5.5 Skin Care
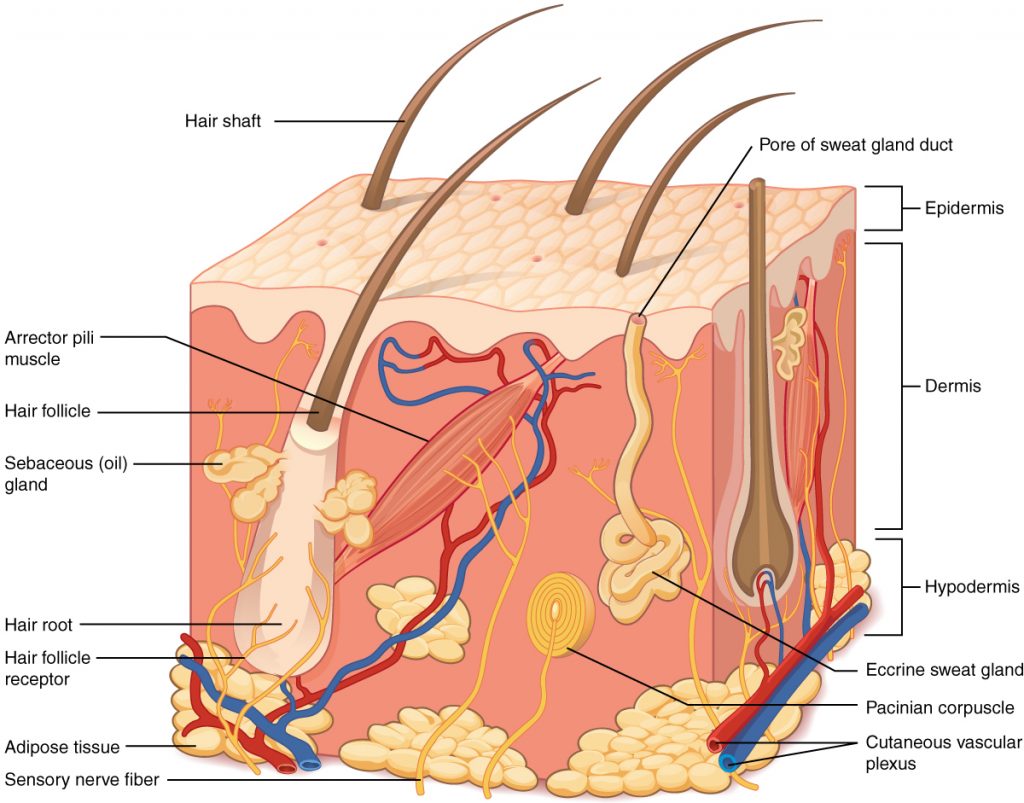
Skin is made up of three layers: epidermis, dermis, and hypodermis. See Figure 5.2[1] for an illustration of skin layers. The epidermis is the thin, topmost layer of the skin. It contains sweat gland duct openings and the visible part of hair known as the hair shaft. Underneath the epidermis lies the dermis where many essential components of skin function are located. The dermis contains hair follicles (the roots of hair shafts), sebaceous oil glands, blood vessels, endocrine sweat glands, and nerve endings. The bottommost layer of skin is the hypodermis (also referred to as the subcutaneous layer). It mostly consists of adipose tissue (fat), along with some blood vessels and nerve endings. Beneath the hypodermis layer lie bone, muscle, ligaments, and tendons.[2]
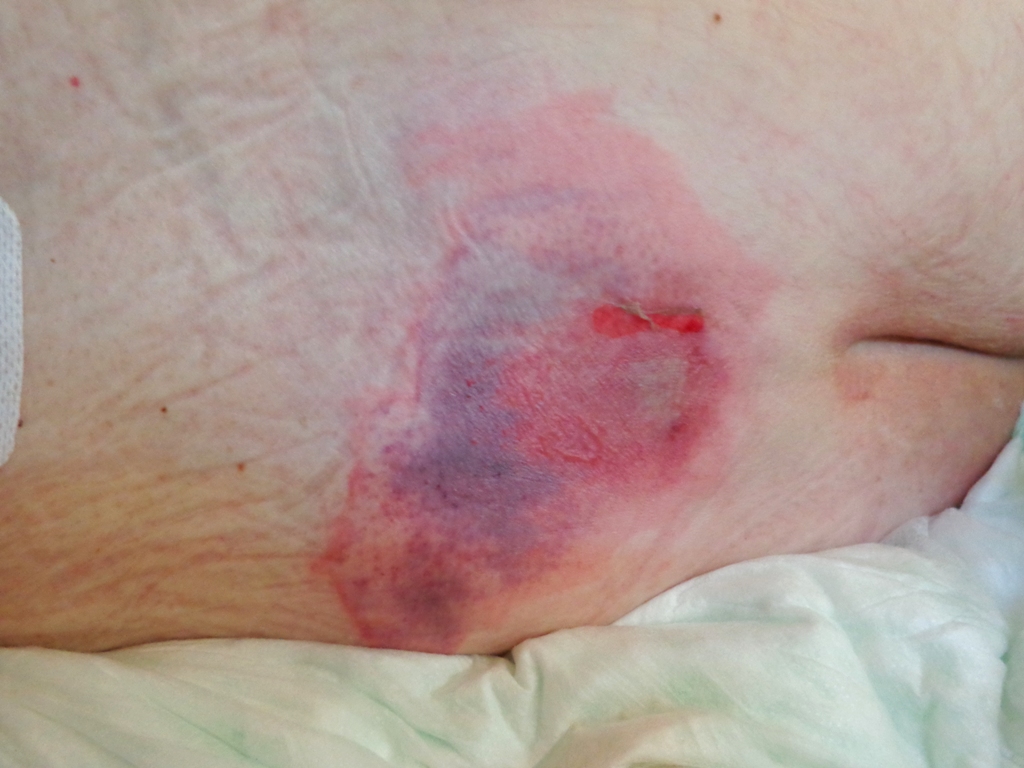
As discussed in Chapter 4, the skin is the body’s first layer of defense against pathogens entering the body. Maintaining healthy skin is an integral responsibility of the nursing assistant. Nursing assistants provide the vast majority of bathing and are able to observe and report any changes to skin integrity while performing ADLs on a daily basis. Impaired skin integrity refers to skin that is damaged or not healing normally. An example of impaired skin integrity is a pressure injury (also called a bedsore or pressure ulcer) with damage to the skin and surrounding tissue. See Figure 5.3[3] for an image of a pressure injury on a client’s lower back above their buttocks.
Age-Related Changes in the Skin
Several changes occur in the skin as one ages. As people age, the amount of adipose tissue decreases. Adipose tissue (i.e., body fat) provides insulation to keep one warm, as well as protection against injury by cushioning underlying structures. See Figure 5.4[4] for an image of age-related changes in the skin on the hand of an older adult.

Oil glands are less productive, making skin drier and more susceptible to cracking. Dry skin and cracked skin make older adults more susceptible to injuries, like skin tears and pressure injuries, that create openings for pathogens and increase the risk of infection. NAs can encourage good nutrition and hydration to help maintain good skin integrity.
Older residents also have reduced production of sweat, which affects the ability of their body to regulate their temperature. This makes them more susceptible to heat-related illness such as exhaustion and heat stroke, especially when being physically active in the heat.[5]
Skin Care Needs of Older Adults
