14.3 Applying the Nursing Process
Open Resources for Nursing (Open RN)
Now that we have discussed basic nutritional concepts, dietary guidelines, and factors affecting nutritional status, let’s apply the nursing process to this information when caring for clients.
Assessment
A thorough nutritional assessment provides information about an individual’s nutritional status, as well as risk factors for nutritional imbalances. Assessment starts with reviewing the client’s medical record and initiating a client interview, followed by a physical exam and review of lab and diagnostic test results.
Subjective Assessment
Subjective assessments include questions regarding normal eating patterns and risk factor identification. Subjective assessment data is obtained by interviewing the client as a primary source or a family member or caregiver as a secondary source. While a wealth of subjective information can be obtained through a chart review, it is important to verify this information with either the client or family member because details may be recorded inaccurately or may have changed over time. Subjective information to obtain when completing a nutritional assessment includes age, sex, history of illness or chronic disease, surgeries, dietary intake including a 24-hour diet recall or food diary, food preferences, cultural practices related to diet, normal snack and meal timings, food allergies, special diets, and food shopping or preparation activities.
A detailed nutritional assessment can also provide important clues for identification of risk factors for nutritional deficits or excesses. For example, a history of anorexia or bulimia will put the client at risk for vitamin, mineral, and electrolyte disturbances, as well as potential body image disturbances. Swallowing impairments place the client at risk for decreased intake that may be insufficient to meet metabolic demands. Use of recreational drugs or alcohol places the client at risk for insufficient nutrient intake and impaired nutrient absorption. Use of nutritional supplements places the client at risk for excess nutrient absorption and potential toxicity. Recognizing and identifying risks to nutritional status help the nurse anticipate problems that may arise and identify complications as they occur. Ideally, the nurse will recognize subtle cues of impending or actual dysfunction and prevent bigger problems from happening.
Objective Assessment
Objective assessment data is information derived from direct observation by the nurse and is obtained through inspection, auscultation, and palpation. The nurse should consider nutritional status while performing a physical examination.
The nurse begins the physical examination by making general observations about the client’s status. A well-nourished client has normal skin color and hair texture for their ethnicity, healthy nails, a BMI within normal range according to their height, and appears energetic.
Height and weight should be accurately measured and documented. Height and weight in infants and children are plotted on a growth chart to give a percentile ranking across the United States. The infant or child should show a trend of consistent height and weight increase.
Height and weight in adults are often compared to a Body Mass Index (BMI) graph. BMI can also be calculated using the following formulas:
- BMI = weight (kilograms)/height(meters)2
- BMI = weight (pounds) x 703)/height(inches)2
To calculate BMI using a BMI table, the client’s height is plotted on the horizontal axis and their weight is plotted on the perpendicular axis. The BMI is measured where the lines intersect. See Figure 14.11[1] for an image of a BMI table. BMI is interpreted using the following ranges:
- Less than 18.5: Underweight
- 18.5-24.9: Desirable range
- 25-29.9: Overweight
- Equal or greater than 30: Obese[2]
After completing the subjective and objective assessment, the data should be analyzed for expected and unexpected findings. See Table 14.3a for a comparison of expected versus unexpected assessment findings related to nutritional status on assessment, including those that require notification of the health care provider in bold font.
