3.2 Diverse Patients Basic Concepts
Open Resources for Nursing (Open RN)
Let’s begin the journey of developing cultural competency by exploring basic concepts related to culture.
Culture and Subculture
Culture is a set of beliefs, attitudes, and practices shared by a group of people or community that is accepted, followed, and passed down to other members of the group. The word “culture” may at times be interchanged with terms such as ethnicity, nationality, or race. See Figure 3.1[1] for an illustration depicting culture by various nationalities. Cultural beliefs and practices bind group or community members together and help form a cohesive identity.[2],[3] Culture has an enduring influence on a person’s view of the world, expressed through language and communication patterns, family connections and kinship, religion, cuisine, dress, and other customs and rituals.[4] Culture is not static but is dynamic and ever-changing; it changes as members come into contact with beliefs from other cultures. For example, sushi is a traditional Asian dish that has become popular in America in recent years.

Nurses and other health care team members are impacted by their own personal cultural beliefs. For example, a commonly held belief in American health care is the importance of timeliness; medications are administered at specifically scheduled times, and appearing for appointments on time is considered crucial.
Most cultural beliefs are a combination of beliefs, values, and habits that have been passed down through family members and authority figures. The first step in developing cultural competence is to become aware of your own cultural beliefs, attitudes, and practices.
Nurses should also be aware of subcultures. A subculture is a smaller group of people within a culture, often based on a person’s occupation, hobbies, interests, or place of origin. People belonging to a subculture may identify with some, but not all, aspects of their larger “parent” culture. Members of the subculture share beliefs and commonalities that set them apart and do not always conform with those of the larger culture. See Table 3.2a for examples of subcultures.
Table 3.2a Examples of Subcultures
| Age/Generation | Baby Boomers, Millennials, Gen Z |
|---|---|
| Occupation | Truck Driver, Computer Scientist, Nurse |
| Hobbies/Interests | Birdwatchers, Gamers, Foodies, Skateboarders |
| Religion | Hinduism, Baptist, Islam |
| Gender | Male, Female, Nonbinary, Two-Spirit |
| Geography | Rural, Urban, Southern, Midwestern |
Culture is much more than a person’s nationality or ethnicity. Culture can be expressed in a multitude of ways, including the following:
- Language(s) spoken
- Religion and spiritual beliefs
- Gender identity
- Socioeconomic status
- Age
- Sexual orientation
- Geography
- Educational background
- Life experiences
- Living situation
- Employment status
- Immigration status
- Ability/Disability
People typically belong to more than one culture simultaneously. These cultures overlap, intersect, and are woven together to create a person’s cultural identity. In other words, the many ways in which a person expresses their cultural identity are not separated, but are closely intertwined, referred to as intersectionality.
Assimilation
Assimilation is the process of adopting or conforming to the practices, habits, and norms of a cultural group. As a result, the person gradually takes on a new cultural identity and may lose their original identity in the process.[5] An example of assimilation is a newly graduated nurse, who after several months of orientation on the hospital unit, offers assistance to a colleague who is busy. The new nurse has developed self-confidence in the role and has developed an understanding that helping others is a norm for the nurses on that unit.
Assimilation is not always voluntary, however, and may become a source of distress. There are historic examples of involuntary assimilation in many countries. For example, in the past, authorities in the United States and Canadian governments required indigenous children to attend boarding schools, separated them from their families, and punished them for speaking their native language.[6],[7]
Cultural Values and Beliefs
Culture provides an important source of values and comfort for patients, families, and communities. Think of culture as a thread that is woven through a person’s world and impacts one’s choices, perspectives, and way of life. It plays a role in all of a person’s life events and threads its way through the development of one’s self-concept, sexuality, and spirituality. It affects lifelong nutritional habits, as well as coping strategies with death and dying.