Due to less oil and sweat production as one ages, daily showering or full body bathing is not necessary and can even be damaging to skin. Additionally, residents in long-term care settings don’t typically venture out into the community regularly, thus reducing their exposure to pathogens. Due to these factors, daily partial baths are provided to maintain hygiene, but full body bathing is typically performed only weekly.
It is important to adequately dry skin folds and moisturize the skin regularly to maintain skin integrity and prevent dryness, cracking, and infection. Additionally, clients who are immobile should be repositioned at least every two hours to reduce the risk of pressure injuries. Repositioning techniques can be found in Chapter 8.
Chronic Conditions Affecting Skin Integrity
Skin needs oxygen and nutrients carried in blood to stay healthy. Any condition that impairs blood flow will increase the risk of skin conditions. As a person ages, a general decline in cardiac function decreases blood flow and oxygen to the skin, putting all older adults at increased risk for skin breakdown. Common medical disorders affecting skin health include high cholesterol that causes blockages of blood flow in the arteries, heart failure, high blood pressure, and diabetes.
Clients with diabetes are prone to developing wounds on their feet that can quickly become infected and require amputation. See Figure 5.5[6] for an image of wounds on the foot of a client with diabetes. Nursing assistants should carefully observe the client’s feet and in between their toes daily and report any concerns to the nurse to preserve skin integrity. Nail care for diabetics should be performed by the Registered Nurse (RN) due to the increased risk of infection.

Skin care is important for all clients, but additional moisturizing and frequent repositioning should be performed for clients with increased risk for skin breakdown. See Chapter 8 and 11 for more specific information on risks for skin breakdown and maintaining skin integrity.
- “501 Structure of the skin.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/5-1-layers-of-the-skin ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- “Decubitus 01.jpg” by AfroBrazilian is licensed under CC BY-SA 3.0 ↵
- “hands-578918_1280.jpg” by Gaertringen on Pixabay.com is licensed under CC0 ↵
- Balmain, B. N., Sabapathy, S., Louis, M., & Morris, N. R. (2018). Aging and thermoregulatory control: The clinical implications of exercising under heat stress in older individuals. BioMed Research International, 2018, 8306154. https://doi.org/10.1155/2018/8306154 ↵
- “Two_ischaemic_ulcers_on_the_foot_of_an_individual_with_type_2_diabetes.jpg” by Bondegezou is licensed under CC BY-SA 4.0 ↵
Skin that is damaged or not healing normally.

