11.2 Cardiovascular System
The cardiovascular system consists of the heart, blood, and blood vessels. (See Figure 11.1.[1]) The heart pumps the blood through the blood vessels. Blood can be viewed as the transportation fluid that transports nutrients to cells and carries wastes away from cells.[2]
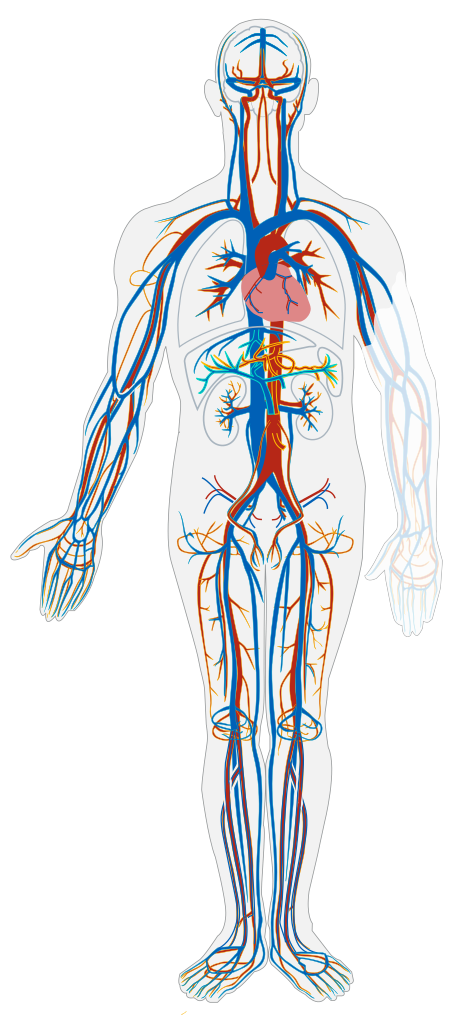
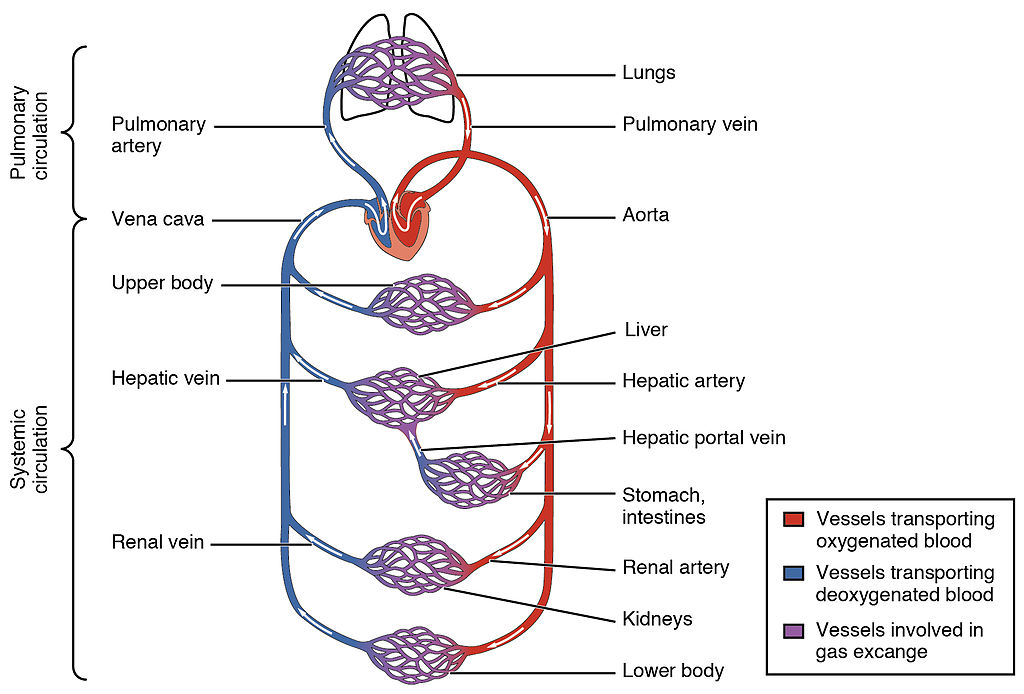
The transportation route to all tissues is an intricate blood vessel network composed of arteries, veins, and capillaries. See Figure 11.2[3] for an illustration of the blood vessel network. The transportation of nutrients begins in the small intestine where they are absorbed and then transported to the liver through the hepatic portal vein. From the liver, nutrients travel in the blood up to the inferior vena cava blood vessel to the heart. The heart pumps the nutrient-rich blood to the lungs to pick up oxygen. The oxygenated blood returns to the heart, where it is pumped out to tissues in the body through the aorta and the arteries. Arteries become smaller and smaller on their way to cells, so that by the time blood reaches a cell, the vessel’s diameter is extremely small, and it is now called a capillary. This reduced diameter of capillaries slows the speed of blood flow and gives cells time to harvest the nutrients and oxygen in the blood and return metabolic wastes to the capillary to be eliminated. Deoxygenated blood containing metabolic wastes is transported back to the heart via veins, and wastes are filtered out by the kidneys and liver.[4]
As the body ages, the strength and elasticity of the heart and blood vessels decrease, resulting in a decreased ability to regulate blood pressure, distribute oxygen, and remove wastes from the body. These changes can lead to dizziness (and a higher fall risk), fluid retention, edema, fatigue, and decreased stamina to complete daily functions.
