5.2 Basic Safety Concepts
Open Resources for Nursing (Open RN)
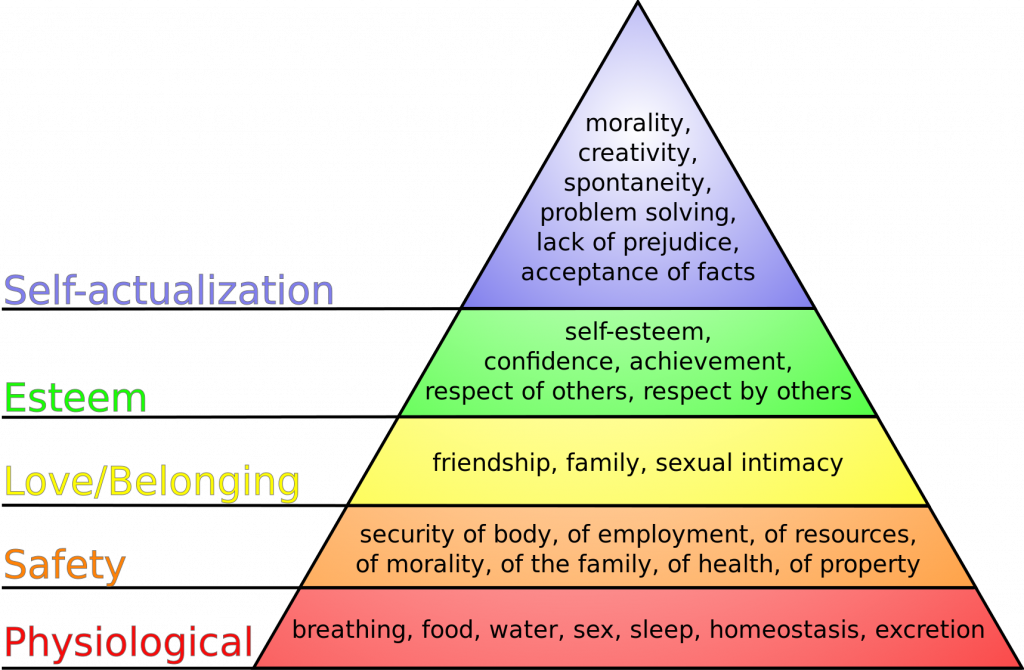
Safety: A Basic Need
Safety is a basic foundational human need and always receives priority in client care. Nurses typically use Maslow’s Hierarchy of Needs to prioritize urgent client needs, with the bottom two rows of the pyramid receiving top priority. See Figure 5.1[1] for an image of Maslow’s Hierarchy of Needs. Safety is intertwined with basic physiological needs.
Consider the following scenario: You are driving back from a relaxing weekend at the lake and come upon a fiery car crash. You run over to the car to help anyone inside. When you get to the scene, you notice that the lone person in the car is not breathing. Your first priority is not to initiate rescue breathing inside the burning car, but to move the person to a safe place where you can safely provide CPR.
In nursing, the concept of client safety is central to everything we do in all health care settings. As a nurse, you play a critical role in promoting client safety while providing care. You also teach clients and their caregivers how to prevent injuries and remain safe in their homes and in the community. Safe client care also includes measures to keep you safe in the health care environment; if you become ill or injured, you will not be able to effectively care for others.
Safe client care is a commitment to providing the best possible care to every client and their caregivers in every moment of every day. Clients come to health care facilities expecting to be kept safe while they are treated for illnesses and injuries. Unfortunately, you may have heard stories about situations when that did not happen. Medical errors can be devastating to clients and their families. Consider the true story in the following box that illustrates factors affecting client safety.
The Josie King Story
In 2001, 18-month-old Josie King died as a result of medical errors in a well-known hospital from a hospital-acquired infection and an incorrectly administered pain medication. How did this preventable death happen? Watch this video of her mother, Sorrel King, telling Josie’s story and explaining how Josie’s death spurred her work on improving client safety in hospitals everywhere.[2]
Reflective Questions:
- What factors contributed to Josie’s death?
- How could these factors be resolved?