Culture influences how a patient interprets “good” health, as well as their perspectives on illness and the causes of illness. The manner in which pain is expressed is also shaped by a person’s culture. See Table 3.2b for additional examples of how a person’s culture impacts common values and beliefs regarding family patterns, communication patterns, space orientation, time orientation, and nutritional patterns. As you read Table 3.2b, take a moment to reflect on your own cultural background and your personally held beliefs for each of these concepts.
Table 3.2b Cultural Concepts
| Cultural Concepts | Examples of Culturally Influenced Values and Beliefs |
|---|---|
| Family Patterns | Family size Views on contraception Roles of family members Naming customs Value placed on elders and children Discipline/upbringing of children Rites of passage End-of-life care |
| Communication Patterns | Eye contact Touch Use of silence or humor Intonation, vocabulary, grammatical structure Topics considered personal (i.e., difficult to discuss) Greeting customs (handshakes, hugs) |
| Space Orientation | Personal distance and intimate space |
| Time Orientation | Focus on the past, present, or future Importance of following a routine or schedule Arrival on time for appointments |
| Nutritional Patterns | Common meal choices Foods to avoid Foods to heal or treat disease Religious practices (e.g., fasting, dietary restrictions) Foods to celebrate life events and holidays |
A person’s culture can also affect encounters with health care providers in other ways, such as the following:
- Level of family involvement in care
- Timing for seeking care
- Acceptance of treatment (as preventative measure or for an actual health problem)
- The accepted decision-maker (i.e., the patient or other family members)
- Use of home or folk remedies
- Seeking advice or treatment from nontraditional providers
- Acceptance of a caregiver of the opposite gender
Cultural Diversity and Cultural Humility
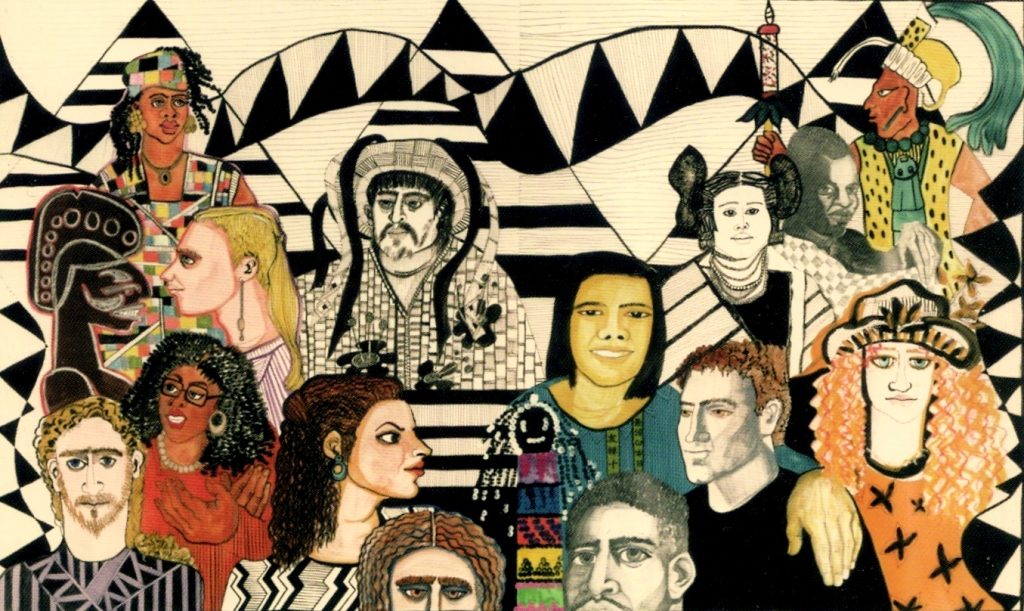
Cultural diversity is a term used to describe cultural differences among people. See Figure 3.2[8] for artwork depicting diversity. While it is useful to be aware of specific traits of a culture or subculture, it is just as important to understand that each individual is unique and there are always variations in beliefs among individuals within a culture. Nurses should, therefore, refrain from making assumptions about the values and beliefs of members of specific cultural groups.[9] Instead, a better approach is recognizing that culture is not a static, uniform characteristic but instead realizing there is diversity within every culture and in every person. The American Nurses Association (ANA) defines cultural humility as, “A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.”[10]
Current demographics in the United States reveal that the population is predominantly white. People who were born in another country, but now live in the United States, comprise approximately 14% of the nation’s total population. However, these demographics are rapidly changing. The United States Census Bureau projects that more than 50 percent of Americans will belong to a minority group by 2060. With an increasingly diverse population to care for, it is imperative for nurses to integrate culturally responsive care into their nursing practice.[11],[12] Creating a culturally responsive environment is discussed in a later subsection of this chapter.
