5.8 Assistance With Toileting
Just as there are several bathing techniques based on a resident’s functioning and mobility, there are multiple methods for assisting residents with their bladder and bowel elimination. Regardless of the method used, residents should be offered toileting assistance at least every two hours. The following subsections provide an overview of each toileting method and when it may be implemented.
Toilet
The resident should be able to stand independently, walk, or pivot transfer with assistance. A mechanical lift that assists with bearing weight may also be used to place a resident on the toilet.
Bedpan
Bedpans are used for residents who cannot bear weight or prefer to stay in bed, such as when having to urinate during the night. Residents who require a full body lift to transfer typically require the use of a bedpan, but there are also toileting slings to assist a fully dependent resident to use a toilet or commode. See Figure 5.17[1] for an image of two types of bedpans. The image on the left is a standard bedpan and the image on the right is called a fracture pan. Fracture bedpans are smaller than standard bedpans and have one flat end. They are designed for individuals recovering from a hip fracture or hip replacement.
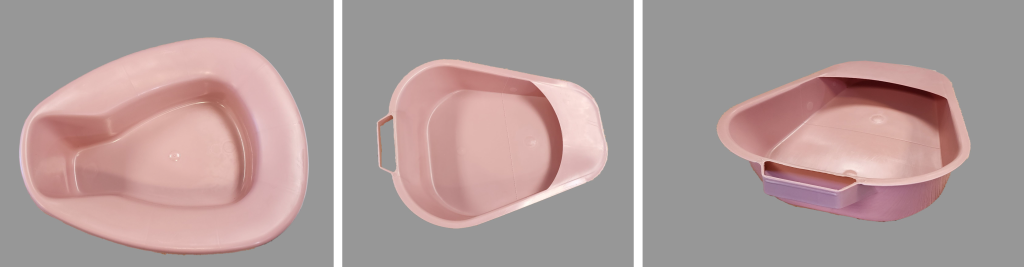
For residents with strong hip mobility who require a bedpan, ask them to bend their knees and push their hips upwards. While they are raised, place a barrier (e.g., a towel, waterproof soaker pad, disposable pad, etc.) under them and then place a standard bedpan underneath their buttocks. Ensure the handle of the fracture pan (or the opening of the rim on a full bedpan) is pointed towards the foot of the bed before they lower themselves onto the bedpan. For residents with limited hip mobility, use their lift sheet to roll them away from you towards a raised side rail. While they are lying on their side and holding the side rail, return the lift sheet on top of the bed and then place a barrier on top of the lift sheet. Place a fracture pan behind the resident’s buttocks and then gently roll both the resident and the fracture pan back to the bed surface, ensuring proper placement of the pan.
Please see Skills Checklist for additional information.
Commode
A commode looks like a toilet, but it is a movable device with a bucket underneath the seat. See Figure 5.18[2] for an image of a commode. Commodes are typically placed near the bed for residents who have limited weight-bearing ability, do not want to share a bathroom with another resident, or have urge incontinence. Urge incontinence means that as soon as the person feels the need to empty their bladder, they have very little time before urine escapes.

Incontinence Briefs or Pads
Incontinence briefs or pads are disposable products used for residents who have little to no control over bladder or bowel function and are worn in, or in place of, their underwear. Please see Skills Checklist for additional information.
Urinary Catheter
A urinary catheter is a device placed into the bladder by a nurse using sterile technique that allows the urine to drain into a collection bag. Urinary catheters are used sparingly due to increased risk of urinary tract infections. Catheters are typically used for clients with urinary retention, have a wound near the perineal area that may become infected due to incontinence, or have a neurological condition that does not allow them to control their bladder function. See Figure 5.19[3] for an illustration of an indwelling urinary catheter attached to a collection bag. Nursing assistants may assist in emptying/documenting urine output from the collection bag or providing catheter care according to agency policy. Please see 5.25 Skills Checklist for additional information.