In addition to these age-related changes, a diet high in saturated fats causes plaque to be deposited on the walls of the blood vessels, causing further narrowing and decreased blood flow. This decrease in circulation increases the risk for blood clots, heart attacks, and strokes.
Because the cardiovascular system is vital for health, any symptoms related to chest pain, shortness of breath, or lack of oxygenation should be immediately reported to the nurse. Cyanosis is a common cardiovascular symptom that refers to bluish discoloration around the mouth and in the extremities (i.e., feet and hands). It occurs when there is decreased oxygenated blood flow to the tissues and should be immediately reported to the nurse. Common nursing assistant interventions for all cardiovascular conditions include encouraging activity as tolerated; promoting a low fat, low cholesterol diet; motivating individuals to quit smoking; and helping individuals make healthy food choices to maintain a healthy weight. Table 11.2 describes symptoms of common cardiovascular diagnoses and related nursing assistant interventions.
Table 11.2 Common Chronic Cardiovascular Diagnoses and Related Nursing Assistant Interventions[5],[6],[7],[8],[9]
| Diagnosis | Definition | Symptoms to Report | Specific Interventions |
|---|---|---|---|
| Heart Failure (HF) | Heart muscle becomes weakened and is unable to adequately pump oxygenated, nutrient-rich blood to the tissues. | Increasing edema, shortness of breath, cyanosis, or rapid weight gain (i.e., more than 2 -3 pounds in 24 hours). |
|
| Hypertension (HTN) or High Blood Pressure | Increased pressure of blood flow against the arteries. HTN is often called the “silent killer” because there are few recognizable symptoms. | Dizziness and/or headache. |
|
| Atrial Fibrillation | Irregular heart rhythm that can cause decreased blood pressure, blood clots, and strokes. | Fatigue, dizziness, chest pain, shortness of breath, and/or palpitations. |
|
| Coronary Artery Disease (CAD) | Cholesterol deposits (plaque) in the heart and arteries cause decreased oxygenated blood flow. | Signs and symptoms occur when the heart muscle doesn’t get enough oxygen-rich blood, causing chest pain and shortness of breath. A complete blockage can cause a heart attack. |
|
| Deep Vein Thrombosis (DVT) | A DVT is a blood clot in a deep vein, typically occurring in the legs.
DVT can be serious because blood clots in the veins can break loose and travel through the bloodstream and get stuck in the lungs, called a pulmonary embolism (PE). PEs block oxygenated blood flow and are life-threatening. |
Unilateral leg swelling, redness, warmth, and/or tenderness or calf cramping. |
|
- “Circulatory_System_no_tags.png” by LadyofHats is in the Public Domain ↵
- This work is a derivative of Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and is licensed under CC BY NC SA 4.0 ↵
- “2101_Blood_Flow_Through_the_Heart.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and is licensed under CC BY NC SA 4.0 ↵
- Mayo Clinic Staff. (2021, October 19). Atrial fibrillation. https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/diagnosis-treatment/drc-20350630 ↵
- Mayo Clinic Staff. (2021, December 10). Heart failure. https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142 ↵
- Mayo Clinic Staff. (2021, July 1). High blood pressure (hypertension). https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410 ↵
- Mayo Clinic Staff. (2022, May 25). Coronary artery disease. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613 ↵
- Mayo Clinic Staff. (2022, June 11). Deep vein thrombosis (DVT). https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557/. ↵
Blue coloration around the mouth and in the extremities (i.e., feet and hands) that occurs when there is decreased oxygenated blood flow to the tissues.

