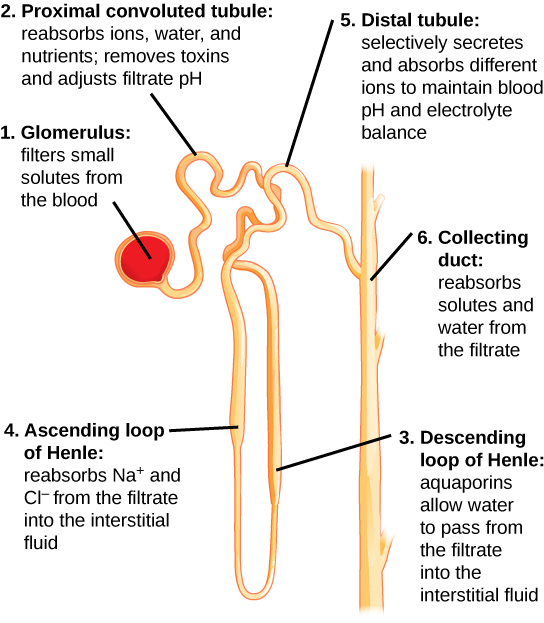
See Figure 5.9[11] for an illustration of nephron structure. The glomerulus (1) filters small solutes from the blood. The proximal tubule (2) reabsorbs 60-70% of the sodium and water back into the bloodstream. From the proximal tubule, the filtrate flows into the descending loop of Henle (3) and then into the ascending loop of Henle (4). Another 20-25% of sodium is reabsorbed in the ascending loop of Henle. Filtrate then enters the distal tubule (5), where sodium is actively filtered in exchange for potassium or hydrogen ions to maintain blood pH and electrolyte balance, a process regulated by the hormone aldosterone. The collecting duct (6) is the final pathway where antidiuretic hormone (ADH) acts to further reabsorb water and solutes back into the bloodstream, thereby preventing it from being eliminated in urine.[12]
Imbalances Resulting From Nephron Damage
Several diseases and disorders can damage the kidneys and the nephrons. When nephrons are damaged, their ability to filter, reabsorb, and secrete substances is affected. Two common symptoms of kidney disease include fluid retention (causing edema) and hyperkalemia (hī-pĕr-kă-LĒM-ē-ă) or increased levels of potassium in the blood due to a reduced inability to reabsorb these substances.
Urine
Urine volume varies considerably by individual, based on several factors such as fluid intake, perspiration, and disorders affecting the urinary system. The normal range of urine output for adults is one to two liters per day. The kidneys must produce a minimum urine volume of about 500 mL/day to adequately rid the body of wastes. Urine output below this level can be caused by severe dehydration or kidney disease.[13]
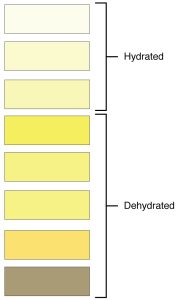
Urine color and odor are affected by many conditions and even the food the person has eaten. For example, a urinary tract infection or kidney stone may cause bleeding, resulting in pink or even bright red urine. Dehydration produces darker, concentrated urine. See Figure 5.10[14] for an illustration of the color of urine based on the patient’s hydration status. Additionally, about one in five people detect a distinctive odor in their urine after consuming asparagus; other foods such as onions, garlic, and fish can impart their own aromas. These food-caused odors are harmless.[15]
Urea
Urea (yū-RĒ-ă) nitrogen is a waste product made when the liver breaks down protein into amino acids, and then deamination (dē-am-ĭ-NĀ-shŏn) converts the amino acids into ammonia, urea, or uric acid. Urea is transported in the blood, filtered out by the kidneys, and eliminated from the body in urine. Urine primarily contains urea with small amounts of ammonia and uric acid. When damage occurs to the nephrons, urea is filtered out less efficiently, and a buildup of urea in the blood can occur.[16] For this reason, a diagnostic test called blood urea nitrogen (BUN) provides important information about kidney function and is further discussed in the “Medical Specialists, Diagnostic Testing, and Procedures Related to the Urinary System” section.