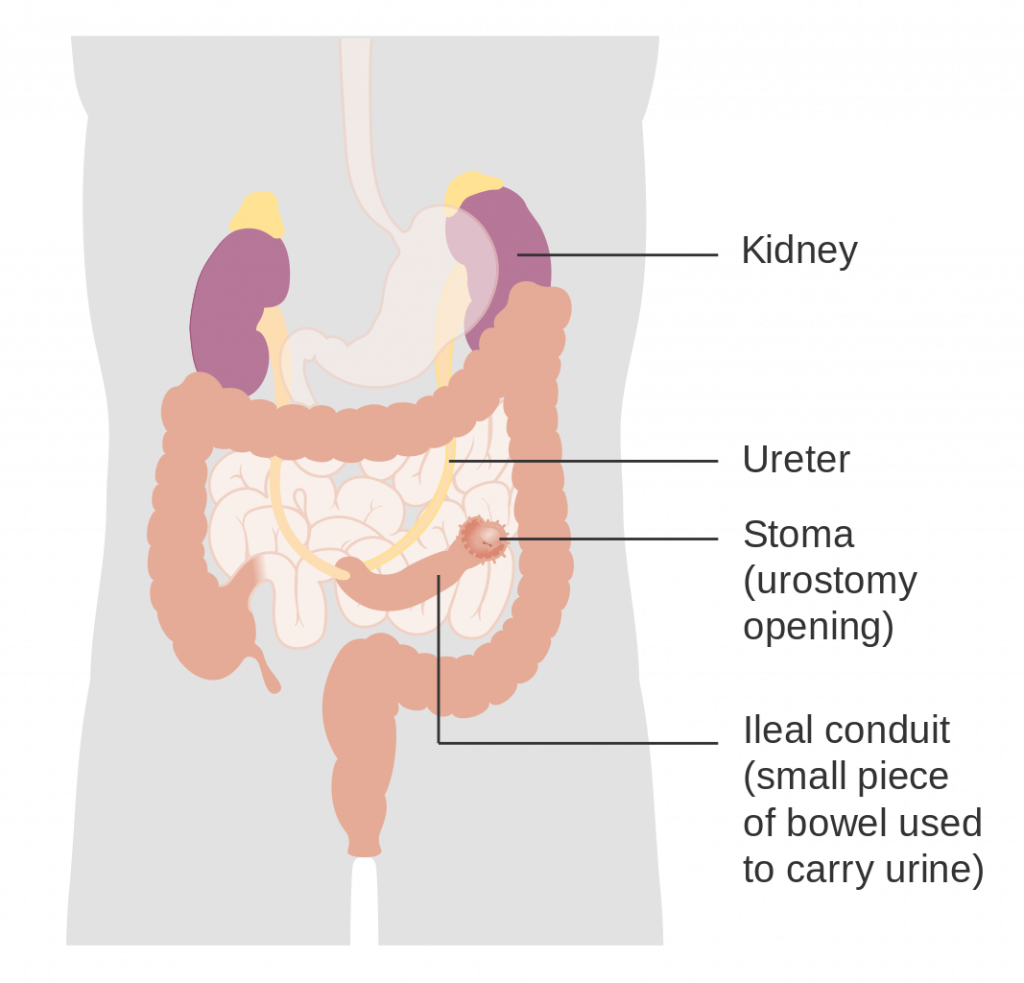
Urostomy
A urostomy is placed surgically to collect urine from the ureters when the bladder is diseased or has been removed. Urostomies are typically located on the lower right side of the abdomen, and urine is collected into a drainage bag. See Figure 5.20[4] for an illustration of a urostomy.
Colostomy
A colostomy is placed surgically when colon function is impaired. A piece of the colon is diverted to an artificial opening in the abdominal wall called a stoma, and feces is collected in a pouch.
Considerations When Assisting Clients With Toileting
Nursing assistants must consider a resident’s privacy and dignity when assisting with toileting just as they do with bathing. Most residents prefer to be alone when urinating or defecating. Privacy can be provided by closing the bathroom door if the resident is able to be left alone. If the resident is not safe to be left alone, close the door as much as possible while keeping the resident within eyesight. Maintain awareness of a resident who is toileting or on the bedpan so they do not need to wait for assistance with perineal care after elimination and will not develop any skin issues from sitting on a hard surface.
To maintain dignity, nurse aides should be careful when explaining and providing care related to toileting. For example, a disposable brief should never be referred to as a diaper; acceptable terms include a brief, pad, liner, or disposable underwear. Additionally, a nurse aide should never show reluctance or appear burdened when providing toileting assistance, no matter how often a resident feels the need to be toileted or requires perineal care due to incontinence.