Never Events
The event described in the Josie King story is considered a “never event.” Never events are adverse events that are clearly identifiable, measurable, serious (resulting in death or significant disability), and preventable. In 2007 the Centers for Medicare and Medicaid Services (CMS) discontinued payment for costs associated with never events, and this policy has been adopted by most private insurance companies. Never events are publicly reported, with the goal of increasing accountability by health care agencies and improving the quality of client care. The current list of never events includes seven categories of events:
- Surgical or procedural event, such as surgery performed on the wrong body part
- Product or device, such as injury or death from a contaminated drug or device
- Client protection, such as client suicide in a health care setting
- Care management, such as death or injury from a medication error
- Environmental, such as death or injury as the result of using restraints
- Radiologic, such as a metallic object in an MRI area
- Criminal, such as death or injury of a client or staff member resulting from physical assault on the grounds of a health care setting
Sentinel Events
Sentinel events are very similar to never events although they may not be entirely preventable. They are defined by The Joint Commission as an “A client safety event that reaches a client and results in death, permanent harm, or severe temporary harm requiring interventions to sustain life.” Such events are called “sentinel” because they signal the need for immediate investigation and response. Each accredited organization is strongly encouraged, but not required, to report sentinel events to The Joint Commission.[3] It is helpful to facilities to self-report sentinel events so that other facilities can learn from these events and future sentinel events can be prevented through knowledge sharing and risk reduction. Investigations into sentinel events are typically achieved through a process called root cause analysis.
Root cause analysis is a structured method used to analyze serious adverse events to identify underlying problems that increase the likelihood of errors, while avoiding the trap of focusing on mistakes by individuals. A multidisciplinary team analyzes the sequence of events leading up to the error with the goal of identifying how and why the event occurred. The ultimate goal of root cause analysis is to prevent future harm by eliminating hidden problems within a health care system that contribute to adverse events. For example, when a medication error occurs, a root cause analysis goes beyond focusing on the mistake by the nurse and looks at other system factors that contributed to the error, such as similar-looking drug labels, placement of similar-looking medications next to each other in a medication dispensing machine, or vague instructions in a provider order.
Root cause analysis uses human factors science as part of the investigation. Human factors focus on the interrelationships among humans, the tools and equipment they use in the workplace, and the environment in which they work. Safety in health care is ultimately dependent on humans – the doctors, nurses, and health care professionals – providing the care.
Near Misses
In addition to investigating sentinel events and never events, agencies use root cause analysis to investigate near misses. Near misses are defined by the World Health Organization (WHO) as, “An error that has the potential to cause an adverse event (client harm) but fails to do so because of chance or because it is intercepted.” Errors and near misses are rarely the result of poor motivation or incompetence of the health care professional but are often caused by key contributing factors such as poor communication, less-than-optimal teamwork, memory overload, reliance on memory for complex procedures, and lack of standardization of policies and procedures. In an effort to prevent near misses, medical errors, sentinel events, and never events, several safety strategies have been developed and implemented in health care organizations across the country. These strategies will be discussed throughout the remainder of the chapter.
Incident Reports and Client Safety
Recall from the previous discussion in Chapter 2.5 that an incident report is a specific type of documentation performed when there is an error, near miss, or other unexpected occurrence that occurs during client care. Incident reports are used to identify process problems or other areas that could benefit from safety and quality improvement and are not included in the client’s medical record. They are a component of an agency’s culture of safety and are used during investigations like root cause analysis to help improve the safety and quality of client care.
- “Maslow's hierarchy of needs.svg” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
- Healthcare.gov. (2011, May 25). Introducing the partnerships for patients with Sorrel King [Video]. YouTube. https://youtu.be/ak_5X66V5Ms ↵
- The Joint Commission. (2024). Sentinel event. https://www.jointcommission.org/resources/sentinel-event/ ↵
Adverse events that are clearly identifiable, measurable, serious (resulting in death or significant disability), and preventable.
A client safety event that reaches a client and results in death, permanent harm, or severe temporary harm requiring interventions to sustain life.
A structured method used to analyze serious adverse events to identify underlying problems that increase the likelihood of errors, while avoiding the trap of focusing on mistakes by individuals.
A science that focuses on the interrelationships between humans, the tools and equipment they use in the workplace, and the environment in which they work.
An error that has the potential to cause an adverse event (client harm) but fails to do so because of chance or because it is intercepted.