Most of the ammonia produced from the breakdown of protein in the body is converted into urea by the liver, so the odor of ammonia is rarely detected in fresh urine. The strong ammonia odor that can sometimes be detected in bathrooms is due to the breakdown of urea into ammonia by bacteria in the environment.[17]
Diuretics
A diuretic (dī-ū-RĒT-ĭk) is a substance that increases urine production. Three common beverages contain diuretic compounds: coffee, tea, and alcohol. The caffeine in coffee and tea works by promoting vasodilation in the nephron, which increases GFR. Alcohol increases GFR by inhibiting ADH release from the posterior pituitary, resulting in less water recovery by the collecting duct. Medications called diuretics are prescribed to individuals with high blood pressure to reduce blood volume and, thereby, reduce blood pressure.[18]
Other Terms Related to Urine and Urination
Terms commonly used to document urine and urination are as follows:
- Anuria (ă-NOOR-ē-ă): Absence of urine output, typically found during kidney failure, defined as less than 50 mL of urine over a 24-hour period.
- Diuresis (dī-ū-RĒ-sĭs): Increased production of urine.
- Dysuria (dĭs-ŪR-ē-ă): Painful or difficult urination.
- Enuresis (en-ū-RĒ-sĭs): Involuntary urination, especially by children at night.
- Frequency (FRĒ-kwĕn-sē): The need to urinate several times during the day or at night (nocturia) in normal or less-than-normal volumes. It may be accompanied by a feeling of urgency.[19]
- Hematuria (hē-mă-TŪR-ē-ă): Blood in the urine, either visualized or found during microscopic analysis.
- Oliguria (ŏ-lĭ-GŪR-ē-ă): Decreased urine output, defined as less than 500 mL of urine in adults in a 24-hour period.
- Nocturia (nŏk-TŪR-ē-ă): The need to get up at night on a regular basis to urinate. Nocturia often causes sleep deprivation that affects a person’s quality of life.[20]
- Polyuria (pŏl-ē-ŪR-ē-ă): Greater than 2.5 liters of urine output over 24 hours, also referred to as diuresis.[21] New polyuria should be reported to the health care provider because it can be a sign of many medical conditions.
- Pyuria (pī-ŪR-ē-ă): White blood cells in a urine sample indicating infection. In severe infections, pus may be visible in the urine.[22] See Figure 5.11[23] for an image of pyuria.
- Urgency (ŬR-jĕn-sē): A sensation of an urgent need to void.[24] Urgency can cause urge incontinence if the patient is not able to reach the bathroom quickly.
- Urinal (Ū-rĭn-ăl): A receptacle used for urine collection in health care facilities.

View the following YouTube video about the urinary system: Urinary System, Part 2: Crash Course Anatomy & Physiology #39[25]
- Centers for Disease Control and Prevention. (2022, February 28). Chronic kidney disease basics. https://www.cdc.gov/kidneydisease/basics.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020, June). The urinary tract & how it works. National Institutes of Health. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works ↵
- Anatomy & Physiology by CCCOnline is licensed under CC BY-SA ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Capillary_microcirculation.jpg” by Kes47 is in the Public Domain ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Figure 41 03 04.jpg” by CNX OpenStax is licensed under CC BY 4.0 ↵
- McCuistion, L., Vuljoin-DiMaggio, K., Winton, M., & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 443-454. Elsevier. ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2601_Urine_Color_Chart.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Maddukuri, G. (2021, January). Urinary frequency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/symptoms-of-genitourinary-disorders/urinary-frequency ↵
- This work is a derivative of StatPearls by Leslie, Sajjad, & Singh and is licensed under CC BY 4.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Urination - excessive amount; [updated 2021, Feb 8; cited 2021, Feb 16]. https://medlineplus.gov/ency/article/003146.htm ↵
- Cherney, K. (2018, August 30). Everything you should know about pyuria. Healthline. https://www.healthline.com/health/pyuria ↵
- “Pyuria2011.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- Maddukuri, G. (2021, January). Urinary frequency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/symptoms-of-genitourinary-disorders/urinary-frequency ↵
- CrashCourse. (2015, October 19).Urinary system, Part 2: Crash Course Anatomy & Physiology #39 [Video]. YouTube. All rights reserved. https://youtu.be/DlqyyyvTI3k?si=Pf8-lEPgHQJTLHAa ↵