Bladder and Bowel Retraining
Clients who are dependent on others for assistance with elimination should be taken to the bathroom or offered toileting options every two hours. Incontinence is a very personal matter and can be embarrassing for clients. Nursing assistants should use therapeutic communication when assisting clients with toileting.
When indicated, clients may undergo bladder and bowel retraining to regain control of elimination. There are several strategies used to promote bladder continence. The nurse aide may assist the nurse with one of the strategies called timed voiding. Timed voiding encourages the patient to urinate on a set schedule, such as every hour, whether they feel the urge to urinate or not. The time between bathroom trips is gradually extended with the general goal of achieving four hours between voiding. Timed voiding helps to control urge and overflow incontinence as the brain is trained to be less sensitive to the sensation of the bladder walls expanding as they fill.[5]
Bowel retraining involves teaching the body to have a bowel movement at a certain time of the day. This training includes encouraging clients to go to the bathroom when feeling the urge to do so and not ignoring the urge. For some individuals, it is helpful to schedule this consistent time in the morning when the natural urge occurs after drinking warm fluids or eating breakfast. For other people, especially those with a neurological cause, a laxative may be scheduled regularly to stimulate the urge to have a bowel movement on a regular basis and prevent constipation. The nurse should communicate to the nursing assistant when bowel retraining is in place, or a laxative is administered to a client so they are aware of the client’s need to defecate.[6]
Urinary Tract Infection (UTI)[7]
A urinary tract infection (UTI) is a common infection that occurs when bacteria, typically from the rectum, enter the urethra and infect the bladder or kidneys. Infections can affect several parts of the urinary tract, but the most common type is a bladder infection. Kidney infections are more serious than a bladder infection because they can have long-lasting effects on the kidneys.
Some people are at higher risk of getting a UTI. UTIs are more common in females because their urethras are shorter and closer to the rectum, which makes it easier for bacteria to enter the urinary tract. Providing improper perineal care is a common cause of a UTI. Nursing assistants must be diligent and assist with perineal hygiene as needed to prevent infections. Other factors that can increase the risk of UTIs include the following:
- A previous UTI
- Sexual activity, especially with a new sexual partner
- Pregnancy
- Age (Older adults and young children are at higher risk)
- Urinary retention
- Low fluid intake
- Structural problems in the urinary tract, such as prostate enlargement
Symptoms of a UTI should be reported to the nurse immediately and include the following:
- Pain or burning while urinating (dysuria)
- Frequent urination (frequency)
- Urgency with small amounts of urine
- Bloody urine
- Pressure or cramping in the groin or lower abdomen
- Confusion or altered mental status in older adults
Symptoms of a more serious kidney infection (called pyelonephritis) include fever above 101 degrees F (38.3 degrees C), shaking chills, lower back pain or flank pain (i.e., on the sides of the back), and nausea or vomiting.
It is important to remember that older adults with a UTI may not exhibit these common symptoms but instead demonstrate an increased level of confusion. Older adults often become weaker when they have a UTI and may fall. If you notice increased weakness or a change in the level of confusion in an older client, report these symptoms to the nurse immediately. If not treated quickly, UTIs can spread to the blood (called septicemia), leading to life-threatening infection called sepsis.
When a patient has symptoms related to a possible UTI, the health care provider will order diagnostic tests, such as a urine dip, urinalysis, or urine culture. See the subsection below on “Specimen Collection,” which details how nursing aides assist with these tests. Antibiotics are prescribed for urinary tract infections and are administered by the nurse. Nursing assistants should encourage clients with UTIs to drink extra fluids to help flush bacteria from the urinary tract, and toileting should be offered more frequently with proper perineal care.
Observation and Documentation of Urinary Output
When assisting residents with urinary elimination, their urine should be observed for the characteristics described in Table 5.8. Terms used to document these characteristics are included.
Characteristics of urine can be indicative of a urinary tract infection or dehydration and should be reported to the nurse. Dark urine, minimal urine output, or the infrequent need to void can be signs of dehydration. Characteristics of an infection are described in the previous “Urinary Tract Infection (UTI)” subsection. If noted and reported promptly, fluids can be encouraged to help treat these conditions.