Table 14.3a Expected Versus Unexpected Findings During Nutritional Assessment[3]
| Assessment | Expected Findings | Unexpected Findings
*Bolded items are critical conditions that require immediate health care provider notification. |
|---|---|---|
| General appearance | Energetic; normal skin, hair, and nails; and normal weight related to height | Lethargic, skin ulcerations, rashes, bruising, thinning or loss of hair, spooning of nails, obese, or underweight |
| Eyes | Normal vision and normal eye moisture | Impaired night vision or dry eyes |
| Mouth | Moist mucous membranes, intact oral mucosa, and intact smooth tongue | Dry/sticky mucous membranes, oral ulcerations, glossitis (swollen tongue), coughing while swallowing or inability to swallow, or swollen throat |
| Extremities/Integumentary | Normal skin, nontenting (good skin turgor) and supple texture | Tenting (poor skin turgor), dry skin, edema, or shiny skin |
| Neurological | Normal sensation and normal cognition | Numbness or tingling, tetany, dementia, or acute confusion |
| Cardiac | Normal heart tones, capillary refill < 3 seconds, normal pulses, and normal EKG tracing | Bounding pulses, S3 heart tone, jugular venous distention, abnormal EKG tracing, or cardiac arrhythmias |
| Respiratory | Clear lung sounds throughout, normal respiratory rate, and no shortness of breath | Crackles in lung fields, pink frothy sputum, shortness of breath, or respiratory distress |
| Gastrointestinal | Normal stool quality and frequency for the client, bowel sounds present x 4 quadrants, and absence of nausea/vomiting | Constipation, diarrhea, nausea, or vomiting |
| Urinary | Clear urine, normal urine specific gravity, and urine output >30 mL/hr | Decreased urine output <30 mL/hr or <0.5 mL/kg/hr, concentrated urine, or burning with urination |
| Weight | Normal BMI of 18.5-24.9, weight loss or gain of 0.5 to 1 pound per week is realistic, and <5% weight loss over 6 months | BMI <18.5 or >25, weight gain or loss of > 1kg over 24 hrs, or severe weight loss of >10% over 6 months |
Review how to perform a physical examination on the body systems listed in the previous table in Open RN Nursing Skills, 2e.
Diagnostic and Lab Work
Diagnostic and lab work results can provide important clues about a client’s overall nutritional status and should be used in conjunction with a thorough subjective and objective assessment to provide an accurate picture of the client’s overall health status. Common lab tests include hemoglobin (hgb), hematocrit (HCT), white blood cells (WBC), albumin, prealbumin, and transferrin.
Anemia is a medical condition diagnosed by low hemoglobin levels. Hemoglobin is important for oxygen transport throughout the body. Anemia can be caused acutely by hemorrhage, but it is often the result of chronic iron deficiency, vitamin B12 deficiency, or folate deficiency. Iron supplements, B12 injections, folate supplements, and increased iron or folate intake in the diet can help increase hemoglobin levels.
Albumin and prealbumin are proteins in the bloodstream. They maintain oncotic pressure so that fluid does not leak out of blood vessels into the extravascular space. (Read more about oncotic pressure in the “Fluids and Electrolytes” chapter.) Albumin and prealbumin levels are used as markers of malnutrition, but these levels can also be affected by medical conditions such as liver failure, kidney failure, inflammation, and zinc deficiency. Low albumin levels can indicate prolonged protein deficiency intake over several weeks, whereas prealbumin levels reflect protein intake over the previous few weeks. For this reason, prealbumin is often used to monitor the effectiveness of parenteral nutrition therapy.[4],[5]
Transferrin is a protein required for iron transport on red blood cells. Transferrin levels increase during iron deficiency anemia and decrease with renal or liver failure and infection.
A client’s amount of muscle wasting due to malnutrition is measured by a 24-hour urine creatinine level.[6] If insufficient calories are consumed, the body begins to break down its own tissues in a process called catabolism. Blood urea nitrogen and creatinine are released as a by-product. A 24-hour urine collection measures these by-product levels to assess the degree of catabolism occurring.
White blood cells will decrease with malnourishment, specifically with protein and vitamins C, D, and E and B-complex deficiencies. Low white blood cell counts place the client at risk for infection because adequate white blood cells are necessary for a fully functioning immune system.
See Table 14.3b for a description of selected lab values associated with nutritional status. As always, refer to agency lab reference ranges when providing client care.
Table 14.3b Selected Lab Values Associated with Nutritional Status[7],[8],[9]
| Lab | Normal Range | Nursing Considerations
*Bolded items are critical conditions and require immediate health care provider notification. |
|---|---|---|
| Hemoglobin (Hgb) | Females: 12 – 16 g/dLMales: 14 – 17.4 g/dL |
Hemoglobin measures the oxygen-carrying capacity of blood. Decreased levels occur due to hemorrhage or deficiencies in iron, folate, or B12.
10 – 14: mild anemia 6 – 10: moderate anemia* Less than 6: severe anemia* |
| Hematocrit (Hct) | 37 – 50% | Hematocrit is normally three times the client’s hemoglobin level during normal fluid status. Increased levels occur with dehydration, and decreased levels occur with fluid overload or hemorrhage. |
| White blood cells (WBC) | 5,000 – 10,000 mm3 | Increased levels occur due to infection. Decreased levels occur due to prolonged stress, poor nutrition, and vitamins C, D, and E and B-complex deficiencies.
