9.6 Promoting Independence During ADLs
As a health care professional, it is your responsibility to maintain residents’ optimal levels of functioning by encouraging their participation and independence in completing activities of daily living (ADLs). While it may be quicker and more efficient to wheel someone to the dining room rather than assisting them to walk there, it is detrimental to their health to do so. As previously discussed in the “Complications of Immobility” section of this chapter, many interventions prevent decline in residents’ functioning, including encouraging activity as tolerated, and promote independence in completing ADLs with segmenting as needed. Independence in completing ADLs not only prevents complications of immobility but also enhances their quality of life by promoting mental wellness through enhancement of their autonomy and self-esteem.
However, some clients may prefer others to completely care for them because the movements are painful or involve more effort than they are willing to exert. As you gain more experience as a nursing assistant, you will learn to find the delicate balance between promoting health and following client preferences.
Always encourage clients to complete as many ADLs as they can, segmenting them if needed. When you notice a client is becoming fatigued or irritable when performing a task, it is often a good time to begin assisting the client. It does not matter how little a person is able to do for themselves; they should be given the time and opportunity to do so. For nonverbal clients, consider using a white board, communication book, or other device to assist in their communication. These actions demonstrate respect for the person’s dignity, as well as promote their physical health and cognitive involvement in their own care. Refer to the Chapter 8.3, “Promoting Joint Mobility and Activity” section for other ways to encourage mobility and independence.
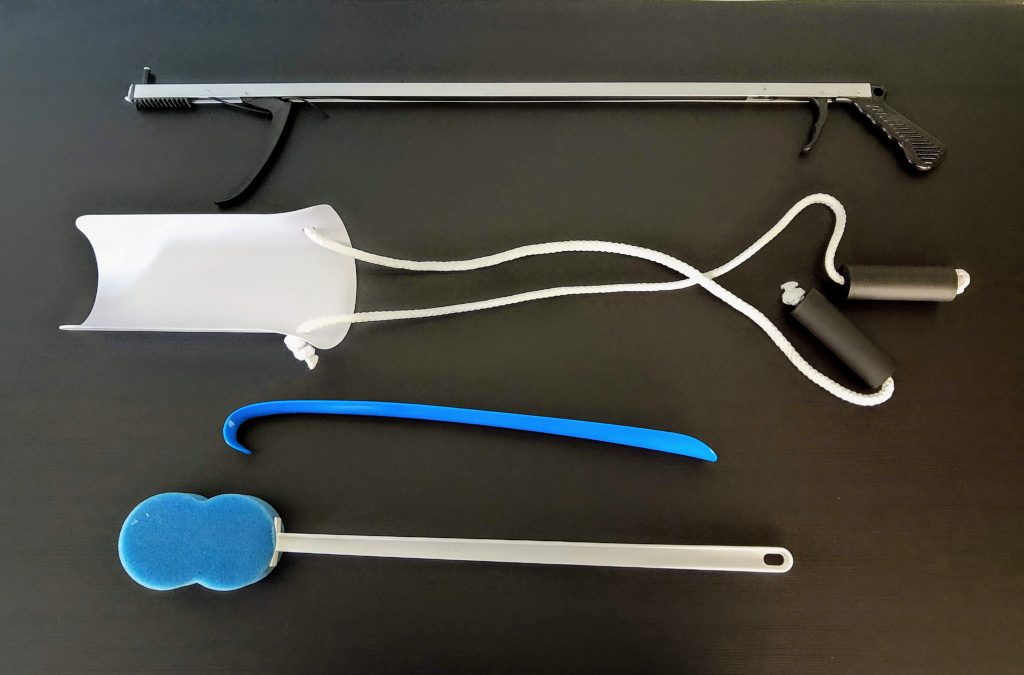
The therapy team will assess the client and recommend aids that can promote independence to complete daily tasks. Common aids for ADLs may include a reacher, sock aid, bath sponge, and an elongated shoehorn. All these tools allow a person to reach objects or complete hygiene needs with less bending or stretching. They may be used temporarily during the rehabilitation process until full ROM is achieved, especially after joint replacement surgeries. See Figure 9.10[1] for an image of these assistive devices.
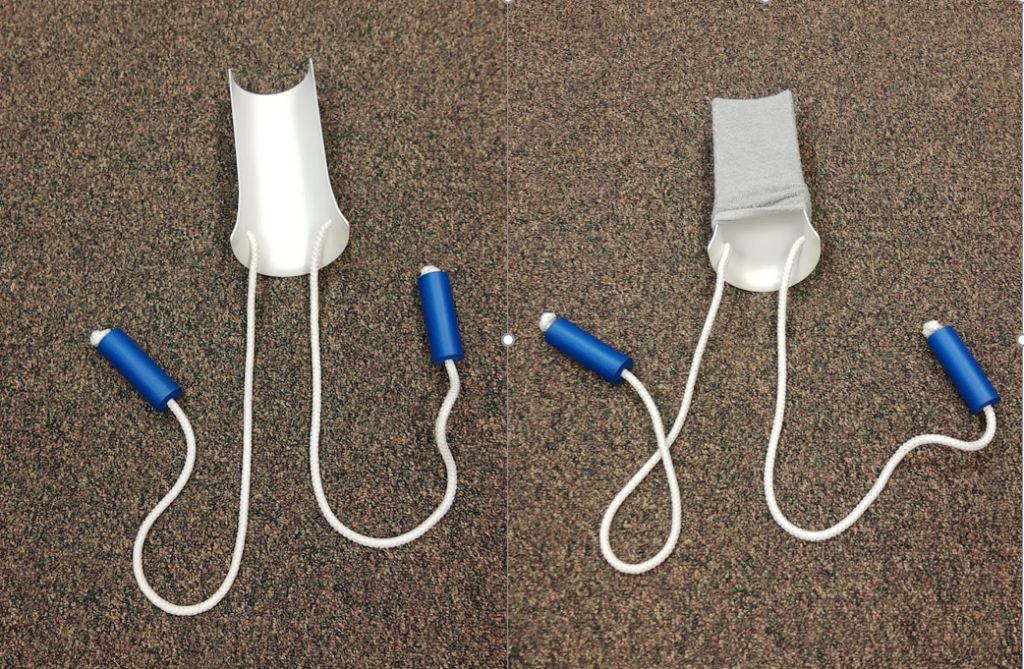
Sock Aid
To utilize the sock aid, the sock is placed around the plastic mold. The person holds the rope handles and then puts their foot into the sock. They pull on the ropes to get the sock completely on the foot without bending over to the floor. See Figure 9.11[2] for an image of the placement of a sock on a sock aid and Figure 9.12[3] for an image of getting the sock on the foot.

Please also review assistive devices to promote independence with feeding in “Assistance With Nutrition and Fluid Needs.”
- “ADL Aids” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Sock Aid.jpg" by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Applying Sock Aid.png” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵

