9.7 Assisting With Sensory Deficits
An impairment of one or more senses can occur in clients of any age, in addition to the aging process causing a decline in all sensory functioning. Sensory impairments, especially vision and hearing impairments, can impact the way a person navigates through the environment and thus increases their risk for falls. Refer to Chapter 11.8, “Neurological System” for additional information about sensory impairments. Information regarding communicating with individuals affected by sensory deficits can be found in the Chapter 1.3, “Strategies for Communicating With Patients With Impaired Hearing, Vision, and Speech” subsection. Interventions that can be performed by nursing assistants to reduce safety risks are described below.
Visual Impairment
The human eye changes around age 40 and decreases an individual’s ability to see close-up objects clearly and makes reading more difficult, although distance vision remains intact. Depth perception also becomes distorted, meaning the person cannot accurately determine the distance between themselves and another object.
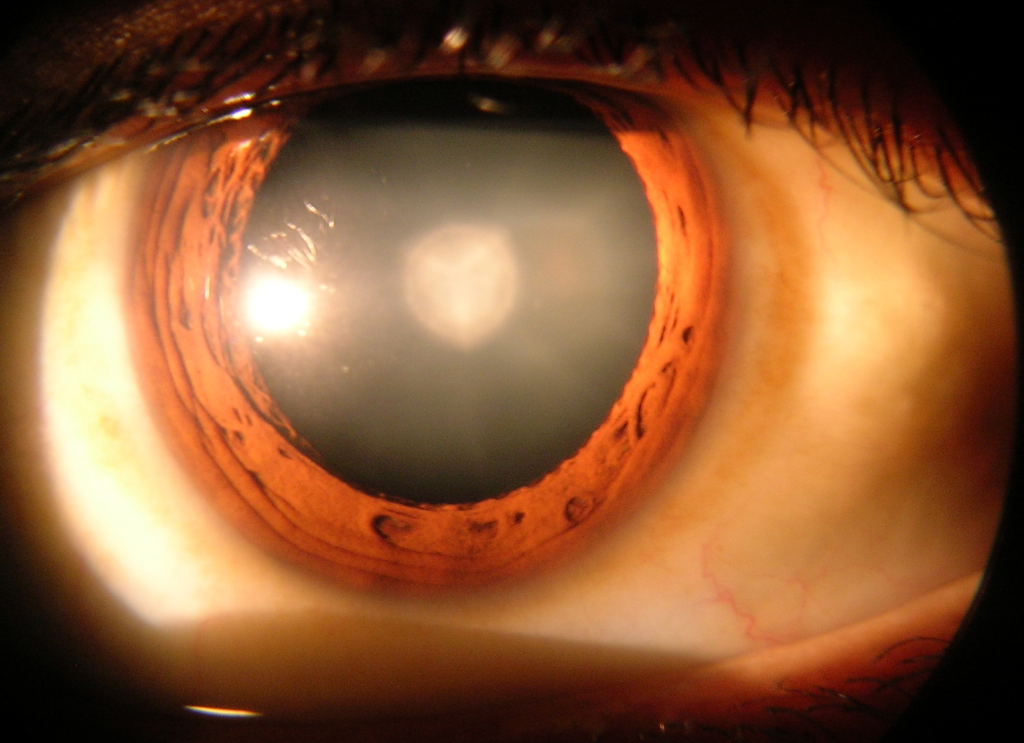
Other eye conditions may occur with age that impair vision. Some people develop cataracts, a clouding of the clear lens of the eye. Cataracts can be observed in a person’s eye by the appearance of a cloudiness in their pupil. See Figure 9.13[1] for a simulated image of a person with cataracts.
Glaucoma is a visual condition caused by elevated pressure on the optic nerve, resulting in loss of peripheral vision, blind spots, or even blindness across the entire visual field.
Macular degeneration is another visual condition that results in a blind spot in an individual’s center field of vision. It is the leading cause of vision loss in people over 50. See Figure 9.14[2] for a simulated image of what a person with macular degeneration may experience.

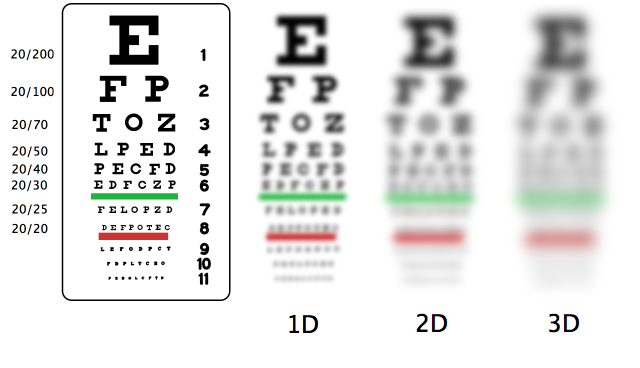
The Snellen chart is a common tool for assessing distant vision.[3] See Figure 9.15[4] for a simulated image of how a person with 20/20 vision sees the Snellen chart compared to simulated visual experiences of those with levels of low vision and blindness.