Table 5.8 Urine Characteristics
| Characteristic | Normal Observation | Abnormal Observation | Documentation Terminology |
|---|---|---|---|
| Color | Amber (like a stoplight) or straw-colored | Dark amber or possibly root beer or cola-colored | Amber or cola |
| Odor | Acidic | Noticeably stronger odor than usual | Strong |
| Clarity | Clear | Cloudy | Cloudy |
| Sediment | None present | Particles present | Sediment noted |
| Amount | Generally 250-350 cc | More or less than usual amount | Amount in milliliters or cubic centimeters. Minimal amount may be described as scant |
If a resident is regularly incontinent and uses a brief or disposable pad for elimination, the nursing assistant should document the number of times the resident is incontinent rather than recording the amount. For a continent resident, use a toilet hat to measure urine output as described in the “Specimen Collection” subsection below. If the resident uses a commode or bedpan, place a graduated cylinder on a barrier, carefully pour the urine into the graduated cylinder, and observe and document the characteristics. See Figure 5.21[8] for an image of a graduated cylinder.

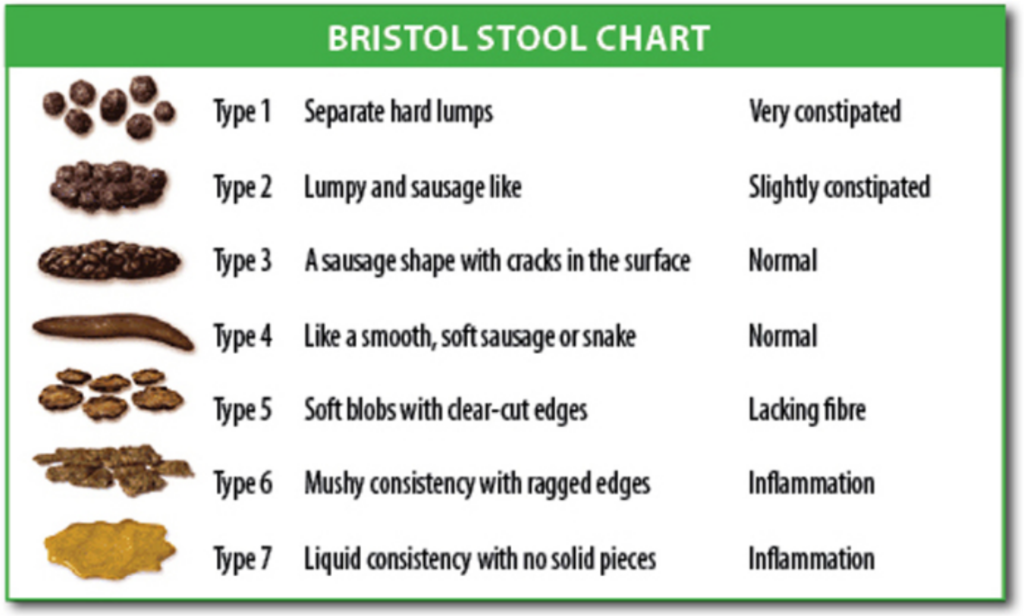
Observation and Documentation of Stool
Similar to urine, stool output and characteristics can indicate underlying health concerns. Risk factors to healthy stool elimination will be discussed further in the “Digestive System” section in Chapter 11, but slowing of the digestive system, decreased intake, and lower mobility can all contribute to constipation and even cause bowel obstruction. Documentation and reporting of unusual characteristics can assist nurses in providing interventions that can prevent more serious health concerns.
Elimination patterns vary for each individual, but a typical range for bowel elimination is twice daily to once every other day. When regular bowel movements do not occur, stool becomes hardened in the colon, making it difficult to push out, especially for those who are physically declined. Stool should be soft and formed when eliminated to prevent additional problems like hemorrhoids. Stool that is loose or liquid may indicate an infection or other chronic intestinal issues.
Nursing assistants should note the size of a client’s bowel movement as “small,” “medium,” or “large” as an estimation. Using agency protocol, the consistency of the stool should also be documented. The Bristol Stool Chart is a common tool used to easily observe and document the consistency of stool. See Figure 5.22[9] for an image of the Bristol Stool Chart. Additionally, if any blood or dark tarry stool is observed, this should be reported immediately to the nurse.