Less than 4000: at risk for infection or sepsis Greater than 11,000: infection present |
| Magnesium | 1.6 – 2.6 mEq/L | Decreased level with poor nutrition or alcohol abuse. Increased levels due to kidney dysfunction.
Critical values can cause cardiac complications such as arrhythmias or asystole: Less than 1.2 mg/dL or greater than 4.9 mg/dL |
| Albumin | 3.4 – 5.4 g/dL | Increased with dehydration.
Decreased level due to zinc deficiency, corticosteroid use, protein deficiency over several weeks, or conditions resulting in muscle wasting/muscle loss. |
| Prealbumin | 15 – 36 mg/dL | Increased levels with corticosteroid or contraceptive use.
Decreased levels due to inflammation, poor immunity, protein depletion over a few weeks. |
| Transferrin | 250 – 450 mcg/dL | Increased levels due to dehydration and iron deficiency.
Decreased levels due to anemia; vitamin B12, folate, and zinc deficiency; protein depletion; and conditions resulting in muscle wasting/muscle loss. |
| 24-hour urine creatinine | Males: 0.8 – 1.8 g/24 hrs
Females: 0.6 – 1.6 g/24 hrs |
Increased levels with renal disease and muscle breakdown.
Decreased levels with progressive malnutrition as muscles atrophy. |
Various diagnostic tests may be ordered by the health care provider based on the client’s medical conditions and circumstances. For example, a swallow study is a diagnostic test used for clients having difficulty swallowing. An abdominal X-ray is used to determine the correct placement of a feeding tube or to note any excess air or stool in the colon. A barium swallow is used in conjunction with a CT scan to note any blockages in the intestines.
Life Span and Cultural Considerations
Newborns and Infants
A crucial amount of growth and development happens between birth to age two. For proper growth, development, and brain function, this age group requires nutrient-dense food choices, primarily because they eat so little compared to adults, but also because of their rapid growth rate that is higher than any other time of development. Ideally, newborns through age six months should be fed exclusively human breast milk if possible, to develop immunity. Vitamin D and iron supplementation may be needed.[10] For the first two to three days after birth, human milk contains colostrum, a thick yellowish-white fluid rich in proteins and immunoglobulin A (IgA). Colostrum is lower in carbohydrates and fat than mature breast milk. Colostrum helps protect the newborn from infection and builds normal intestinal bacteria. As breast milk matures after two to three days postpartum, it becomes lower in proteins and IgA and higher in carbohydrates and fat.[11] Human donor milk may be used in some situations when the mother cannot breastfeed. If human donor milk is given, it should be sourced through an accredited human milk bank and pasteurized to minimize risk of spreading infectious diseases.
There are many reasons infants may not be breastfed, including insufficient breast milk production, a personal choice not to breastfeed, or adoption of the newborn. If breastfeeding or donor milk is not an option, an iron-fortified commercial infant formula should be used exclusively through at least six months of age. Homemade or non-FDA approved infant formulas or toddler formulas should not be used because they may not meet the high nutritional needs of infants. Infants fed 100% commercial infant formula will not need vitamin D supplementation.[12]
After about six months of age, infants should begin to be introduced to additional nutrient-dense complementary foods that are developmentally appropriate. Foods should be introduced one at a time to monitor for food sensitivities. Introducing food at this time is to provide a varied diet, additional nutrients, and an introduction to different flavors and textures of food. Research shows that introduction to certain allergy-risk foods, such as peanut butter prior to one year of age, helps decrease the risk of developing a peanut allergy later in life. It is important to strictly avoid honey and other unpasteurized food and drink before one year of age to prevent botulism and other bacteria due to immature gut immunity. Additionally, cow’s milk, fortified soy drinks, and fruit or vegetable juices should not be introduced before one year of age.[13]
Children and Adolescents
Growth rate continues to be rapid from ages one through five, requiring adequate nutrition to meet these growth and metabolic demands. Caloric and nutritional intake requirements increase proportionately with age, but unfortunately, the quality of diet tends to decrease proportionately with age. This is in part due to younger children being dependent on adults for nutritional choices and intake while older children and adolescents begin to make their own food choices as they enter school. Poverty can also negatively impact nutritional intake in children and adolescents. School lunch and breakfast programs help mitigate the effects of poverty on nutrition by providing free to low-cost, nutritionally balanced meals.[14]
Healthy dietary habits formed in childhood through adolescence help prevent obesity, cardiovascular disease, diabetes mellitus, and other chronic diseases later in life. It is important to provide children with a variety of different foods prepared in different ways to increase the likelihood of children accepting and growing accustomed to different foods. It is common for children to become picky in their food choices or decide to only eat one or a few different food items over a period of time. Allowing children to help select and prepare food can increase their acceptance of different food choices.[15]
Adults
The adult life stage is ages 19 through 59. A major limiting factor to healthy nutrition in adults is development of poor nutritional habits early in life. These unhealthy diet habits can be very difficult to change due to food preferences, as well as lack of knowledge about proper nutrition. Metabolic rate and caloric needs decrease with increasing age. Females tend to require less caloric intake than males, though caloric and nutritional needs increase with pregnancy and breastfeeding. Without appropriate dietary intake or activity, weight gain will occur that can lead to obesity and other chronic diseases. Over 50% of Americans have one or more chronic diseases that are associated with poor diet and physical inactivity.