To learn more about cataracts, visit the MedlinePlus webpage on cataracts.
To experience what someone with cataracts may see, watch the following YouTube video[5]: See What I See: Cataracts.
To learn more about glaucoma, visit the National Eye Institute web page on glaucoma.
To experience what someone with glaucoma may see, watch the following YouTube video[6]: Glaucoma Simulation – Busy Road.
To learn more about macular degeneration, visit the American Academy of Ophthalmology’s What is Macular Degeneration? web page.
To experience what someone with macular degeneration may see, watch the following YouTube video[7]: See What I See: AMD.
The simplest interventions for maintaining safety for clients with visual impairment include ensuring they are wearing their prescribed eyeglasses, the glasses are clean, and their living areas are well-lit. There should be no clutter, area rugs, or other small objects on the floor or in a direct path to the bathroom, closet, or exit door of the room to prevent tripping. Keeping the room and personal belongings arranged in a consistent manner allows residents to remain aware of the room set-up, making it easier for them to navigate despite impaired vision. If their visual impairment is severe, tell them where personal items are located before leaving the room, especially the call light and frequently used things like facial tissue, beverages, television remotes, or phones. When ambulating a resident with poor vision, tell them when they are getting close to an object that could pose a fall risk.
Hearing Loss
The most common form of hearing loss occurs as a natural part of aging and is called presbycusis. This type of hearing loss is typically worse at higher frequency sounds, so it interferes with speech recognition and music appreciation. Men tend to experience greater hearing loss than females, perhaps because they have historically worked in louder environments, but it is unknown how much the differences in hearing between genders are caused by biological or social factors.[8]
Hearing can impact an individual’s safety risks. For example, the sense of hearing allows a person to locate objects around them making noise without much conscious thought. For example, sounds like fire alarms or ambulance sirens warn people of emergencies. To understand how sound affects safety, try wearing noise-canceling headphones or earplugs while seated in a populated, busy area. Notice how the lack of hearing changes your perception of movement and the location of objects in your environment.
To assist individuals with hearing loss, use other senses, such as vision and touch, to aid in communication. Stand directly in front of the person when you are speaking, use appropriate gestures to guide actions, and use a light touch to gain their attention or assist in movement. People with hearing loss may become frustrated if they are unable to communicate effectively and may withdraw from interaction with others if hearing loss is profound. Be sure to utilize communication techniques described in the Chapter 1.3 subsection “Impaired Hearing” to prevent isolation.
Hearing aids make sounds louder but do not help in every environment. Even with hearing aids, it can be difficult for individuals to hear a conversation in a large open space or if there is other background noise such as music, television, or other conversations.
If a resident has hearing aids, be sure they are cleaned regularly, and change the batteries once a week. Wax can be removed with a monofilament tool provided with the hearing aids. Some hearing aids have rechargeable batteries that should be charged each night while the resident sleeps. See Figure 9.16[9] for a hearing aid in a case with a battery and a cleaning tool.

Hearing aids are expensive for residents to purchase, so it is important to always handle them with care and store them in an appropriate place, so they are not lost. If you are unsure of how to fit a hearing aid into a resident’s ear, ask for assistance from the nurse. Hearing aids can fit completely inside the ear or over the top of the ear. See Figure 9.17[10] for an example of a hearing aid that is placed over the top of the ear and Figure 9.18[11] for a simulated hearing aid placed inside a mannequin ear.


To experience what someone with hearing loss may hear, watch the following YouTube video[12]: Hearing Loss Simulator – Hear What Hearing Loss Sounds Like.
Speech Impairment
Speech impairment is common for individuals who have had a stroke or who have experienced injuries to certain parts of their brain. These injuries can make forming words and understanding conversations difficult. The medical terms for these conditions are expressive aphasia and receptive aphasia.
People with aphasia can become very frustrated. Everyone has experienced a time when they were trying to think of a word but couldn’t remember it. Imagine how it would feel if this was your experience every time you were trying to communicate with someone. Just as can happen with people with hearing loss, clients with aphasia may isolate themselves, avoid interaction, or become agitated and even aggressive if not approached appropriately.
Interventions when working with a client with a speech impairment include allowing the person extra time to form words or to process what was spoken to them. The feeling of being rushed can make aphasia worse, so providing ample time to process and respond is key. Writing conversations on a whiteboard may also be helpful, depending upon the cognition of the person.
