2.4 Communicating With Health Care Team Members
Open Resources for Nursing (Open RN)
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 2.8[1] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports. Reports may be verbal (e.g., reports given in person, by telephone, or recorded) or written (e.g., reports provided electronically or by fax).

Reports to Health Care Team Members
Nurses routinely report information to other nurses and health care team members, as well as urgently contact health care providers to report changes in patient status.
Standardized methods of communication have been developed to allow information to be exchanged between health care team members in a structured, concise, and accurate manner to ensure safe patient care. One common format used by health care team members to exchange patient information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back or a simpler version called SBAR:
-
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the patient’s name and location, why you are calling, recent vital signs, and the status of the patient.
- Background: Provide pertinent background information about the patient such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current patient situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the patient, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the patient’s chart.
Read an example of an ISBARR report in the following box. Information is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. The patient has no known allergies and is a full code. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site, and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear, and her heart rate is regular. I am concerned her incision site may be becoming infected and that she will have difficulty with therapy if her pain remains uncontrolled.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
Handoff Reports
Handoff reports are defined by The Joint Commission as “a transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.”[2] In 2017, The Joint Commission issued a critical alert about inadequate handoff communication that has resulted in patient harm such as wrong-site surgeries, delays in treatment, falls, and medication errors. Strategies for improving handoff communication have been implemented at agencies across the country.
Although many types of nursing shift-to-shift handoff reports have been used over the years, evidence strongly supports that bedside handoff reports increase patient safety, as well as patient and nurse satisfaction, by effectively communicating current, accurate patient information in real time.[3] See Figure 2.9[4] for an image illustrating two nurses participating in a handoff report. Bedside reports typically occur in hospitals and include the patient, along with the off-going and the oncoming nurses in a face-to-face handoff report conducted at the patient’s bedside. HIPAA rules must be kept in mind if visitors are present, or the room is not a private room. Family members may be included with the patient’s permission. See a sample checklist for a bedside handoff report from the Agency for Healthcare Research and Quality in Figure 2.10.[5] Although a bedside handoff report is similar to an ISBARR report, it contains additional information to ensure continuity of care across nursing shifts. For example, the “assessment” portion of the bedside handoff report includes detailed pertinent data the oncoming nurse needs to know, such as current head-to-toe assessment findings to establish a baseline; information about equipment such as IVs, catheters, and drainage tubes; and recent changes in medications, lab results, diagnostic tests, and treatments.
![]"618721604-huge" by Rido is used under license from Shutterstock.com. Image showing two nurses discussing a chart both are holding](https://wtcs.pressbooks.pub/app/uploads/sites/31/2020/08/618721604-huge-1024x680.jpg)
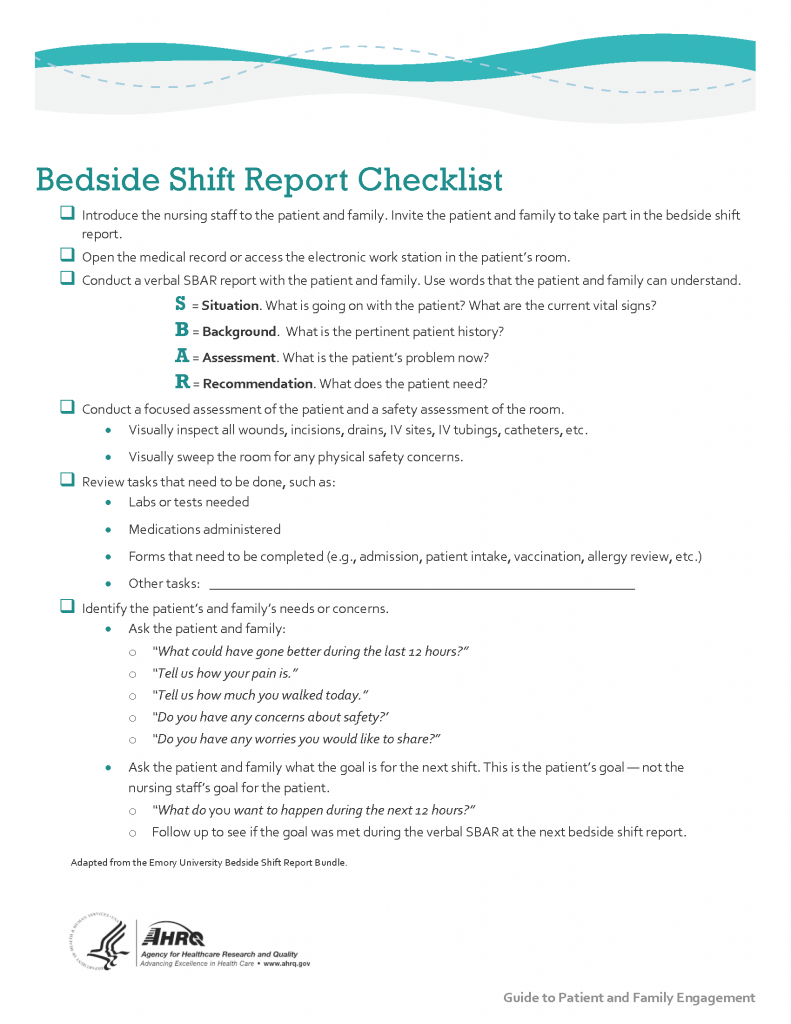
Print a copy of the AHRQ Bedside Shift Report Checklist.
View a video on creating shift reports.[6]
Transfer Reports
Transfer reports are provided by nurses when transferring a patient to another unit or to another agency. Transfer reports contain similar information as bedside handoff reports but are even more detailed when the patient is being transferred to another agency. Checklists are often provided by agencies to ensure accurate, complete information is shared.
Conflict in the Workplace
Nurses encounter conflict in their daily work environment, such as misunderstandings or disagreements among staff, clients, providers, family members, or other individuals. Nurses must learn communication methods that lessen conflict and enhance interactions that lead to a better work environment.
Read additional information about “Conflict Resolution” in Open RN Nursing Health Alterations.
- “1322557028-huge.jpg” by LightField Studios is used under license from Shutterstock.com ↵
- The Joint Commission. (n.d.). Sentinel event alert 58: Inadequate hand-off reports. https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-alert-newsletters/sentinel-event-alert-58-inadequate-hand-off-communication/ ↵
- Dorvil, B. (2018). The secrets to successful nurse bedside shift report implementation and sustainability. Nursing Management, 49(6), 20-25. https://doi.org/10.1097/01.NUMA.0000533770.12758.44 ↵
- “618721604-huge” by Rido is used under license from Shutterstock.com. ↵
- “Strat3_Tool_2_Nurse_Chklst_508.pdf” by AHRQ is licensed under CC0 ↵
- RegisteredNurseRN. (2015, May 23). Nursing shift report sheet templates | How to give a nursing shift report [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/X76iKFQhPNw ↵
A mnemonic for the format of professional communication among health care team members that includes Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
A transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.
A handoff report in hospitals that involves patients, their family members, and both the off-going and the oncoming nurses. The report is performed face to face and conducted at the patient's bedside.