Education regarding a healthy diet, including appropriate calorie, saturated fat, sugar, and sodium intakes, helps improve health in adults. Roughly 73% of males and 70% of females in America exceed the recommended daily intake of saturated fat, and up to 97% of males and 82% of females exceed the recommended daily intake of sodium. Approximately 97% of males and 90% of women in America do not consume the recommended intake of dietary fiber, including underconsumption of fruits, vegetables, and whole grains, which contributes to diet-related chronic diseases.
Alcohol consumption can be problematic for maintaining a healthy diet. Chronic alcohol abuse can interfere with vitamin and mineral absorption and result in general malnourishment. Alcohol should be limited to one drink per day or less for women and two drinks or less per day for men. Alcohol should be avoided by those who are pregnant, breastfeeding, younger than 21 years old, have a chemical dependency, or have other underlying health conditions such as diabetes mellitus.[16]
Pregnancy and Lactation
A well-balanced, healthy diet is essential during pregnancy and lactation to prevent maternal, fetal, and newborn problems. Nutritional requirements, such as calories, vitamins, and minerals, increase during pregnancy and lactation. Increased caloric needs should be met with nutrient-dense foods rather than calorie-dense foods that are higher in fats and sugars. Prenatal vitamins and mineral supplements are often prescribed during pregnancy and lactation, in addition to a nutrient-rich diet, to help ensure women meet requirements for folic acid, iron, iodine, choline, and vitamin D. Folic acid is necessary to prevent neural tube defects in the fetus during the first trimester of pregnancy. Iron requirements increase during pregnancy to support fetal development and prevent anemia. Iodine requirements increase during pregnancy and lactation for fetal neurocognitive development. Choline requirements also increase due to the need to replace maternal stores, as well as for fetal brain and spinal cord development.[17]
Older Adults
People aged 65 years and older are considered older adults. Older adults are more likely to suffer from chronic illness and disease. Older adults have lower calorie needs than younger people, though they still need a diet full of nutrient-dense foods because their nutrient needs increase. Caloric needs decrease due to decreased activity, decreased metabolic rates, and decreased muscle mass. Chronic disease and medication can contribute to decreased nutrient absorption. Protein and vitamin B12 are commonly under consumed in older adults. Protein is necessary to prevent loss of muscle mass. Vitamin B12 deficiency can be a problem for older adults because absorption of vitamin B12 decreases with age and with certain medications. Adequate hydration is also a concern for older adults because feelings of thirst decrease with age, leading to poor fluid intake. Additionally, older adults may be concerned with bladder dysfunction so they may consciously choose to limit fluid intake. Loneliness, ability to chew and swallow, and poverty can also decrease dietary intake in older adults.[18] Meals on Wheels, local senior centers, and other community programs can provide socialization and well-balanced meals to older adults.
The Mini-Nutritional Assessment Short-Form is a screening tool used to identify older adults who are malnourished or at risk of malnutrition. Use the following box to download this tool.