Concepts Related to Culture
There are additional concepts related to culture that can impact a nurse’s ability to provide culturally responsive care, including stereotyping, ethnocentrism, discrimination, prejudice, and bias. See Table 3.2c for definitions and examples of these concepts.
Table 3.2c Concepts Related to Culture
| Concepts | Definitions | Examples |
|---|---|---|
| Stereotyping | The assumption that a person has the attributes, traits, beliefs, and values of a cultural group because they are a member of that group. | The nurse teaches the daughter of an older patient how to make online doctor appointments, assuming that the older patient does not understand how to use a computer. |
| Ethnocentrism | The belief that one’s culture (or race, ethnicity, or country) is better and preferable than another’s. | The nurse disparages the patient’s use of nontraditional medicine and tells the patient that traditional treatments are superior. |
| Discrimination | The unfair and different treatment of another person or group, denying them opportunities and rights to participate fully in society. | A nurse manager refuses to hire a candidate for a nursing position because she is pregnant. |
| Prejudice | A prejudgment or preconceived idea, often unfavorable, about a person or group of people. | The nurse withholds pain medication from a patient with a history of opioid addiction, assuming they are engaging in drug-seeking behavior rather than requesting relief from actual pain. |
| Bias | An attitude, opinion, or inclination (positive or negative) towards a group or members of a group. Bias can be a conscious attitude (explicit) or an unconscious attitude where the person is not aware of their bias (implicit). | A patient does not want the nurse to care for them because the nurse has a tattoo. |
Race is a socially constructed idea because there are no true genetically or biologically distinct races. Humans are not biologically different from each other. Racism presumes that races are distinct from one another and views expression of one’s cultural beliefs as a heritable trait. It also denotes a hierarchy to race, implying that races are unequal. Ernest Grant, president of the American Nurses Association (ANA), recently declared that nurses are obligated “to speak up against racism, discrimination, and injustice. This is non-negotiable.”[13] As frontline health care providers, nurses have an obligation to recognize the impact of racism on their patients and the communities they serve.[14]
Sexual Orientation and Gender Identity
Culture can exert a powerful influence on a person’s sexual orientation and gender expression. Sexual orientation refers to a person’s physical and emotional interest or desire for others. Sexual orientation is on a continuum and is manifested in one’s self-identity and behaviors.[15] The acronym LGBTQAI+ stands for Lesbian, Gay, Bisexual, Transgender, Queer, Asexual, and Intersex. The “+” stands for other identities not encompassed in this short acronym that is often used to refer to the community as a whole. See Figure 3.3[16] for an image of participants in a rally supporting LGBT rights. Historically, individuals within the LGBTQAI+ community have experienced discrimination and prejudice from health care providers and avoided or delayed health care due to these negative experiences. Despite increased recognition of this community in recent years, members of the LGBTQAI+ community continue to experience significant health disparities. Persistent cultural bias and stigmatization of LGBTQAI+ people have been shown to contribute to higher rates of substance abuse and suicide rates in this population.[17],[18],[19]

Gender identity refers to a person’s inner sensibility that they are a man, a woman, or perhaps neither. To the extent that a person’s gender identity does not conform with the sex assigned to them at birth, they may identify as transgender or as nonbinary. Nonbinary means they don’t fall simply into one of two categories, male or female. Transgender and nonbinary people may be sexually oriented toward men, women, both sexes, or neither sex.[20] Gender expression refers to a person’s outward demonstration of gender in relation to societal norms, such as in style of dress, hairstyle, or other mannerisms.[21] Asking a patient for their preferred pronoun (he, she, they, ze, etc.) is considered part of a routine nursing assessment.
