11.4 Endocrine System
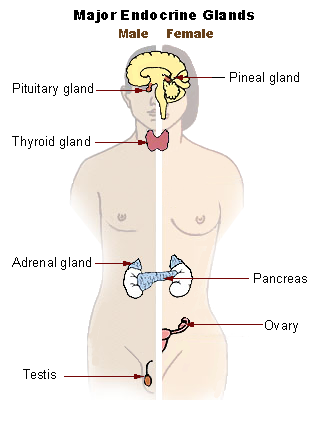
Endocrine glands secrete hormones that affect the functioning of other organs throughout the body and are transported by the circulatory system. The glands in the endocrine system are the pituitary, thyroid, parathyroid, adrenals, thymus, pineal, pancreas, ovaries, and testes, as seen in Figure 11.7.[1]
The functions of the endocrine system are connected to an individual’s nutrition. The endocrine system is responsible for regulating appetite, nutrient absorption, nutrient storage, and nutrient usage, as well as contributing to other body functions such as reproduction. The most notable connection between nutrition and the functions of the endocrine system is how unhealthy dietary patterns are linked to obesity and the development of diabetes.[2]
The pancreas is an endocrine gland that makes insulin, the hormone that allows cells to use glucose for energy. Insulin is released after an individual eats a meal based on the amount of calories they consumed. The function of the pancreas is affected by a medical condition called diabetes. The Centers for Disease Control and Prevention (CDC) estimates that 11 percent of the U.S. population has diabetes, and 49 percent of adults over age 65 have prediabetes.[3]
See maps of diabetes and obesity by county at CDC’s Diabetes and Obesity Maps web page.
In type 1 diabetes, the pancreas becomes unable to make insulin. In type 2 diabetes, obesity causes changes in muscle, fat, and liver cells that leads to their diminished response to insulin, referred to as “insulin-resistance.” When cells are resistant to insulin, they do not take in enough glucose to make energy, resulting in high levels of glucose in the blood. Chronically elevated blood glucose damages other tissues over time, increasing the individual’s risk for cardiovascular disease, kidney disease, nerve damage, and eye disease. The nerve damage causes pain and numbness in the feet and lower legs that can increase risk for falls.[4]
Individuals with diabetes must frequently measure their blood glucose level to keep it in normal range with medications prescribed by their health care provider. Blood glucose levels are typically checked in individuals with diabetes from one to four times per day. This measurement is typically performed by the nurse, but some states allow nursing assistants to receive additional training to complete this procedure.
People with diabetes are typically prescribed oral medications or injectable insulin to keep their blood glucose in a healthy range. Too much or not enough insulin can cause life-threatening reactions so it must be administered cautiously. In hospitals and long-term care centers, insulin is administered by a nurse.
Too much insulin or not enough carbohydrate intake results in very low blood sugar (referred to as hypoglycemia) that can cause a coma if it is not quickly addressed. Nursing assistants must observe for signs of low blood sugar in clients with diabetes and immediately report them to the nurse for follow-up. Signs of low blood sugar include confusion, irritability, shakiness, cold and clammy skin, sweating, hunger, and anxiety.[5]
When not enough insulin or other diabetic medications are administered for the amount of carbohydrates an individual consumes, blood glucose levels become elevated (i.e., hyperglycemia). Symptoms of elevated blood glucose include increased urination; increased thirst and hunger; a fruity breath odor; warm, dry skin; and fast, deep breathing. These symptoms should be immediately reported to the nurse.[6]
Because nutritional intake affects an individual’s blood glucose, nursing assistants play a helpful role in encouraging healthy diet choices for individuals with diabetes. Encourage clients to avoid eating refined sugar and highly processed foods and increase their intake of whole grains and non-starchy vegetables such as broccoli, spinach, and green beans. Encouraging residents to be as active as possible can also help manage their blood glucose levels.[7]
If neuropathy occurs, the individual’s skin should be diligently inspected daily, especially on the bottoms of their feet and in between their toes. Well-fitted shoes should be worn, and socks should be carefully placed so the seams do not cause irritation. Individuals with neuropathy do not feel skin irritations or open areas, and they can become infected quickly. If left untreated, severe infection can lead to amputation. Due to these risks, nursing assistants should not trim the nails of diabetic patients.
- “llu_endocrine_system_New.png” by US Government is in the Public Domain ↵
- This work is a derivative of Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and is licensed under CC BY NC SA 4.0 ↵
- Centers for Disease Control and Prevention. (2022, March 9). Diabetes data and statistics. https://www.cdc.gov ↵
- This work is a derivative of Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and is licensed under CC BY NC SA 4.0 ↵
- Centers for Disease Control and Prevention. (2022, June 1). Diabetes. https://www.cdc.gov/diabetes/index.html ↵
- Centers for Disease Control and Prevention. (2022, June 1). Diabetes. https://www.cdc.gov/diabetes/index.html ↵
- Centers for Disease Control and Prevention. (2022, June 1). Diabetes. https://www.cdc.gov/diabetes/index.html ↵
Low blood sugar.
Elevated blood glucose levels.