Download the Mini-Nutritional Assessment Short-Form from The Hartford Institute for Geriatric Nursing.[19]
Diagnosis
After the assessment stage is conducted, data is analyzed, and pertinent information is clustered together, nursing diagnoses are selected based on defining characteristics. When creating a care plan for a client, review a current nursing care planning source for current NANDA-I approved nursing diagnoses and interventions related to nutritional imbalances. Examples of NANDA-I nursing diagnoses related to nutrition include Imbalanced Nutrition: Less than Body Requirements, Overweight, Obesity, Risk for Overweight, Readiness for Enhanced Nutrition, and Impaired Swallowing.[20] See Table 14.3c for additional information related to the diagnosis Imbalanced Nutrition: Less than Body Requirements.
Table 14.3c Sample NANDA-I Nursing Diagnosis Related to Nutrition[21]
| NANDA-I Diagnosis | Definition | Selected Defining Characteristics |
|---|---|---|
| Imbalanced Nutrition: Less than Body Requirements | Intake of nutrients insufficient to meet metabolic needs. | Abdominal cramping
Abdominal pain Body weight below ideal weight range for age and gender Diarrhea Food intake less than recommended daily allowance (RDA) Hyperactive bowel sounds Lethargy Pale mucous membranes Weight loss with adequate food intake |
A sample nursing diagnosis written in PES format is, “Imbalanced Nutrition: Less than Body Requirements related to insufficient dietary intake as evidenced by body weight 20% below ideal weight range and food intake less than recommended daily allowance.”
Outcome Identification
Goals for clients experiencing altered nutritional status depend on the selected nursing diagnosis and specific client situation. Typically, goals relate to resolution of the nutritional imbalance and are broad in nature. An overall goal related to nutritional imbalances is, “The client will weigh within normal range for their height and age.”[22]
Outcome criteria are specific, measurable, achievable, realistic, and time-oriented. A sample SMART goal is, “The client will select three dietary modifications to meet their long-term health goals using USDA MyPlate guidelines by discharge.”[23]
Planning Interventions
After SMART outcome criteria are customized to the client’s situation, nursing interventions are selected to help them achieve their identified outcomes. Interventions are specific to the alteration in nutritional status and should accommodate the client’s cultural and religious beliefs. The box below outlines selected interventions related to nutrition therapy.
Nutrition Therapy[24]
- Identify nutritional risks
- Monitor food/fluid ingested and calculate daily caloric intake, as appropriate
- Monitor appropriateness of prescribed diet to meet daily nutritional needs, as appropriate
- Initiate prescribed number of calories and types of nutrients needed to meet requirements, as appropriate
- Determine food preferences with consideration of the client’s cultural and religious preferences
- Offer nutritional supplements, as appropriate
- Offer mealtime assistance to support dietary intake, as appropriate
- Determine need for enteral tube or parenteral feedings
- Manage enteral feeding or parenteral nutrition, as indicated
- Structure the environment to create a pleasant and relaxing meal atmosphere
- Present food in an attractive, pleasing manner, giving consideration to color, texture, and variety
- Encourage the client to share mealtimes with others, as appropriate
- Encourage adequate dental and mouth care
- Assist the client to a sitting position before eating or feeding
- Monitor laboratory values, as appropriate
- Instruct the client and family about nutritional information and prescribed diets
- Refer for diet teaching and planning, as appropriate
- Provide written examples of prescribed diet
- Check medications and alter where possible to minimize adverse effects
- Encourage physical activity to maintain or improve muscle mass and function
Clients may be prescribed special diets due to medical conditions or altered nutrition states. See Table 14.3d for commonly prescribed special diets.