Related Ethical Considerations
Justice, a principle and moral obligation to act on the basis of equality and equity, is a standard linked to fairness for all in society.[22] The ANA states this obligation guarantees not only basic rights (respect, human dignity, autonomy, security, and safety) but also fairness in all operations of societal structures. This includes care being delivered with fairness, rightness, correctness, unbiasedness, and inclusiveness while being based on well-founded reason and evidence.[23]
Social justice is related to respect, equity, and inclusion. The ANA defines social justice as equal rights, equal treatment, and equitable opportunities for all.[24] The ANA further states, “Nurses need to model the profession’s commitment to social justice and health through actions and advocacy to address the social determinants of health and promote well-being in all settings within society.”[25]
Social determinants of health are nonmedical factors that influence health outcomes, including conditions in which people are born, grow, work, live, and age, and the wider sets of forces and systems shaping the conditions of daily life.[26] Health outcomes impacted by social determinants of health are referred to as health disparities. Health disparities are further discussed in the “Health Disparities” section later in this chapter.
- “Cultural diversity large.jpg” by მარიამ იაკობაძე is licensed under CC BY-SA 4.0 ↵
- Curtis, E., Jones, R., Tipene-Leach, D., Walker, C., Loring, B., Paine, S.-J., & Reid, P. (2019). Why cultural safety rather than cultural competency is required to achieve health equity: A literature review and recommended definition. International Journal for Equity in Health, 18, 174. https://doi.org/10.1186/s12939-019-1082-3 ↵
- Young, S., & Guo, K. (2016). Cultural diversity training: The necessity for cultural competence for healthcare providers and in nursing practice. The Health Care Manager, 35(2), 94-102. https://doi.org/10.1097/hcm.0000000000000100 ↵
- Campinha-Bacote, J. (2011). Coming to know cultural competence: An evolutionary process. International Journal for Human Caring, 15(3), 42-48. ↵
- Cole, N. L. (2018). How different cultural groups become more alike: Definition, overview and theories of assimilation. ThoughtCo. https://www.thoughtco.com/assimilation-definition-4149483 ↵
- The Truth and Reconciliation Commission of Canada.(2015). Honoring the truth, reconciling for the future: A summary of the final report of the truth and reconciliation commission of Canada. http://www.trc.ca/assets/pdf/Honouring_the_Truth_Reconciling_for_the_Future_July_23_2015.pdf ↵
- Smith, A. (2007, March 26). Soul wound: The legacy of Native American schools. Amnesty International Magazine. https://web.archive.org/web/20121206131053/http://www.amnestyusa.org/node/87342 ↵
- “Pure_Diversity,_Mirta_Toledo_1993.jpg” by Mirta Toledo is licensed under CC BY-SA 4.0 ↵
- Young, S., & Guo, K. (2016). Cultural diversity training: The necessity for cultural competence for healthcare providers and in nursing practice. The Health Care Manager, 35(2), 94-102. https://doi.org/10.1097/hcm.0000000000000100 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Young, S., & Guo, K. (2016). Cultural diversity training: The necessity for cultural competence for healthcare providers and in nursing practice. The Health Care Manager, 35(2), 94-102. https://doi.org/10.1097/hcm.0000000000000100 ↵
- Kaihlanen, A. M., Hietapakka, L., & Heponiemi, T. (2019). Increasing cultural awareness: Qualitative study of nurses’ perceptions about cultural competence training. BMC Nursing, 18(1), 1–9. https://doi.org/10.1186/s12912-019-0363-x ↵
- American Nurses Association. (2020, June 1). ANA president condemns racism, brutality and senseless violence against black communities. https://www.nursingworld.org/news/news-releases/2020/ana-president-condemns-racism-brutality-and-senseless-violence-against-black-communities/ ↵
- Fulbright-Sumpter, D. (2020). “But I’m not racist ...” The nurse’s role in dismantling institutionalized racism. Texas Nursing, 94(3), 14–17. ↵
