11.3 Pain Assessment Methods
Open Resources for Nursing (Open RN)
Asking a client to rate the severity of their pain on a scale from 0 to 10, with “0” being no pain and “10” being the worst pain imaginable is a common question used to screen clients for pain. However, according to The Joint Commission requirements described earlier, this question can be used to initially screen a client for pain, but a thorough pain assessment is required. Additionally, the client’s comfort-function goal must be assessed and documented. This individualized comfort-function goal provides the basis for the client’s pain treatment plan and is used to evaluate the effectiveness of interventions and make changes as needed.
PQRSTU, OLDCARTES, and COLDSPA
The “PQRSTU,” “OLDCARTES,” or “COLDSPA” mnemonics are helpful in remembering a standardized set of questions used to gather additional data about a client’s pain. For example, PQRSTU stands for Provocative/Palliative; Quality/Quantity, Region/Radiation, Severity, Timing/Treatment, and Understanding. See Figure 11.4[1] for an illustration of the “PQRSTU” assessment framework.

While interviewing a client about pain, use open-ended questions to allow the client to elaborate on information that further improves your understanding of their concerns. If their answers do not seem to align, validate data with follow-up questions using the PQRSTU framework to clarify information. For example, if a client states that “the pain is tolerable” but also rates the pain as a “7” on a 0-10 pain scale, these answers do not align, so the data must be validated with follow-up questions using the PQRSTU framework. Upon further questioning the client explains they rate the pain as a “7” in their knee when participating in physical therapy exercises, but currently feels the pain is tolerable while resting in bed. This additional information assists the nurse to customize interventions for effective pain management with reduced potential for overmedication with associated side effects. Sample questions when using the PQRSTU assessment are included in Table 11.3a.
Table 11.3a Sample PQRSTU Focused Questions for Pain
| PQRSTU | Questions Related to Pain |
|---|---|
| Provocation/Palliation
|
What makes your pain worse?
What makes your pain feel better? |
| Quality
|
What does the pain feel like?
Note: You can provide suggestions for pain characteristics such as “aching,” “stabbing,” or “burning.” |
| Region
|
Where exactly do you feel the pain? Does it move around or radiate elsewhere?
Note: Instruct the client to point to the pain location. |
| Severity | How would you rate your pain on a scale of 0 to 10, with “0” being no pain and “10” being the worst pain you’ve ever experienced? |
| Timing/Treatment
|
When did the pain start?
What were you doing when the pain started? Is the pain constant or does it come and go? If the pain is intermittent, when does it occur? How long does the pain last? Have you taken anything to help relieve the pain? |
| Understanding | What do you think is causing the pain? |
An alternative mnemonic to use when assessing pain is “OLDCARTES.”
- Onset: When did the pain start? How long does it last?
- Location: Where is the pain?
- Duration: How long has the pain been going on? How long does an episode last?
- Characteristics: What does the pain feel like? Can the pain be described in terms such as stabbing, gnawing, sharp, dull, aching, piercing, or crushing?
- Aggravating factors: What brings on the pain? What makes the pain worse? Are there triggers such as movement, body position, activity, eating, or the environment?
- Radiating: Does the pain travel to another area or the body, or does it stay in one place?
- Treatment: What has been done to make the pain better and has it been helpful? Examples include medication, position change, rest, and application of hot or cold.
- Effect: What is the effect of the pain on participating in your daily life activities?
- Severity: Rate your pain from 0 to 10.
A third mnemonic used is “COLDSPA.”
- C: Character
- O: Onset
- L: Location
- D: Duration
- S: Severity
- P: Pattern
- A: Associated Factors
No matter which mnemonic is used to guide the assessment questions, the goal is to obtain comprehensive assessment data that allows the nurse to create a customized nursing care plan that effectively addresses the client’s need for comfort.
Pain Scales
In addition to using the PQRSTU or OLDCARTES methods of investigating a client’s chief complaint, there are several standardized pain rating scales used in nursing practice.