Table 14.3d Commonly Prescribed Special Diets
| Diet | Description | Example | Indication |
|---|---|---|---|
| NPO | Nothing by mouth–no food or drink allowed
*Note: Oral care is very important during NPO status. |
Oral care only | Before and after surgery or procedures, when peristalsis is absent, or during severe nausea or vomiting episodes, or for changes in mental status |
| Clear liquids | Fluids or solids that are liquid at room temperature, without residue, clear, or see-through | Water, apple juice, clear soda, Jello, popsicles, and broth | After surgery when peristalsis is slow and diet is being advanced from NPO status |
| Full liquids | Fluids with residue | Creamed soups, pudding, milk, orange juice, and creamed cereals | Next step after clear liquids as diet is being advanced |
| Mechanical soft | Chopped, ground, pureed foods that break apart easily without a knife | Soft cheeses, cottage cheese, ground meat, broiled or baked fish, cooked vegetables, and fruit | Poor or absent dentition; dysphagia |
| Pureed | Spoon thick with consistency of baby food | Applesauce, pudding, mashed potatoes, pureed meats, vegetables, and fruit | Dysphagia |
| Restrictive | Depends on the disease process | Diabetic: controlled amount of carbohydrates
Cardiac: low fat and no added salt Renal: low-sodium and low-potassium containing foods |
Diabetes mellitus
Heart disease
Renal failure or dialysis |
“Thickened liquids” are typically prescribed for clients with difficulty swallowing (dysphagia). Three consistencies of thickened liquids are as follows:
- Nectar-thick liquids: Easily pourable liquid comparable to apricot nectar or thick cream soups.
- Honey-thick liquids: Slightly thicker liquid that is less pourable and drizzles from a cup or bowl.
- Pudding-thick liquids: Liquids that hold their own shape. They are not pourable and usually require a spoon to eat.
Nurses often thicken liquids in the client’s room using a commercial thickener. Most commercial thickeners include directions for achieving the consistency prescribed.
Enteral Nutrition
Enteral nutrition is administered directly to a client’s gastrointestinal tract while bypassing chewing and swallowing. Enteral feedings are prescribed for clients when chewing and/or swallowing are impaired or when there is poor nutritional intake and/or malnutrition.
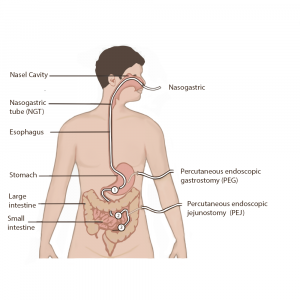
Examples of enteral tube access are nasogastric tubes (NG), orogastric tubes (OG), percutaneous endoscopic gastrostomy (PEG) tubes, or percutaneous endoscopic jejunostomy (PEJ) tubes. See Figure 14.12[25] for an illustration of common enteral tube placement. Nasogastric tubes enter the nare and travel through the esophagus and into the stomach. Liquid tube feedings are infused through this tube and directly into the stomach. Orogastric tubes work in the same manner except they are inserted through the mouth into the esophagus and then into the stomach. Orogastric tubes are typically used with mechanically intubated and sedated clients and should never be used in conscious clients because they can induce a gag reflex and cause vomiting. PEG tubes are inserted through the abdominal wall directly into the stomach, bypassing the esophagus. PEG tubes are used when there is an obstruction to the esophagus, the esophagus has been removed, or if long-term enteral feedings are expected. PEJ tubes are inserted through the abdominal wall directly into the jejunum, bypassing the esophagus and stomach. PEJ tubes are used when all or part of the stomach has been removed or if the provider determines PEJ placement would best suit the client’s needs.
There are several safety considerations for nurses to implement when enteral nutrition is being administered to prevent aspiration and dehydration. Tube placement must be verified after insertion, as well as before every medication or feeding is administered, to prevent inadvertent administration into the lungs if the tube has migrated out of position. Follow agency policy regarding checking placement. The American Association of Critical‐Care Nursing recommends that the position of a feeding tube should be checked and documented every four hours and prior to the administration of enteral feedings and medications by measuring the visible tube length and comparing it to the length documented during X-ray verification. Older methods of checking tube placement included observing aspirated GI contents or the administration of air with a syringe while auscultating (commonly referred to as the “whoosh test”). However, research has determined these methods are unreliable and should no longer be used to verify placement.[26],[27]
In addition to verifying tube placement before administering feedings or medications, nurses perform additional interventions to prevent aspiration. The American Association of Critical‐Care Nurses recommends the following guidelines to reduce the risk for aspiration:
- Maintain the head of the bed at 30°- 45° unless contraindicated
- Use sedatives as sparingly as possible
- Assess feeding tube placement at four‐hour intervals
- Observe for change in the amount of external length of the tube
- Assess for gastrointestinal intolerance at four‐hour intervals[28],[29]
Measurement of gastric residual volume (GRV) is often performed when a client is receiving enteral feeding by using a 60-mL syringe to aspirate stomach contents through the tube. GRVs in the range of 200–500 mL have traditionally triggered nursing interventions, such as slowing or stopping the feeding, to reduce the client’s risk of aspiration. However, according to recent research, it is not appropriate to stop enteral nutrition for GRVs less than 500 mL in the absence of other signs of intolerance because of the impact on the client’s overall nutritional status. Additionally, the aspiration of gastric residual volumes can contribute to tube clogging. Follow agency policy regarding measuring gastric residual volume and implementing interventions to prevent aspiration.[30],[31]
Clients receiving enteral nutrition should be monitored daily for signs of tube feeding intolerance, such as abdominal bloating, nausea, vomiting, diarrhea, cramping, and constipation. If cramping occurs during bolus feedings, it can be helpful to administer the enteral nutritional formula at room temperature to prevent symptoms. Notify the provider of signs of intolerance with anticipated prescription changes regarding the type of formula or the rate of administration.
