4.6 Planning
Open Resources for Nursing (Open RN)
Planning is the fourth step of the nursing process (and the fourth Standard of Practice by the American Nurses Association). This standard is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized for client safety and optimal client outcomes. The plan is modified according to the ongoing assessment of the health care consumer’s response and other indicators. The plan is documented using standardized language or terminology.[1]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve client outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the client’s medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve client problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible.[2] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals. Planning is outside the scope of practice for LPN/VNs, although they may assist in performing planned interventions during the Implementation phase according to their scope of practice. Refer to Figure 4.9a in the “Outcome Identification” section for a illustration of how the Planning phase of the nursing process correlates to NCSBN’s Clinical Judgment Measurement Model.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the client chart. Nurses can also refer to other care planning books or sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are regularly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The RN is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized client’s needs.[3]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with clients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the client. Examples of indirect care interventions are attending care conferences, documenting, and communicating about client care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12[4] for an image of a nurse collaborating with the health care team when planning interventions.)

Independent Nursing Interventions
Any intervention that the nurse can independently provide without obtaining a prescription or consulting another member of the health care team is considered an independent nursing intervention. An example of an independent nursing intervention is when the nurse monitors the client’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist clients to cope with a new medical diagnosis.
Example of an Independent Nursing Intervention
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of an evidence-based independent nursing intervention is, “The nurse will reposition the client with dependent edema frequently, as appropriate.”[5] The nurse would individualize this evidence-based intervention to the client and include agency policy by stating, “The nurse will reposition the client every two hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription or order before they can be performed. Prescriptions are interventions specifically related to medication as directed by an authorized primary health care provider. An order is an intervention, remedy, or treatment as directed by an authorized primary health care provider.[6] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the client’s overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example of a Dependent Nursing Intervention
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative Nursing Interventions
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint.[7]
Example of a Collaborative Nursing Intervention
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a collaborative nursing intervention is the nurse consulting with a respiratory therapist when the client has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “The nurse will manage oxygen therapy in collaboration with the respiratory therapist” in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the client to be successful. For example, adding prune juice to the breakfast meal of a client with constipation will only work if the client likes to drink the prune juice. If the client does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the client, family members, significant others, and the interprofessional team is essential for selecting effective interventions. There is not a set number of interventions required to be included in a nursing care plan, but instead, the number of quality individualized interventions is based on what is required to meet the specific, identified outcomes established for that client.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning at their best and client representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.”[8] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care.[9]
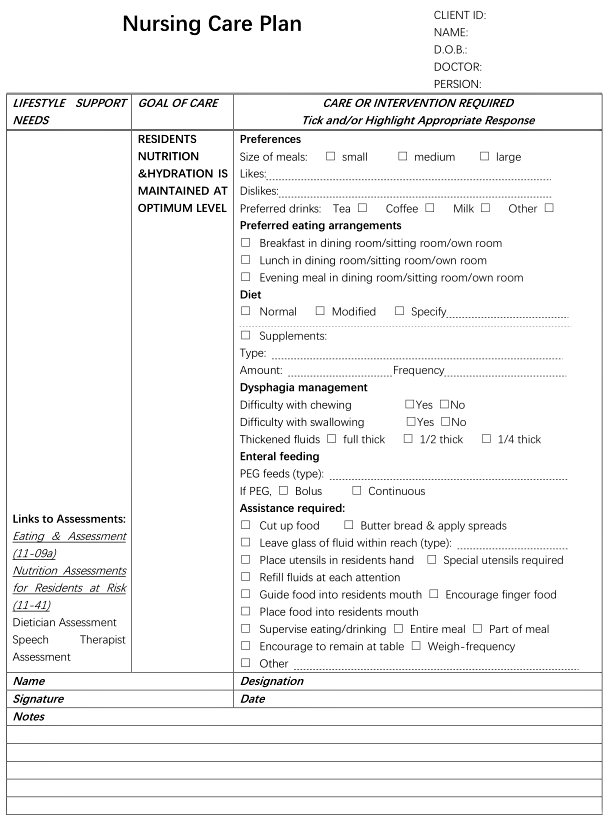
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific client. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each client. See Figure 4.13[10] for an image of a standardized care plan.
Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2021). Nursing diagnoses: Definitions and classification 2021-2023, Twelfth Edition. Thieme Publishers New York. ↵
- Wagner, C. M., Butcher, H. K., & Clarke, M. F. (2024). Nursing interventions classification (NIC) (8th ed.). Elsevier. ↵
- “400845937-huge.jpg” by Flamingo Images is used under license from Shutterstock.com ↵
- Wagner, C. M., Butcher, H. K., & Clarke, M. F. (2024). Nursing interventions classification (NIC) (8th ed.). Elsevier. ↵
- NCSBN. (2024). Test plans. https://www.nclex.com/test-plans.page ↵
- Vera, M. (2020). Nursing care plan (NCP): Ultimate guide and database. https://nurseslabs.com/nursing-care-plans/#:~:text=Collaborative%20interventions%20are%20actions%20that,to%20gain%20their%20professional%20viewpoint ↵
- Centers for Medicare and Medicaid Services. (2017). State operations manual: Appendix PP - Guidance to surveyors for long term care facilities. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_pp_guidelines_ltcf.pdf ↵
- The Joint Commission (n.d.). Standards and guides pertinent to nursing practice. https://www.jointcommission.org/resources/for-nurses/nursing-resources/ ↵
- “Figure 3-3. An example of a nursing care plan in an Australian residential aged care home..png” by NurseRecord is licensed under CC BY-SA 4.0 ↵
Evidence-based actions that the nurse performs to achieve patient outcomes.
Interventions that are carried out by having personal contact with a patient.
Interventions performed by the nurse in a setting other than directly with the patient. An example of indirect care is creating a nursing care plan.
Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else.
Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant.
Interventions specifically related to medication as directed by an authorized primary health care provider
An intervention, remedy, or treatment as directed by an authorized primary health care provider
Member of the healthcare team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client.
Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP).