- Brydum, S. (2015, July 31). The true meaning of the word cisgender. The Advocate. https://www.advocate.com/transgender/2015/07/31/true-meaning-word-cisgender ↵
- “Dublin_LGBTQ_Pride_Festival_2013_-_LGBT_Rights_Matter_(9183564890).jpg” by infomatique is licensed under CC BY-SA 2.0 ↵
- Cole, N. L. (2018). How different cultural groups become more alike: Definition, overview and theories of assimilation. ThoughtCo. https://www.thoughtco.com/assimilation-definition-4149483 ↵
- U.S. Department of Health and Human Services. Healthy People 2020. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health ↵
- Chance, T. F. (2013). Going to pieces over LGBT health disparities: How an amended affordable care act could cure the discrimination that ails the LGBT community. Journal of Health Care Law and Policy, 16(2), 375–402. https://digitalcommons.law.umaryland.edu/cgi/viewcontent.cgi?article=1309&context=jhclp ↵
- Meerwijk, E. L., & Sevelius, J. M. (2017). Transgender population size in the United States: A meta-regression of population-based probability samples. American Journal of Public Health, 107(2), e1–e8. https://doi.org/10.2105/AJPH.2016.303578 ↵
- Keuroghlian, A. S., Ard, K. L., & Makadon, H. J. (2017). Advancing health equity for lesbian, gay, bisexual and transgender (LGBT) people through sexual health education and LGBT-affirming health care environments. Sexual Health, 14(1), 119–122. https://doi.org/10.1071/SH16145 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
A set of beliefs, attitudes, and practices shared by a group of people or community that are accepted, followed, and passed down to other members of the group.
A smaller group of people within a larger culture, often based on a person’s occupation, hobbies, interests, or place of origin.
The many ways in which a person expresses their cultural identity are closely intertwined and not separated.
The process whereby a member of a cultural group adopts or conforms with the practices, habits, and norms of another group, usually a dominant group. As a result, the person gradually takes on a new cultural identity, often losing their original identity in the process.
Cultural differences in people.
A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.
Assuming that a person has the attributes, traits, beliefs, and values of a group because they are a member of that group.
The belief that one’s culture (or race, ethnicity, or country) is better and preferable than another’s.
Unfair and different treatment of another person or group, denying them opportunities and rights to participate fully in society.
To “pre-judge;” a preconceived idea, often unfavorable, about a person or group of people.
To carry an attitude, opinion, or inclination (positive or negative) towards a group or members of a group. Bias can be a conscious attitude (explicit) or a person may not be aware of their bias (implicit).
A socially constructed idea; there are no truly genetically or biologically distinct races. Humans are biologically similar to each other, not different.
The presumption that races are distinct from one another and there is a hierarchy to race, implying that races are unequal. In racism, expression of one’s cultural beliefs are viewed as a heritable trait.
A person’s physical and emotional interest or desire for others. Sexual orientation is on a continuum and is manifested in one’s self-identity and behaviors.
Lesbian, gay, bisexual, transgender, queer, or questioning in reference to sexual orientation.
A person’s inner sensibility that they are a man, a woman, or perhaps neither.
A person’s outward demonstration of gender in relation to societal norms, such as in style of dress, hairstyle, or other mannerisms.
Equal rights, equal treatment, and equitable opportunities for all.
Nonmedical factors that influence health outcomes, including conditions in which people are born, grow, work, live, and age, and the wider sets of forces and systems shaping the conditions of daily life.