Electrolytes and blood glucose levels should also be monitored for signs of imbalances. Carbohydrates in tube feedings are absorbed quickly, so blood glucose levels are monitored, and elevated levels are typically treated with sliding scale insulin according to health care provider orders.
Read about “Enteral Tube Management” in Open RN Nursing Skills, 2e.
Parenteral Nutrition
Parenteral nutrition is nutrition delivered through a central intravenous line, generally the subclavian or internal jugular vein, to clients who require nutritional supplementation but are not candidates for enteral nutrition. Parenteral nutrition is an intravenous solution containing glucose, amino acids, minerals, electrolytes, and vitamins. A lipid solution is typically given in a separate infusion in a hospital setting. This combination of solutions is called total parenteral nutrition because it supplies complete nutritional support. Parenteral nutrition is administered via an IV pump.
Because parenteral nutrition consists of concentrated glucose, amino acids, and minerals, it is very irritating to the blood vessels. For this reason, a large central vein must be used for administration. The client’s lab work must also be closely monitored for signs of nutrient excesses. See Figure 14.13[32] for an image of home parenteral nutrition formula. In this image are three compartments: one with glucose, one with amino acids, and one with lipids. The three compartments are kept separate to enable storage at room temperature but are mixed together before use.
Parenteral nutrition is typically used when the client’s intestines or stomach is not working properly and must be bypassed, such as during paralytic ileus where peristalsis has completely stopped, or after postoperative bowel surgeries, such as bowel resection. It may also be prescribed for severe malnutrition, severe burns, metastatic cancer, liver failure, or hyperemesis with pregnancy.

Implementing Interventions
When implementing interventions to promote good nutrition, it is vital to consider the client’s cultural and religious beliefs. Encourage clients to make healthy food selections based on their food preferences.
If a client has nutritional deficit, perform nursing interventions prior to mealtime to promote their appetite. For example, if the client has symptoms of pain or nausea, administer medications prior to mealtime to manage these symptoms. Do not perform procedures that may affect the client’s appetite, such as wound dressing changes, immediately prior to mealtime. Manage the environment prior to the food arriving and remove any unpleasant odors or sights. For example, empty the trash can of used dressings or incontinence products. If the client is out of the room when the meal tray arrives and the food becomes cold, reheat the food or order a new meal tray.
When assisting clients to eat, help them to wash their hands and use the restroom if needed. Assist them to sit in a chair or sit in high Fowler’s position in bed. Set the meal tray on an overbed table and open containers as needed. Encourage the client to feed themselves as much as possible to promote independence. If a client has vision impairments, explain the location of the food using the clock method. For example, “Your vegetables are at 9 o’clock, your potatoes are at 12 o’clock, and your meat is at 3 o’clock.” When feeding a client, ask them what food they would like to eat first. Allow them to eat at their own pace with time between bites for thorough chewing and swallowing. If any signs of difficulty swallowing occur, such as coughing or gagging, stop the meal and notify the provider of suspected swallowing difficulties.
Evaluation
It is always important to evaluate the effectiveness of interventions implemented. Evaluation helps the nurse and care team determine if the interventions are appropriate for the client or if they need to be revised. Table 14.3e provides a list of assessment findings indicating that alterations of nutritional status are improving with the planned interventions.