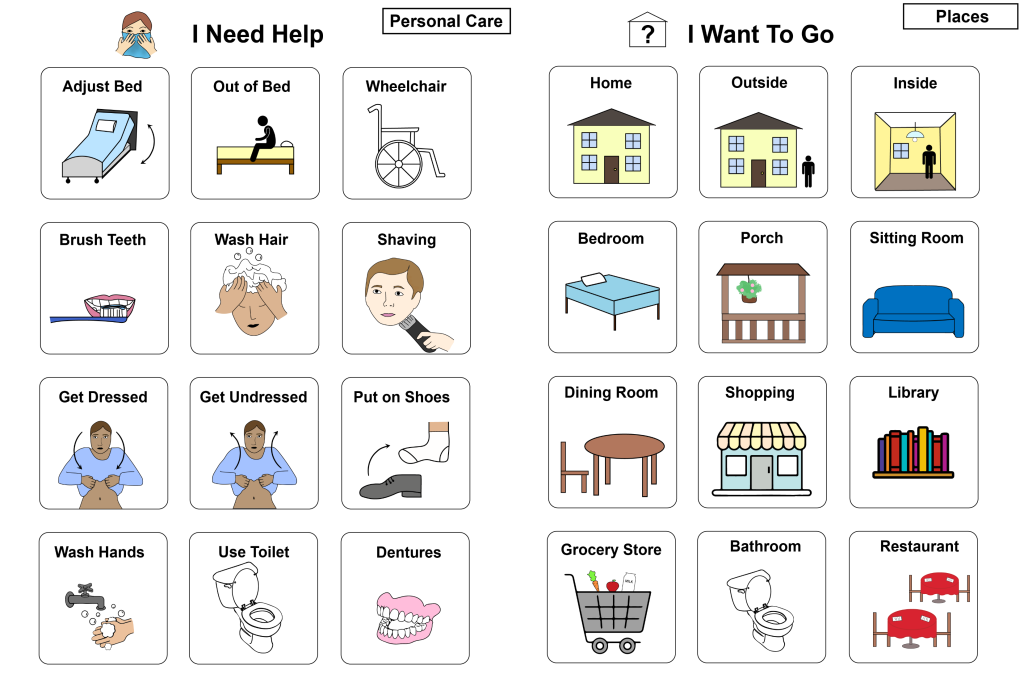
A speech therapist plays an integral role in assessing a resident with aphasia and creating a communication plan. A communication book may be created so the person can point to images of common phrases or requests instead of trying to remember or say the words. See Figure 9.19[13] for an example of a communication board. Refer to the Chapter 1.2, “Overcoming Communication Barriers” subsection for additional information on overcoming barriers.
To learn more about speech impairment, view the following YouTube video[14]: Aphasia: The Disorder That Makes You Lose Your Words – Susan Wortman-Jutt.
- “Cataract in human eye.png” by Rakesh Ajuja, MD is licensed under CC BY-SA 3 ↵
- National Eye Institute. (2020, August 17). Age-related macular degeneration. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration ↵
- This work is a derivative of Nursing Skills by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- “Snellen-myopia.png” by Daniel P. B. Smith (talk) (Uploads) is licensed under CC BY-SA 3.0 ↵
- National Eye Institute, NIH. (2018, November 7). See what I see: Cataracts [Video]. YouTube. All rights reserved. https://youtu.be/nGV3PD5sBgM ↵
- Pugini, A. (2016, May 21). Glaucoma simulation - Busy road [Video]. YouTube. All rights reserved. https://youtu.be/jkYeC_JDEPs ↵
- National Eye Institute, NIH. (2018, November 7). See what I see: AMD [Video]. YouTube. All rights reserved. https://youtu.be/Iu5ToTfUOok ↵
- Introduction to Sensation and Perception by Students of PSY 3031 and edited by Dr. Cheryl Olman is licensed under CC BY 4.0 ↵
- “Hearing Aid in Case.jpg” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “mark-paton-QpOxts03rps-unsplash” by Mark Paton on Unsplash is licensed under CC BY 4.0 ↵
- “Hearing Aid in Mannequin.jpg” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Ear Science Institute Australia. (2017, May 1). Hearing loss simulator - Hear what hearing loss sounds like [Video]. YouTube. All rights reserved. https://youtu.be/_jpe0_v2nAc ↵
- “I Need Help” and “Places I Want to Go” by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- TED-Ed. (2016, September 15). Aphasia: The disorder that makes you lose your words - Susan Wortman-Jutt [Video]. YouTube. All rights reserved. https://youtu.be/-GsVhbmecJA ↵
The ability to determine distance between oneself and another object.
A clouding of the clear lens of the eye.
A visual condition caused by elevated pressure on the optic nerve, resulting in loss of peripheral vision, blind spots, or even blindness across the entire visual field.
Visual condition that results in a blind spot in an individual’s center field of vision.
A common tool for assessing distant vision.
Hearing loss that occurs as a natural part of aging.
A speech disorder where a person understands what other people say but struggles to form words.
A speech condition that causes difficulty in understanding conversations.