Specimen Collection[10]
Urinary Samples
Urinary samples may need to be collected to detect infection. When needed, obtain a toilet hat (see Figure 5.23“Toilet Hat” and “Commode with Toilet Hat” by Landon Cerny are licensed under CC BY 4.0[/footnote]. Ask the nurse to label a specimen cup before collecting urine (see Figure 5.24[11]).
When assisting in collecting a urine specimen, place the cup and toilet hat on a barrier to prevent contamination with bacteria from the environment. Apply gloves and assist the client when needed to clean around the urethra to remove any external pathogens. If able, ask the resident to void a small amount of urine into the toilet. Place the toilet hat in the front of the toilet and instruct the resident to void into the hat. Do not put toilet paper or any other products into the toilet hat. After urination, assist the resident in completing perineal care and transferring from the toilet. Remove dirty gloves, perform hand hygiene, and apply new gloves to prevent contamination of the urine with bacteria from the perineal area. Pour the urine sample from the toilet hat into the specimen cup and tightly put on its cover. Remove gloves and perform hand hygiene before writing the time of collection on the label. Immediately bring the urine sample to the nurse.


Stool Samples
Stool samples are collected from patients to test for cancer, parasites, or for occult blood (i.e., hidden blood). The Guaiac-Based Fecal Occult Blood Test (gFOBT) is a commonly used test to find hidden blood in the stool that is not visibly apparent. As a screening test for colon cancer, it is typically obtained by the patient in their home using samples from three different bowel movements. Nursing assistants may collect gFOBT specimens for clients.
Before the test, the nurse should verify that the client has avoided red meat for three days and has not taken aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, for seven days prior to the test. (Blood from the meat can cause a false positive test, and aspirin and NSAIDS can cause bleeding, also leading to a false positive result.) Vitamin C (more than 250 mg a day) from supplements, citrus fruits, or citrus juices should be avoided for 3 to 7 days before testing because it can affect the chemicals in the test and make the result negative, even if blood is present.
To perform a gFOBT in an inpatient setting, perform the following steps.
- Verify with the nurse that the client has met dietary and medication requirements.
- Explain the procedure to the client. Assist the resident to a clean, dry commode and instruct them not to put any toilet paper in the commode, as this may alter the test result. Request they use the call light when they have had a bowel movement.
- Review the manufacturer’s instructions with the nurse.
- Label the card with the patient’s name and medical information per agency policy. Open the flap of the guaiac test card.
- Apply nonsterile gloves. Use the applicator stick to apply a thin smear of the stool specimen to one of the squares of filter paper on the card. Obtain a second specimen from a different part of the stool and apply it to the second square of filter paper on the card. (Occult blood isn’t typically equally dispersed throughout the stool.)
- Place the labeled test card in a transport bag.
- Remove gloves and perform hand hygiene.
- Give the transport bag to the nurse to send to the laboratory for analysis.
- “Bedpan.jpg”, "Fracture Bedpan.jpg", and "Fracture Bedpan View 2.jpg" by Landon Cerny are licensed under CC BY 4.0 ↵
- “Bedside Commode” by Landon Cerny is licensed under CC BY 4.0 ↵
- "Foley Catheter with Collection Bag and Leg Strap" by Landon Cerny is licensed under CC BY 4.0 ↵
- “Diagram_showing_how_a_urostomy_is_made_(ileal_conduit)_CRUK_124.svg” by Cancer Research UK is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- "Graduated Cylinder" by Landon Cerny is licensed under CC BY 4.0 ↵
- “Bristol_stool_chart.svg” by Cabot Health, Bristol Stool Chart is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- “Sterile Specimen Container" by Landon Cerny are licensed under CC BY 4.0 ↵
A movable device with a bucket underneath the seat that is used for elimination when the client has difficulty getting to the bathroom.
A condition where as soon as the person feels the need to empty their bladder they have very little time before urine escapes.
Disposable products used for clients with little to no control over bladder or bowel function.
A surgically placed opening to collect urine from a person’s ureters when their bladder is diseased or has been removed.
A surgically placed opening when a client’s colon function is impaired.
Encourages the patient to urinate on a set schedule.
Common infection that occurs when bacteria, typically from the rectum, enter the urethra and infect the bladder or kidneys.
Life-threatening infection that has spread throughout the body.