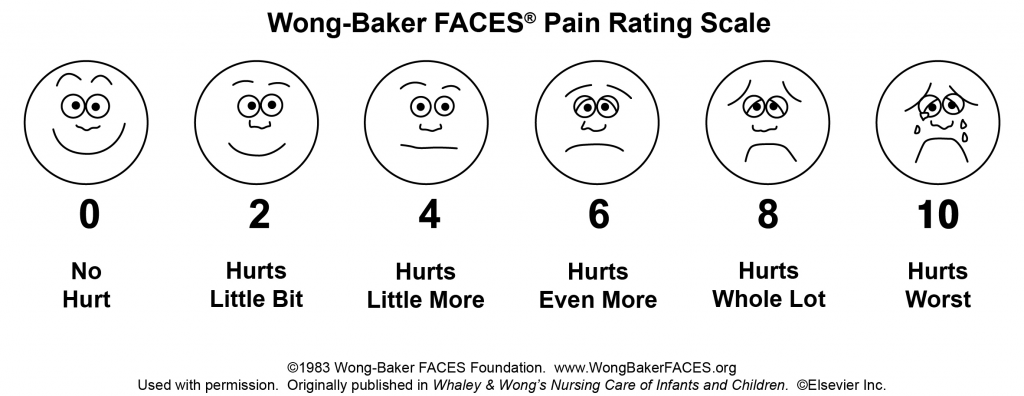
FACES Scale
The FACES scale is a visual tool for assessing pain with children and others who cannot quantify the severity of their pain on a scale of 0 to 10. See Figure 11.5[2] for the FACES Pain Rating Scale. To use this scale, use the following evidence-based instructions. Explain to the client that each face represents a person who has no pain (hurt), some pain, or a lot of pain. “Face 0 doesn’t hurt at all. Face 2 hurts just a little. Face 4 hurts a little more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don’t have to be crying to have this worst pain.” Ask the person to choose the face that best represents the pain they are feeling.[3] Note that the client reports which face best represents how they are feeling and the nurse is not selecting a face based on how the client appears to feel.
FLACC Scale
The FLACC scale (i.e., the Face, Legs, Activity, Cry, Consolability scale) is a measurement used to assess pain for children between the ages of 2 months and 7 years or individuals who are unable to verbally communicate their pain. The scale has five criteria, which are each assigned a score of 0, 1, or 2. The scale is scored in a range of 0–10 with “0” representing no pain.[4] See Table 11.3b for the FLACC scale.
Table 11.3b The FLACC Scale[5]
| Criteria | Score 0 | Score 1 | Score 2 |
|---|---|---|---|
| Face | No particular expression or smile | Occasional grimace or frown, withdrawn, or uninterested | Frequent to constant quivering chin; clenched jaw |
| Legs | Normal position or relaxed | Uneasy, restless, or tense | Kicking or legs drawn up |
| Activity | Lying quietly, normal position, and moves easily | Squirming, shifting, back and forth, or tense | Arched, rigid, or jerking |
| Cry | No cry (awake or asleep) | Moans or whimpers or occasional complaint | Crying steadily, screams or sobs, or frequent complaints |
| Consolability | Content and relaxed | Reassured by occasional touching, hugging, or being talked to; distractible | Difficult to console or comfort |
COMFORT Behavioral Scale
The COMFORT Behavioral Scale is a behavioral-observation tool validated for use in children of all ages who are receiving mechanical ventilation. Eight physiological and behavioral indicators are scored on a scale of 1 to 5 to assess pain and sedation.[6]
View the COMFORT Behavioral Scale.
Pain Assessment in Advanced Dementia (PAINAD) Scale
The Pain Assessment in Advanced Dementia (PAINAD) Scale is a simple, valid, and reliable instrument for assessing pain in noncommunicative clients with advanced dementia. See Table 11.3c for the items included on the scale. Each item is scored from 0-2, When totaled, the score can range from 0 (no pain) to 10 (severe pain).