Table 14.3e Evaluation of Alterations in Nutritional Status
| Imbalance | How Do We Know It Is Improved? |
|---|---|
| Imbalanced Nutrition: Less than Body Requirements | Stable or increasing weight; sufficient daily calories; well-balanced meal intake; improved energy, appearance of hair, nails, skin, or vision |
| Imbalanced Nutrition: More than Body Requirements | Stable or decreasing weight, <5% body weight loss over six months, well-balanced meal intake |
- “Bmi-chart_colored.gif” by Cbizzy2313 is licensed under CC BY-SA 4.0 ↵
- Hood, W. A. (2020). Nutritional status assessment in adults technique. Medscape. https://emedicine.medscape.com/article/2141861-technique ↵
- Hood, W. A. (2020). Nutritional status assessment in adults technique. Medscape. https://emedicine.medscape.com/article/2141861-technique ↵
- U.S. National Library of Medicine. (2022). Prealbumin blood test: Medlineplus medical test. MedlinePlus. https://medlineplus.gov/lab-tests/prealbumin-blood-test/ ↵
- Simons, S. R., & Abdallah, L. M. (2012). Bedside assessment of enteral tube placement: Aligning practice with evidence. American Journal of Nursing, 112(2), 40-46. https://doi.org/10.1097/01.naj.0000411178.07179.68 ↵
- Hood, W. A. (2020). Nutritional status assessment in adults laboratory medicine. Medscape. https://emedicine.medscape.com/article/2141861-labs ↵
- Hood, W. A. (2020). Nutritional status assessment in adults laboratory medicine. Medscape. https://emedicine.medscape.com/article/2141861-labs ↵
- Ignativicius, D. D., Workman, M. L., & Rebar, C. (2018). Medical surgical nursing: Concepts for interprofessional collaborative care (9th ed.). Elsevier. ↵
- University of Rochester Medical Center. (n.d.). Health Encyclopedia. https://www.urmc.rochester.edu/encyclopedia.aspx ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- Jozsa, F., & Thistle, J. (2023). Anatomy, colostrum. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK513256/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025 (9th ed.). https://www.dietaryguidelines.gov/ ↵
- The Hartford Institute for Geriatric Nursing, New York University, Rory Meyers School of Nursing. (n.d.). Assessment tools for best practices of care for older adults. https://hign.org/consultgeri-resources/try-this-series ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2021). Nursing diagnoses: Definitions and classification 2021-2023, Twelfth Edition. Thieme Publishers New York. ↵
- Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2021). Nursing diagnoses: Definitions and classification 2021-2023, Twelfth Edition. Thieme Publishers New York. ↵
- Ackley, B., Ladwig, G., Makic, M.B., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier, pp. 651-657. ↵
- Ackley, B., Ladwig, G., Makic, M.B., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier, pp. 651-657. ↵
- Wagner, C. M., Butcher, H. K., & Clarke, M. F. (2024). Nursing interventions classification (NIC) (8th ed.). Elsevier. ↵
- “Types and Placement of Enteral Tubes” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Simons, S. R., & Abdallah, L. M. (2012). Bedside assessment of enteral tube placement: Aligning practice with evidence. American Journal of Nursing, 112(2), 40-46. https://doi.org/10.1097/01.naj.0000411178.07179.68 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- Simons, S. R., & Abdallah, L. M. (2012). Bedside assessment of enteral tube placement: Aligning practice with evidence. American Journal of Nursing, 112(2), 40-46. https://doi.org/10.1097/01.naj.0000411178.07179.68 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- Simons, S. R., & Abdallah, L. M. (2012). Bedside assessment of enteral tube placement: Aligning practice with evidence. American Journal of Nursing, 112(2), 40-46. https://doi.org/10.1097/01.naj.0000411178.07179.68 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- “Tpn_3bag.jpg” by Tristanb in English Wikipedia is licensed under CC BY-SA 3.0 ↵
A measure of weight categories including underweight, normal weight, overweight, and obese taking height and weight into consideration.
A thick yellowish-white fluid rich in proteins and immunoglobulin A (IgA) and lower in carbohydrates and fat than mature breast milk secreted within the first 2-3 days after giving birth.
Breast milk production.
Liquid nutrition given through the gastrointestinal tract via a tube while bypassing chewing and swallowing.
An intravenous solution containing glucose, amino acids, minerals, electrolytes, and vitamins, along with supplemental lipids.