Table 11.3c The PAINAD Scale[7]
| Item | 0 | 1 | 2 |
| Breathing independent of vocalization | Normal | Occasional labored breathing. Short period of hyperventilation. | Noisy labored breathing. Long period of hyperventilation. Cheyne-Stokes respirations. |
| Negative vocalization | None | Occasional moan or groan. Low-level speech with a negative or disapproving quality. | Repeated troubled calling out. Loud moaning or groaning. Crying. |
| Facial Expression | Smiling or inexpressive | Sad. Frightened. Frown. | Facial grimacing. |
| Body language | Relaxed | Tense. Distressed pacing. Fidgeting. | Rigid. Fists clenched. Knees pulled up. Pulling or pushing away. Striking out. |
| Consolability | No need to console | Distracted or reassured by voice or touch. | Unable to console, distract, or reassure. |
Comfort-Function Goals
Comfort-function goals encourage the client to establish their level of comfort needed to achieve functional goals based on their current health status. For example, one client may be comfortable ambulating after surgery and their pain level is 3 on a 0-to-10 pain intensity rating scale, whereas another client desires a pain level of 0 on a 0-to-10 scale in order to feel comfortable ambulating. To properly establish a client’s comfort-function goal, nurses must first describe the essential activities of recovery and explain the link between pain control and positive outcomes.[9]
If a client’s pain score exceeds their comfort-function goal, nurses must implement an intervention and follow up within 1 hour to ensure that the intervention was successful. Using the previous example, if a client had established a comfort-function goal of 3 to ambulate and the current pain rating was 6, the nurse would provide appropriate interventions, such as medication, application of cold packs, or relaxation measures. The nurse would then perform a follow-up assessment within an hour to evaluate the effectiveness of these interventions. Documentation of the comfort-function goal, pain level, interventions, and follow-up are key to effective, individualized pain management.[10]
- Lapum, J., St-Amant, O., Hughes, M., Petrie, P., Morrell, S., & Mistry, S. (2019). The complete subjective health assessment. Open Libary. https://ecampusontario.pressbooks.pub/healthassessment/ ↵
- Wong-Baker FACES Foundation. (2016). Wong-Baker FACES pain rating scale. https://wongbakerfaces.org/. Used with permission. ↵
- Wong-Baker FACES Foundation. (2016). Wong-Baker FACES pain rating scale. https://wongbakerfaces.org/. Used with permission. ↵
- Merkel, S. I., Voepel-Lewis, T., Shayevitz, J. R., & Malviya, S. (1997). The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatric Nursing, 23(3). https://pubmed.ncbi.nlm.nih.gov/9220806/ ↵
- Merkel, S. I., Voepel-Lewis, T., Shayevitz, J. R., & Malviya, S. (1997). The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatric Nursing, 23(3). https://pubmed.ncbi.nlm.nih.gov/9220806/ ↵
- Freund, D., & Bolick, B. (2019). CE: Assessing a Child's Pain. American Journal of Nursing. 119(5), 34. https://journals.lww.com/ajnonline/Fulltext/2019/05000/CE__Assessing_a_Child_s_Pain.25.aspx ↵
- Warden, V., Hurley, A., & Volicer, L. (2003). Development and psychometric evaluation of the pain assessment in advanced dementia (PAINAD) scale. Journal of the American Medical Directors Association, 4(1), 9-15. https://doi.org/10.1097/01.JAM.0000043422.31640.F7 ↵
- The Hartford Institute for Geriatric Nursing, New York University, Rory Meyers School of Nursing. (n.d.). Assessment tools for best practices of care for older adults. https://hign.org/consultgeri-resources/try-this-series ↵
- Boswell, C., & Hall, M. (2017). Engaging the patient through comfort-function levels. Nursing 2017, 47 (10), 68-69. https://www.nursingcenter.com/journalarticle?Article_ID=4345712&Journal_ID=54016&Issue_ID=4345459 ↵
- Boswell, C., & Hall, M. (2017). Engaging the patient through comfort-function levels. Nursing 2017, 47 (10), 68-69. https://www.nursingcenter.com/journalarticle?Article_ID=4345712&Journal_ID=54016&Issue_ID=4345459 ↵

